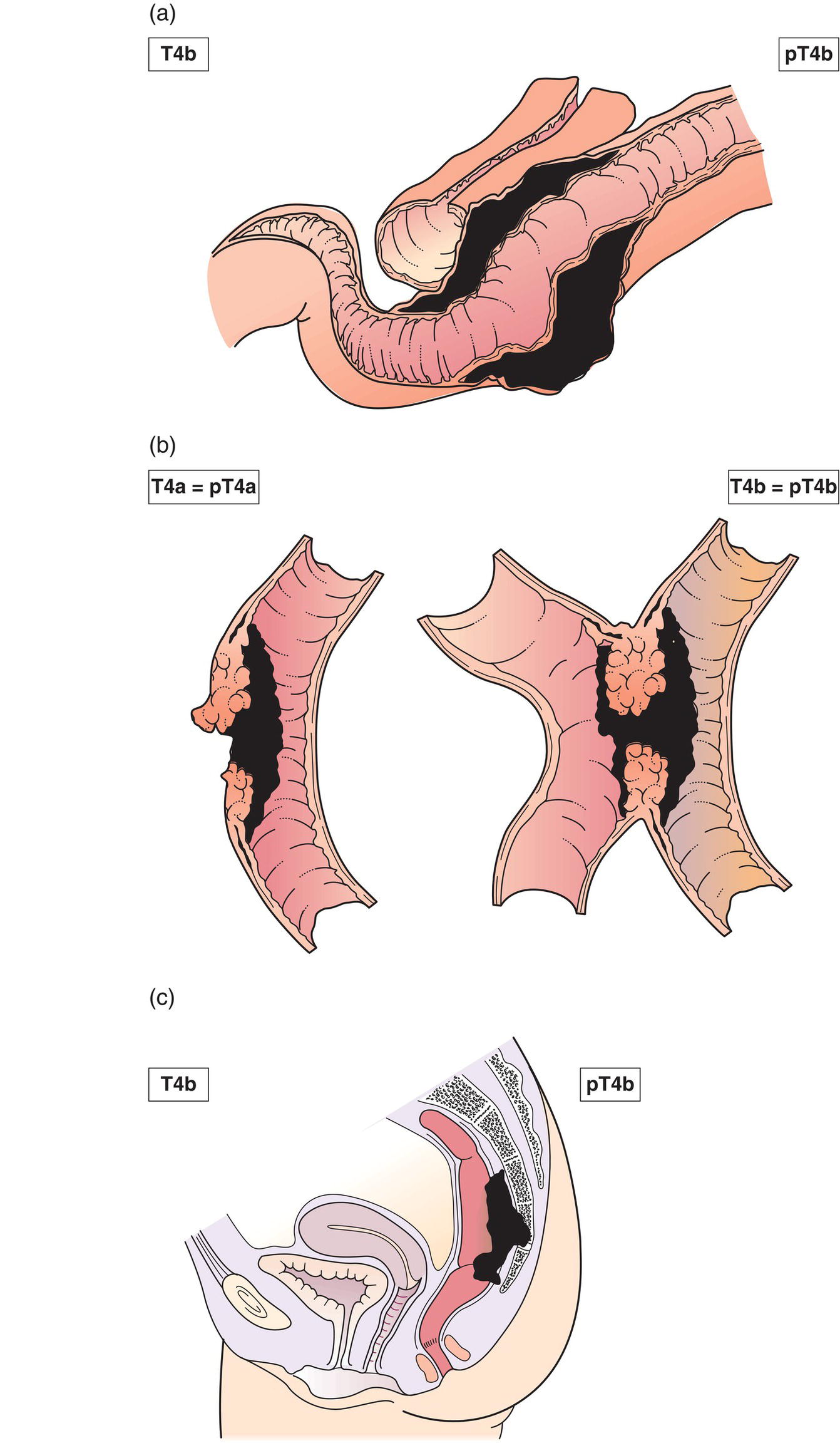
The classification applies only to carcinomas. There should be histological confirmation of the disease. For each anatomical site or subsite, the following are regional lymph nodes: Metastasis in nodes other than those listed above is classified as distant metastasis. Notes 1 Tis includes cancer cells confined within mucosal lamina propria (intramucosal) with no extension through the muscularis mucosae into the submucosa. 2 Invades through to visceral peritoneum to involve the surface. 3 Direct invasion in T4b includes invasion of other organs or segments of the colorectum by way of the serosa, as confirmed on microscopic examination, or for tumours in a retroperitoneal or subperitoneal location, direct invasion of other organs or structures by virtue of extension beyond the muscularis propria. 4 Tumour that is adherent to other organs or structures, macroscopically, is classified as cT4b. However, if no tumour is present in the adhesion, microscopically, the classification should be pT1–3, depending on the anatomical depth of wall invasion. Note * Tumour deposits (satellites) are discrete macroscopic or microscopic nodules of cancer in the pericolorectal adipose tissue’s lymph drainage area of a primary carcinoma that are discontinuous from the primary and without histological evidence of residual lymph node or identifiable vascular or neural structures. If a vessel wall is identifiable on H&E, elastic or other stains, it should be classified as venous invasion (V1/2) or lymphatic invasion (L1). Similarly, if neural structures are identifiable, the lesion should be classified as perineural invasion (Pn1). The presence of tumour deposits does not change the primary tumour T category, but changes the node status (N) to pN1c if all regional lymph nodes are negative on pathological examination. The pT and pN categories correspond to the T and N categories. Note pM0 and pMX are not valid categories.
COLON AND RECTUM (ICD‐O‐3 C18–20)
Rules for Classification
Anatomical Sites and Subsites
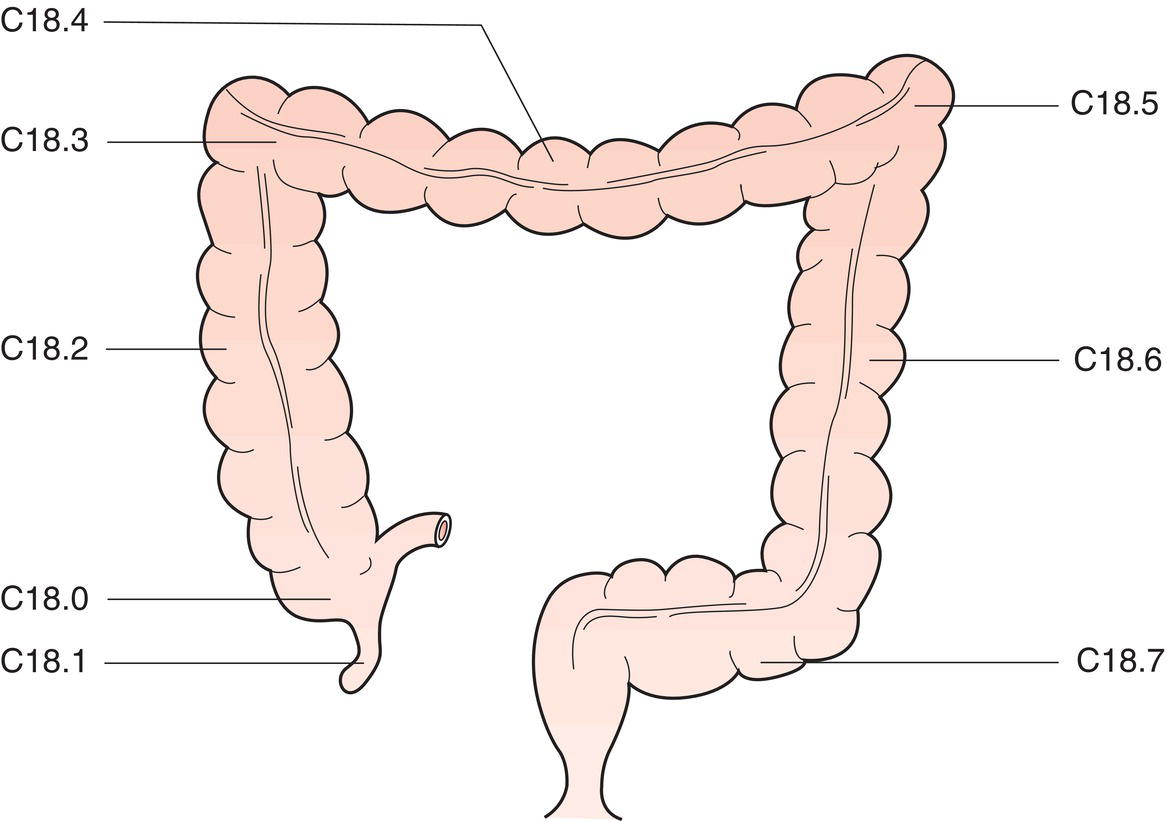
Colon (C18) (Fig. 170)
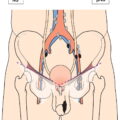
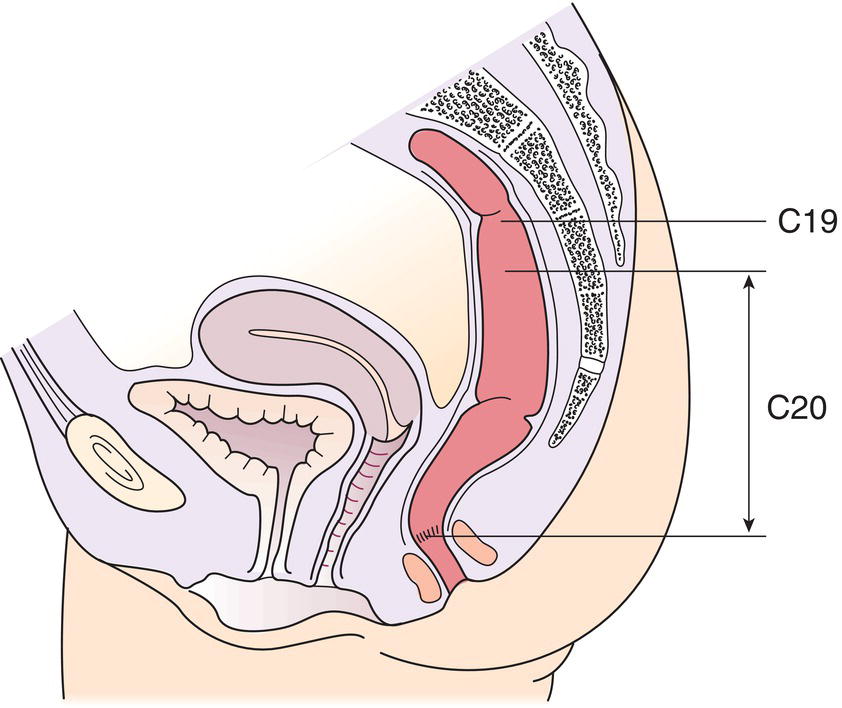
Rectosigmoid junction (C19) (Fig. 171)
Rectum (C20) (Fig. 171)
Regional Lymph Nodes
Caecum
Ileocolic, right colic (Fig. 172)
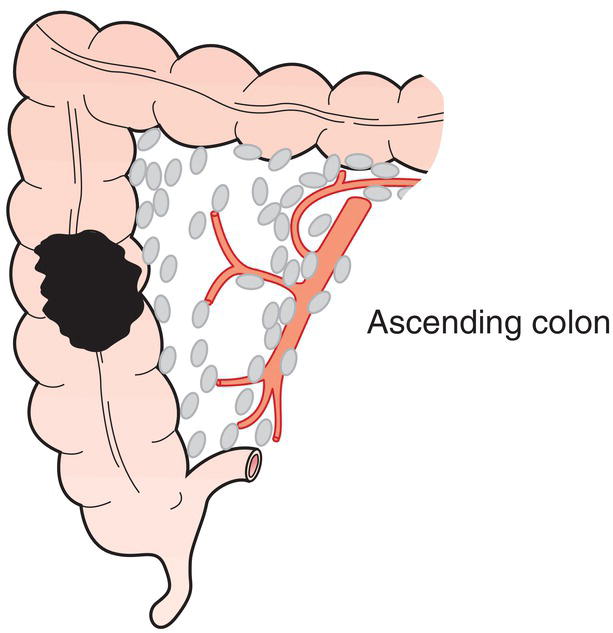
Ascending colon
Ileocolic, right colic, middle colic (Fig. 173)
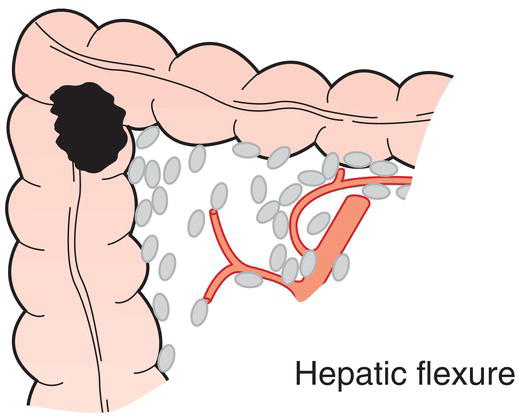
Hepatic flexure
Middle colic, right colic (Fig. 174)
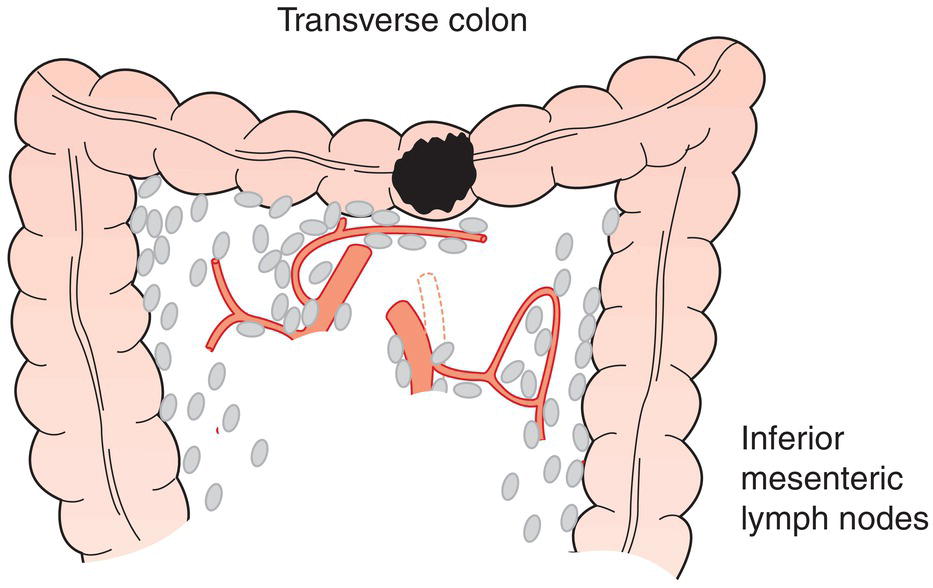
Transverse colon
Right colic, middle colic, left colic, inferior mesenteric (Fig. 175)
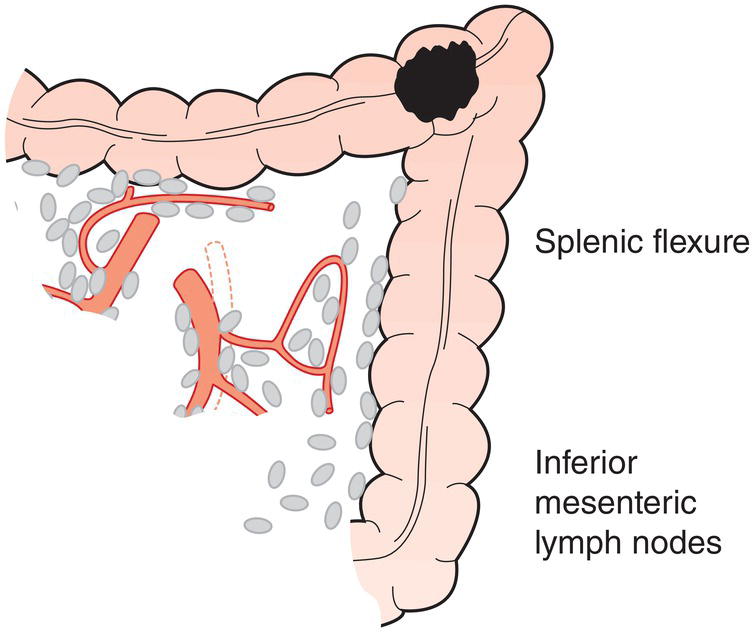
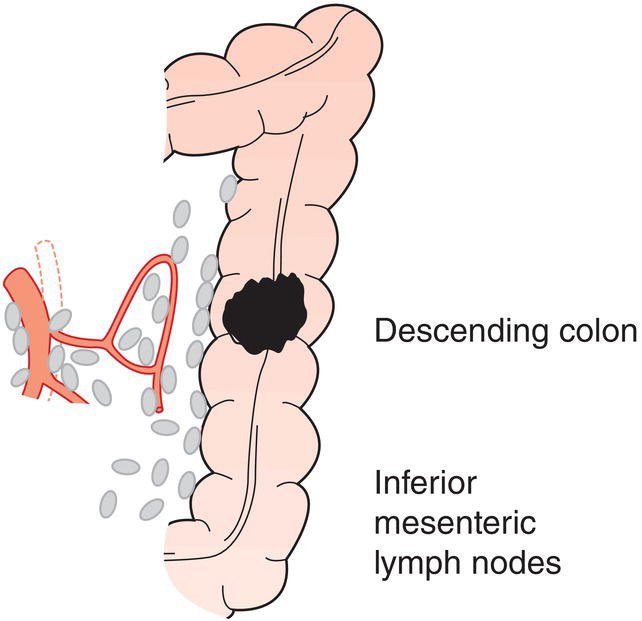
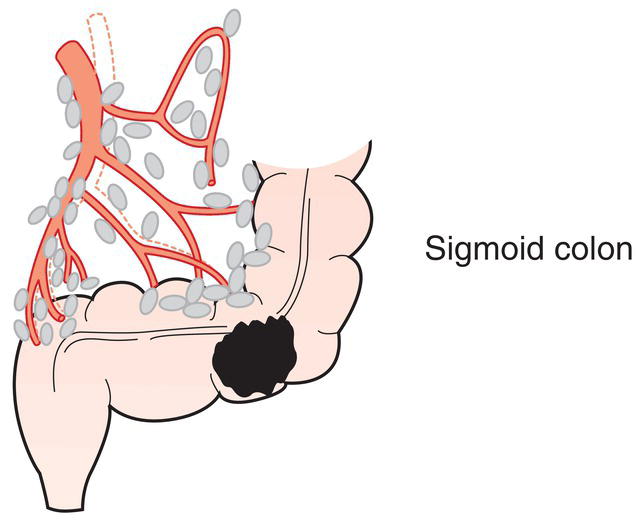
Splenic flexure Descending colon Sigmoid colon
Middle colic, left colic, inferior mesenteric (Fig. 176)
Left colic, inferior mesenteric (Fig. 177)
Sigmoid, left colic, superior rectal (haemorrhoidal), inferior mesenteric and rectosigmoid (Fig. 178)
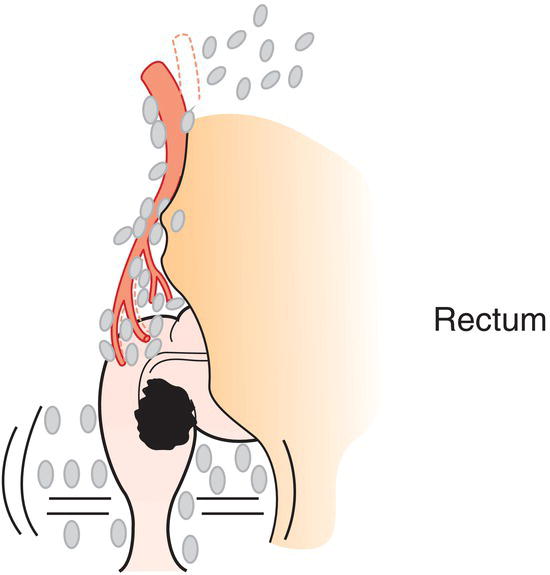
Rectum
Superior, middle, and inferior rectal (haemorrhoidal), inferior mesenteric, internal iliac, mesorectal (paraproctal), lateral sacral, presacral, sacral promontory (Gerota) (Fig. 179) 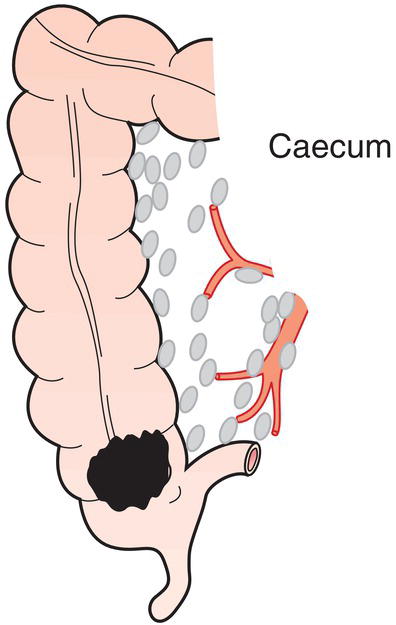
TNM Clinical Classification
T – Primary Tumour
TX
Primary tumour cannot be assessed
T0
No evidence of primary tumour
Tis
Carcinoma in situ: intraepithelial or invasion of lamina propria1
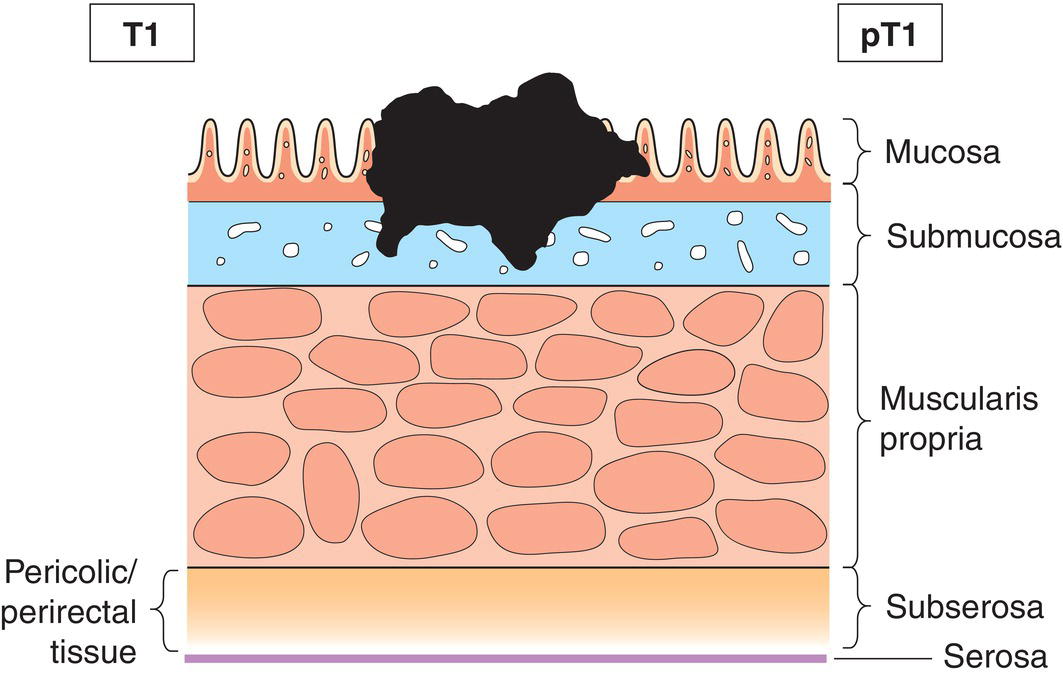
T1
Tumour invades submucosa (Fig. 180)
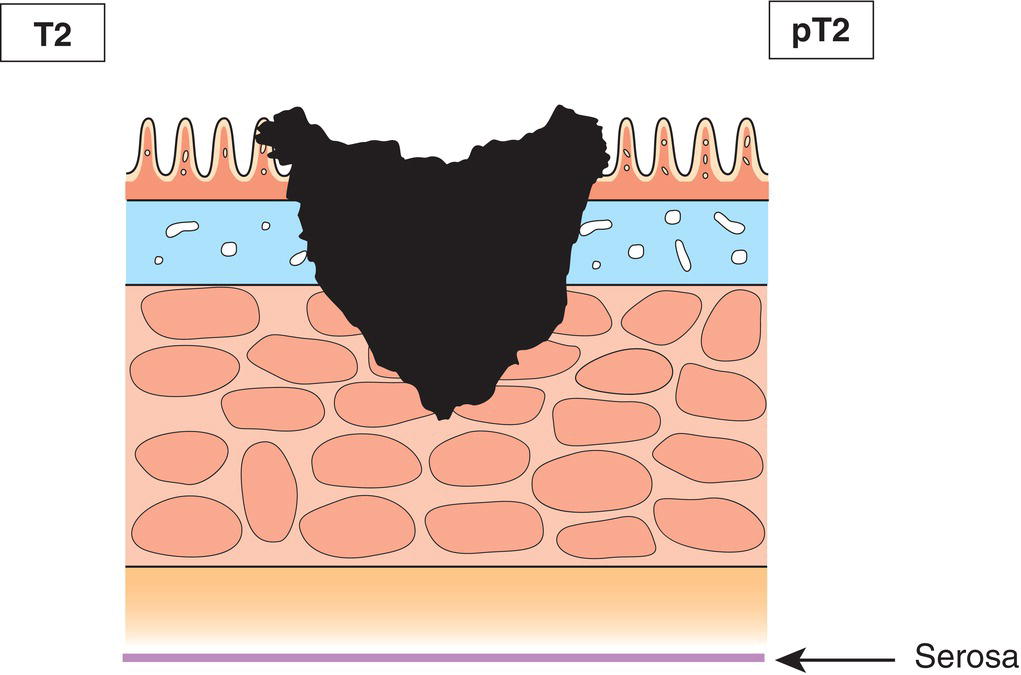
T2
Tumour invades muscularis propria (Fig. 181)
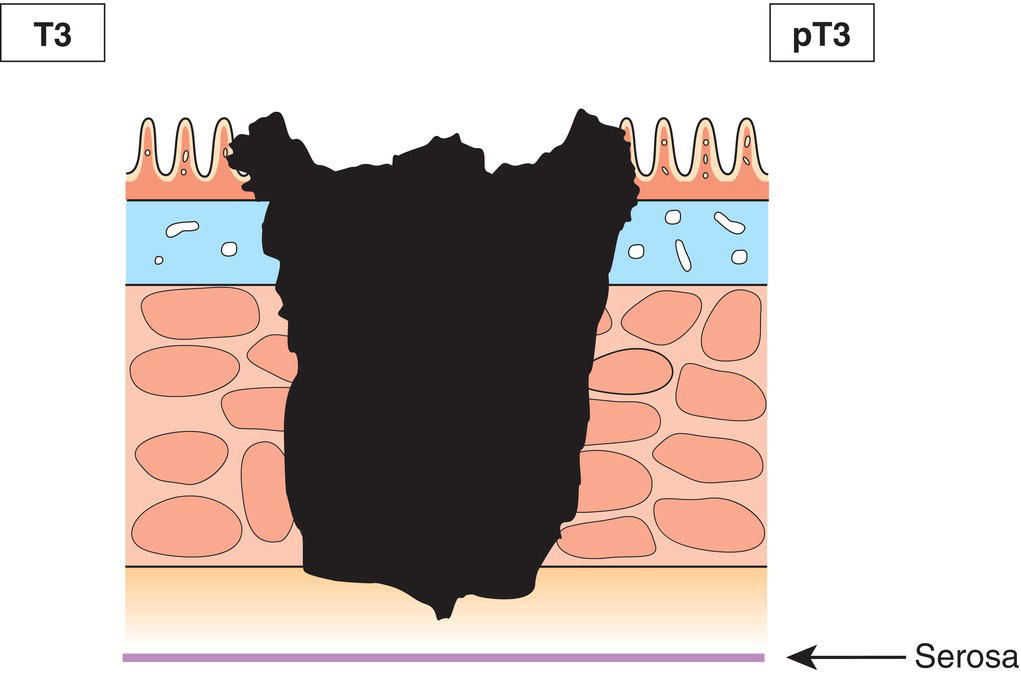
T3
Tumour invades subserosa or into non‐peritonealized pericolic or perirectal tissues (Fig. 182)
T4
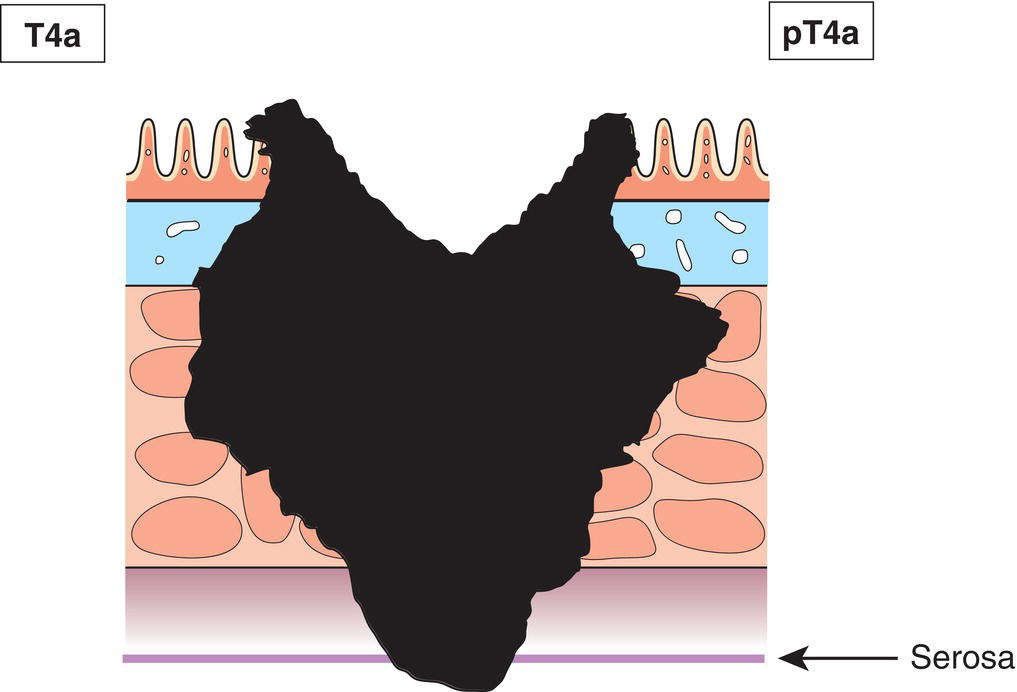
Tumour directly invades other organs or structures2,3,4 and/or perforates visceral peritoneum (Figs. 183, 184)
T4a
Tumour perforates visceral peritoneum
T4b
Tumour directly invades other organs or structures
N – Regional Lymph Nodes
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
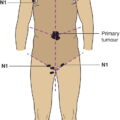
N1
Metastasis in 1 to 3 regional lymph nodes (Fig. 185)
N1a
Metastasis in 1 regional lymph node
N1b
Metastasis in 2 to 3 regional lymph nodes
N1c
Tumour deposit(s), i. e. satellites*, in the subserosa, or in non‐peritonealized pericolic or perirectal soft tissue without regional lymph node metastasis
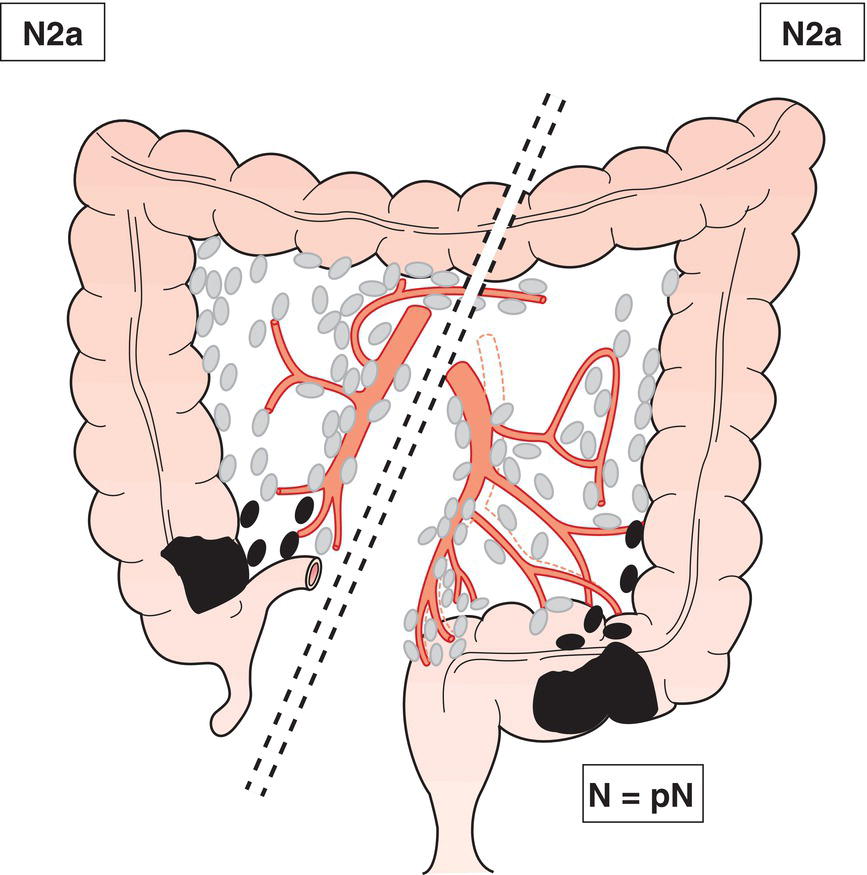
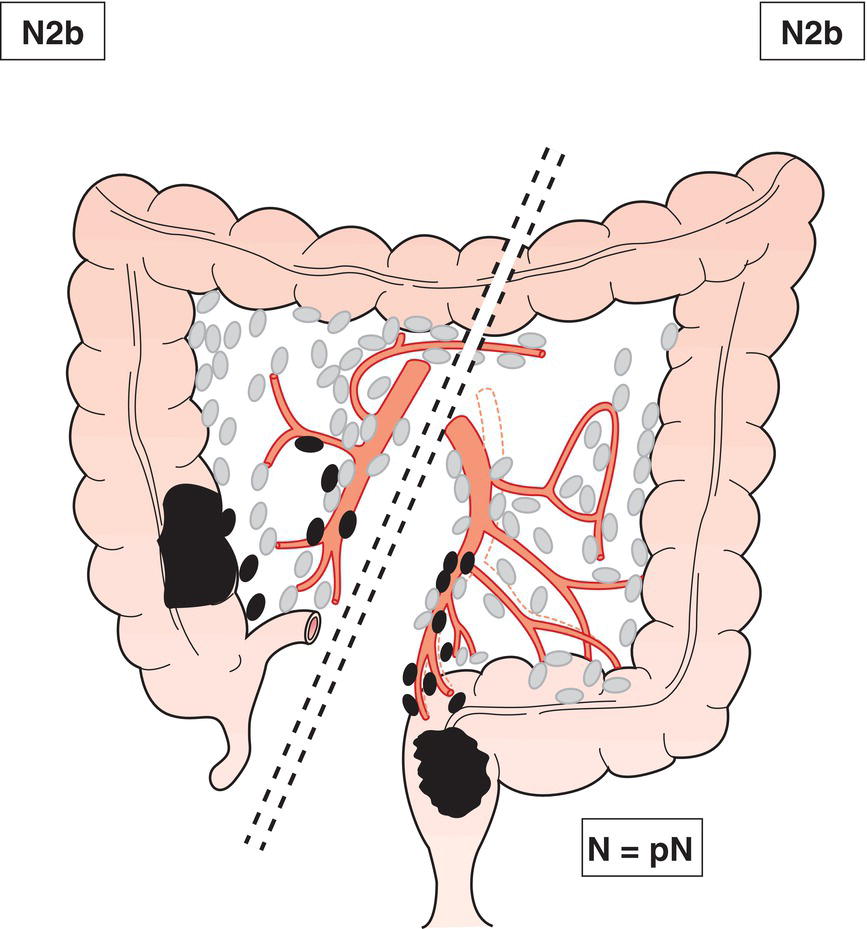
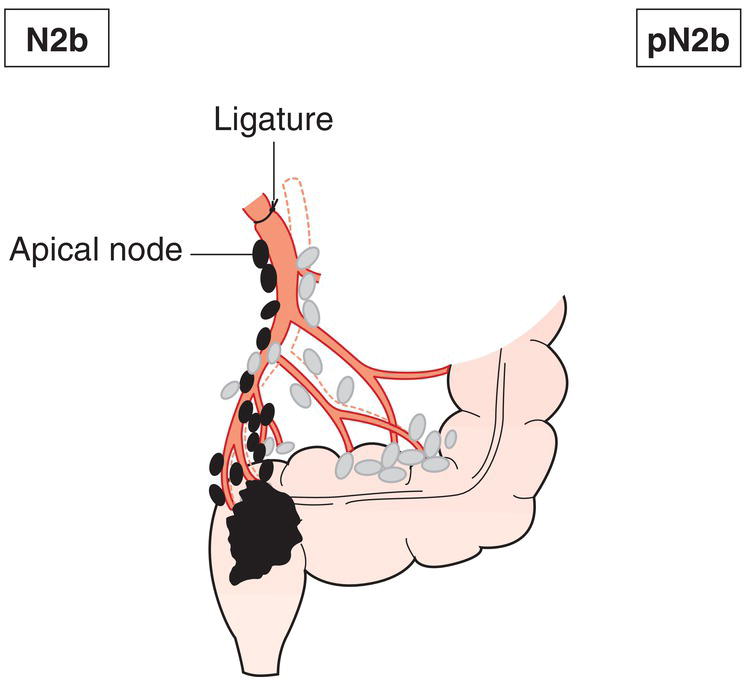
N2
Metastasis in 4 or more regional lymph nodes (Figs. 186, 187, 188)
N2a
Metastasis in 4 to 6 regional lymph nodes
N2b
Metastasis in 7 or more regional lymph nodes 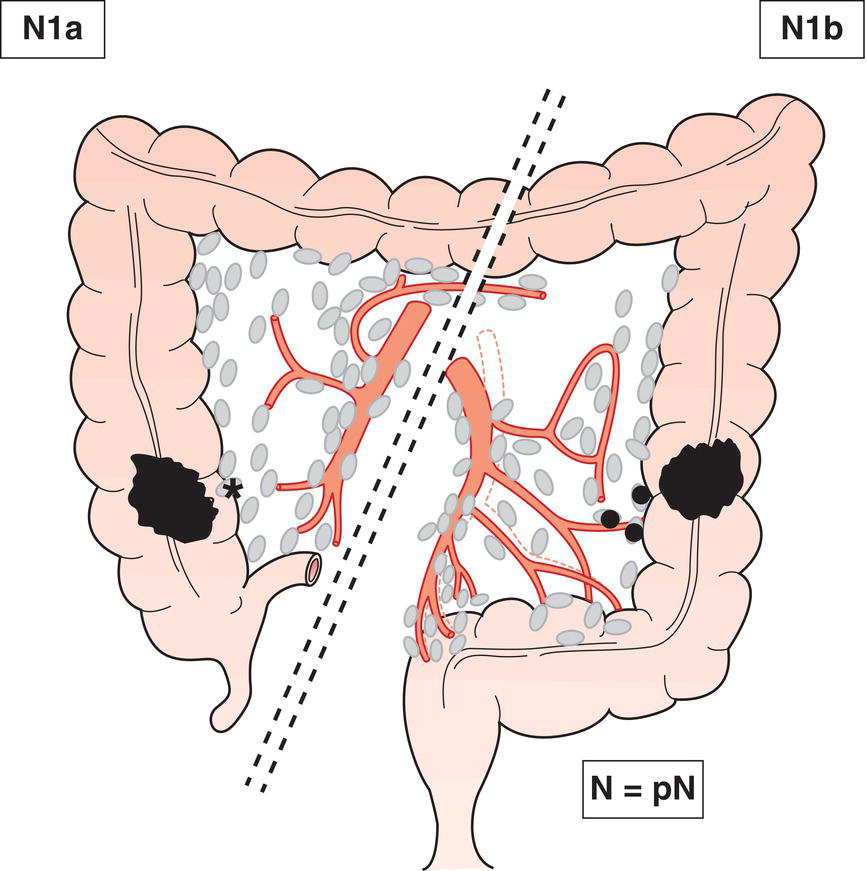
M – Distant Metastasis
M0
No distant metastasis
M1
Distant metastasis
M1a
Metastasis confined to one organ (liver, lung, ovary, non‐regional lymph node(s)), without metastases to the peritoneum
M1b
Metastases in more than one organ without metastases to the peritoneum
M1c To peritoneum with or without other organs
TNM Pathological Classification
pM1
Distant metastasis microscopically confirmed
pN0
Histological examination of a regional lymphadenectomy specimen will ordinarily include 12 or more lymph nodes. If the lymph nodes are negative, but the number ordinarily examined is not met, classify as pN0.
Summary
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree