ANATOMIC LOCALIZATION
Part of “CHAPTER 75 – CUSHING SYNDROME“
DETECTION OF PITUITARY LESIONS
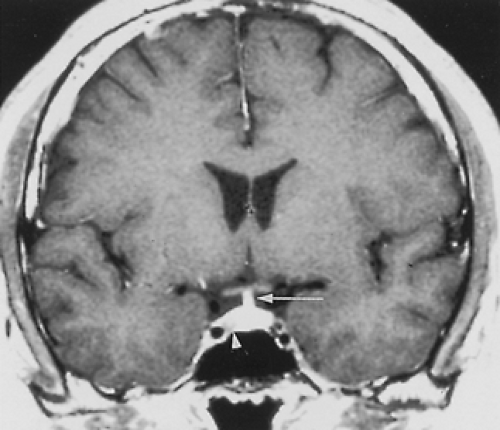
After the diagnosis of Cushing disease has been established on clinical and biochemical grounds, the presence of pituitary lesions should be further determined by magnetic resonance imaging (MRI) of the sella turcica. Because of the small size of most pituitary tumors associated with Cushing disease, the results of plain radiographic studies are often normal or misleading. Large microadenomas secreting ACTH are extremely rare at the time the initial diagnosis of the disease is made. However, small (<10 mm) pituitary microadenomas can be identified by MRI of the pituitary gland with gadolinium contrast using coronal cuts in approximately 70% of patients with Cushing disease. On T1-weighted images, the lesion usually appears as a nonenhancing abnormality surrounded by an enhancing normal pituitary gland (Fig. 75-7).
Petrosal sinus sampling with or without CRH stimulation can be used for localization of pituitary tumors.47 Through a percutaneous
bilateral femoral approach, catheters are placed in the left and right inferior petrosal sinuses, and blood for ACTH is withdrawn simultaneously from both catheters and from a peripheral vein. To account for fluctuations in levels caused by the pulsatile nature of ACTH secretion, sequential samples (i.e., four samples drawn on both sides over a 20-second period at 2-to 5-minute intervals) are obtained. A plasma ACTH concentration gradient (i.e., petrosal sinus/peripheral vein ACTH of ≥1.6) verifies the pituitary source of ACTH. A right to left discrepancy may also help to lateralize ACTH secretion and aids in the preoperative localization of the lesion. A lateralization of the source of ACTH by this procedure can help in cases in which a tumor is not found at the time of surgery. Partial resection of the side of the pituitary where the highest ACTH levels are recorded can be accompanied by remission of the disease. Failure to find the pituitary microadenoma or to induce cure after resection of the side of the pituitary with the highest concentration of ACTH may be due to failure to remove the involved part of the pituitary gland completely or to the fact that confluent pituitary veins do not invariably drain into the ipsilateral inferior petrosal sinus, so that a microadenoma may be present in the opposite side of the pituitary gland.48
bilateral femoral approach, catheters are placed in the left and right inferior petrosal sinuses, and blood for ACTH is withdrawn simultaneously from both catheters and from a peripheral vein. To account for fluctuations in levels caused by the pulsatile nature of ACTH secretion, sequential samples (i.e., four samples drawn on both sides over a 20-second period at 2-to 5-minute intervals) are obtained. A plasma ACTH concentration gradient (i.e., petrosal sinus/peripheral vein ACTH of ≥1.6) verifies the pituitary source of ACTH. A right to left discrepancy may also help to lateralize ACTH secretion and aids in the preoperative localization of the lesion. A lateralization of the source of ACTH by this procedure can help in cases in which a tumor is not found at the time of surgery. Partial resection of the side of the pituitary where the highest ACTH levels are recorded can be accompanied by remission of the disease. Failure to find the pituitary microadenoma or to induce cure after resection of the side of the pituitary with the highest concentration of ACTH may be due to failure to remove the involved part of the pituitary gland completely or to the fact that confluent pituitary veins do not invariably drain into the ipsilateral inferior petrosal sinus, so that a microadenoma may be present in the opposite side of the pituitary gland.48
Another possibility is the presence of multiple microadenomas. The administration of CRH at the time of catheterization may enhance differences between the two sides; however, a simultaneous response by the uninvolved gland may blur the differences.
To correct for unequal dilution by nonpituitary venous blood, other pituitary hormones, including prolactin, thyroid-stimulating hormone (TSH), human chorionic gonadotropin, and α subunit, have been measured simultaneously. The assumption was that an ACTH-secreting microadenoma would not cause unequal delivery of these hormones into the two inferior petrosal sinuses, but correction of the ACTH gradients by these hormones did not improve the discriminatory ability of the test.49
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree