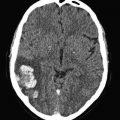
Fig. 1
Prevalence of carotid plaques in patients with unprovoked and secondary DVT and in the control subjects [8]
Subsequently, three studies have provided further evidence in support of the association between VTE and atherosclerosis. In a case-control study, Hong et al. found a higher prevalence of coronary artery calcium, as assessed by chest CT scan, in patients with unprovoked VTE than in matched control individuals [9]. In a series of almost 24,000 consecutive autopsies, Eliasson et al. found an increased prevalence of VTE in patients with arterial thrombosis, except for those with coronary artery thrombosis [10]. Finally, in a recent a case-control study conducted on subjects older than 50, we assessed the prevalence of symptomatic or subclinical atherosclerosis in 100 unselected patients with unprovoked VTE, and compared it with that of 100 patients with secondary VTE and of 100 matched control individuals free from VTE disorders [11]. In patients with unprovoked VTE, the adjusted OR for symptomatic or subclinical atherosclerosis was 5.1 (95 % CI, 2.0–13.1) in comparison to patients with secondary VTE, and 14.5 (95 % CI, 5.8–36.3) in comparison to controls. The prevalence of atherosclerosis was higher in patients with secondary VTE than in controls (OR, 3.1; 95 % CI, 1.6–6.1).
4 Risk Factors of Atherosclerosis and Venous Thromboembolism
Ageno et al. reviewed the evidence favouring the association of the most important risk factors for atherosclerosis and VTE [12]. After reviewing 21 case-control and cohort studies dealing with a total of 63,552 patients meeting the inclusion criteria, factors that were found to be significantly associated with an increased risk of VTE were obesity, blood hypertension, diabetes mellitus, and hypertriglyceridemia, According to the results of subsequent population-based study, abdominal obesity appears to be the pivotal risk factor among the individual components of the metabolic syndrome [13–15].
While the review by Ageno et al. failed to identify smoking as an additional potential risk factor for VTE, the findings from two more recent population-based studies provided strong evidence that this is the case [16, 17]. Interestingly enough, in a cross-sectional study a few markers of atherosclerosis (namely, male sex and arterial hypertension) were found to be independently associated also with an increased risk of recurrent VTE after a period of 3–6 months of vitamin K antagonist therapy for the first VTE event [18].
5 Nature of the Association
Although information coming from the above reported investigations suggests the existence of an association between VTE and atherosclerosis, it does not clarify the nature of this association. On the one hand, atherosclerosis has the potential to promote the development of thrombotic disorders in the venous system. Atherosclerosis is associated with a detectable activation of both platelets and blood coagulation as well as an increased fibrin turnover, which can lead to thrombotic complications [19–28]. The role of this prothrombotic state in favouring venous thrombotic events is plausible given the assumption that activated platelets and coagulation factors appear in the slow-flowing venous system.
On the other hand, the two clinical conditions may share common mechanisms or risk factors. In nature, there are many examples of conditions accounting for both arterial and venous thromboembolic disorders, such as hyperhomocysteinemia, antiphospholipid antibodies, malignancies, paroxysmal nocturnal haemoglobinuria, infectious states, inflammatory bowel disease, and the use of hormonal therapy [29] (Fig. 2).
Fig. 2
Potential links between venous and arterial thrombosis
Interestingly enough, a few markers of endothelial dysfunction have been found to be significantly higher in patients with unprovoked DVT than in matched control individuals [30, 31]. In a case-control investigation enrolling patients with previous unprovoked DVT and matched control individuals, flow-mediated vasodilatation was found to be significantly lower in cases than in controls; accordingly, a few parameters of endothelial function (von Willebrand factor and soluble P-selectin) were significantly higher. Interestingly enough, a few markers of platelet activation (plasma soluble CD40 ligand and urinary 11-dehydro-TxB2 levels) did not differ between the two groups (Figs. 3 and 4). Microalbuminuria, a well know marker of endothelial dysfunction whose and of arterial cardiovascular events, was found to be independently associated with an increased risk for VTE as well [32].
Fig. 3
Flow-mediated vasodilation of the brachial artery in patients with previous unprovoked DVT and in controls [30]
Fig. 4
Endothelium and platelets activation markers in patients with previous unprovoked DVT and in controls [30]
6 Is Atherosclerosis Predictive of VTE?
In an attempt to assess whether atherosclerotic disease predisposes to VTE, the authors of two similar population-based cohort studies carried out in the U.S.A., the Atherosclerosis Risk in Communities and the Cardiovascular Health Study, evaluated the rate of VTE development in subjects younger and older than 65, respectively, who had carotid ultrasound and the assessment of other subclinical parameters of atherosclerosis, and were then followed-up prospectively for several years [33, 34].
In the former study, 13,081 adults aged 45–64 years underwent carotid ultrasonography to assess the intima-media thickness and the presence of atherosclerotic plaques [33]. After adjustment for age, sex, ethnicity, body mass index and diabetes, no association was found between ultrasound parameters of subclinical atherosclerosis and VTE development after a mean follow-up of 12.5 years (adjusted hazard ratio [HR] of VTE for presence of carotid plaques, 0.97; 95 % CI, 0.72–1.29).
In the latter study, 4108 individuals aged at least 65 years underwent non-invasive assessment of subclinical atherosclerosis using carotid ultrasound (intima-media thickness and presence of plaques), ankle-brachial blood pressure index and electrocardiogram, and then were followed-up for a median of 11.7 years [34]. Surprisingly enough, the adjusted RR of overall and unprovoked VTE for presence of any type of subclinical atherosclerosis was 0.60 (95 % CI, 0.39 to 0.91) and 0.32 (95 % CI, 0.18 to 0.59), respectively. These unexpected findings were mostly explained by an inverse association of high-risk carotid plaques and arterial events during follow-up.
While in the former of the two above reported studies, the occurrence of cardiovascular and cerebrovascular events was significantly associated with the development of VTE [33], in the latter the opposite was seen [34].
In an attempt to determine the impact of cardiovascular risk factors, including family history of myocardial infarction, on the incidence of VTE, a few investigators from Norway extracted data from more than 21,000 subjects, aged 25–96 years, who had been enrolled in a prospective, population-based study (the Tromsø Study) [35, 36]. In multivariable analysis, family history of myocardial infarction was significantly associated not only with an increased risk of infarction but also of total VTE (HR, 1.27; 95 % CI 1.01–1.60) and unprovoked VTE (HR, 1.46; 95 % CI: 1.03–2.07. The risk was found to increase with increasing number of affected individuals. The association was not explained by modifiable atherosclerotic risk factors. In another population-based study, having first degree relatives with myocardial infarction before the age of 60 years was positively associated with VTE compared to participants not having a positive family history (OR 1.3; 95 % CI 1.1–1.6) [37]. Finally, in a more recent population-based study conducted in Denmark patients with a history of arterial cardiovascular events had a clearly increased relative risk of VTE events in the first 3 months following the index event, then the risk decreased yet remained statistically significant [38].
Based on these findings, asymptomatic atherosclerosis is unlikely to constitute a risk factor of venous thromboembolic disorders. Whether patients developing symptomatic complications of atherosclerosis such as myocardial infarction or stroke are at a higher risk of VTE complications is controversial.
7 Is VTE Predictive of Arterial Cardiovascular Events?
Another scenario assumes that the same biological trigger is responsible for activating coagulation and inflammatory pathways in both arterial and venous thromboembolism, in such a way determining a simultaneous risk of arterial and venous thrombotic complications. This assumption is supported by the results of a cohort study. Indeed, in an attempt to evaluate whether elevated clotting factors, which have been linked to chronic sub-clinical inflammation and arterial thromboembolic disease, have a high prevalence in patients with VTE as well, Luxembourg et al. measured the plasma level of fibrinogen, factor VIII, and high-sensitivity C-reactive protein in a cohort of sex- and age-matched patients with unprovoked VTE, patients with secondary VTE and controls [39]. They found that these markers of inflammation were significantly higher in patients with unprovoked compared to secondary VTE and controls, in such a way providing evidence in support of the hypothesis that VTE and arterial thromboembolism may share common risk factors.
If this is true, subjects with VTE may be at a higher risk of subsequent arterial cardiovascular events than matched control individuals. This hypothesis was tested in 11 studies [40–50] (Table 1) and summarized in a meta-analysis [51]. All together, the results of these studies are in keeping with the observation of a higher prevalence of carotid atherosclerosis in patients with unprovoked DVT than in matched control individuals [8, 11], and strongly suggest that patients with VTE have also an increased risk of subsequent symptomatic arterial cardiovascular events. Of particular relevance is a population-based cohort study carried out in Denmark. Using nationwide Danish medical databases, Sorensen et al. assessed the risk of hospitalization due to myocardial infarction, stroke and transient ischemic attack among 25,199 patients with DVT, 16,925 patients with PE and 163,566 population controls discharged from the Danish hospitals in a 25-year period [45]. Patients with both DVT and PE were found to have a substantially increased risk of myocardial infarction and stroke during the first year after the thrombotic event. For patients with DVT, the RRs varied from 1.60 for myocardial infarction (95 % CI 1.35–1.91) to 2.19 (95 % CI 1.85–2.60) for stroke. For patients with PE, the RRs were 2.60 (95 % CI 2.14–3.14) for myocardial infarction and 2.93 (95 % CI 2.34–3.66) for stroke. The RRs were also elevated, though less markedly, during the subsequent 20 years of follow-up, with 20–40 % increases in risk for arterial cardiovascular events. RRs were similar for those with provoked and unprovoked DVT and PE (Figs. 5 and 6).
Table 1
Main studies addressing the risk of arterial cardiovascular events in patients with VTE
Ref | Study design | Study population | Number | Findings |
|---|---|---|---|---|
[40] | Prospective cohort | Idiopathic PE | 209 | Idiopathic PE risk factor of arterial cardiovascular events |
Secondary PE | 151 | |||
[41] | Prospective cohort | Idiopathic VTE | 1063 | Idiopathic VTE risk factor of arterial cardiovascular events |
Secondary VTE | 856 | |||
[42] | Extended follow-up of the DURAC study | VTE patients | 897 | Higher mortality from myocardial infarction or stroke in VTE patients |
General Swedish population | ||||
[43] | Retrospective cohort | DVT patients | 151 | Idiopathic VTE risk factor of arterial cardiovascular events |
Controls | 151 | |||
[44] | Prospective cohort | DVT with residual thrombosis | 173 | Residual thrombosis risk factor of vascular death |
DVT with recanalized veins | 143 | |||
[45] | Population-based | VTE patients | 42,124 | VTE risk factor of myocardial infarction or stroke |
Controls | 163,566 | |||
[46] | Population-based | Idiopathic VTE | 6065 | Idiopathic VTE in patients aged < 40 risk factor of myocardial infarction |
Controls | 12,040 | |||
[47] | Prospective cohort | PE patients | 364 | Idiopathic PE risk factor of subsequent arterial cardiovascular events |
Suspected PE (not confirmed) | 334 | |||
[48] | Population-based | VTE patients | 1311 | VTE not a predictor of myocardial infarction |
Controls | 1511 | |||
[49] | International RIETE registry | VTE patients | 23,370 | PE-related mortality lower than mortality due to ischemic events |
[50] | Prospective cohort | DVT patients | 244 | Idiopathic DVT risk factor of subsequent arterial cardiovascular events |
Suspected DVT (not confirmed) | 991 |
Fig. 5
Risk of acute myocardial infarction and stroke in patients with unprovoked VTE in relation to the length of the follow-up period [45]
Fig. 6
Risk of acute myocardial infarction and stroke in patients with secondary VTE in relation to the length of the follow-up period [45]
Whether the risk of subsequent arterial thrombotic disorders applies to all VTE patients or to the only patients with unprovoked disease is uncertain. According to the results of a meta-analysis of six studies, the risk appears higher in patients with unprovoked VTE compared to those with provoked VTE (IRR 1.86, 95 % CI 1.19–2.89) [51]. Of interest, based on recent findings the persistence of residual thrombosis, as assessed with ultrasonography 3 months after an episode of proximal DVT, predicts the development of arterial thrombotic disorders both in patients with unprovoked and in those with secondary DVT [52].
8 Implications of the Association
We speculate that venous and arterial thrombosis are two aspects of the same disease (i.e., thrombosis), and that this disease may electively affect genetically predisposed individuals resulting in clinically manifestations that are, in turn, depending on a variety of elements including the age of patients, their lifestyle, and the occurrence of co-morbidities and circumstantial factors: the venous thrombotic events being more frequent, for example, after triggering risk factors such as surgery or trauma, and the arterial thrombotic events being more frequent in subjects who have developed atherosclerosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree