Altered Fractionation Schedules
Altered Fractionation Schedules
Conventional fractionation consists of daily fractions of 1.8 to 2.0 Gy, 5 days per week; the total dose is determined by the tumor being treated and the tolerance of critical normal tissues in the target volume (usually 60 to 75 Gy).
Hyperfractionation uses an increased total dose, with the size of dose per fraction significantly reduced and the number of fractions increased; overall time is relatively unchanged. Quasi-hyperfractionation is the same as hyperfractionation, except that total dose is not increased.
In accelerated fractionation, overall time is significantly reduced; the number of fractions, total dose, and size of dose per fraction are unchanged or somewhat reduced, depending on the overall time reduction.
Quasi-accelerated fractionation is the same as accelerated fractionation, except that overall time is not reduced because of treatment interruption, which defeats the rationale of accelerated fractionation.
Accelerated hyperfractionation has features of both hyperfractionation and accelerated fractionation.
Concomitant boost is an additional dose delivered 1 or more times per week to selected target volumes (i.e., gross tumor volume) through smaller field(s), along with the conventional dose to larger irradiated volumes.
To achieve an increase in tolerance of late-responding tissues through dose fractionation, the time interval between the dose fractions must be long enough (6 hours) to allow cellular repair to approach completion.
Two Radiation Therapy Oncology Group (RTOG) reports showed an increased rate of late complications with hyperfractionated protocols when the mean interfraction interval was less than 4.5 hours (
1). Most protocols now stipulate a minimum 6-hour interval between dose fractions. Clinical data suggest that this is adequate for normal tissues other than the spinal cord.
OVERALL TIME
The intensity of acute reactions is determined primarily by the rate of dose accumulation (daily dose fractionation).
The importance of the dose per fraction is a reflection of the biologic fact that acute reactions represent a deficit in the balance between the rate of cell killing by radiation and cell regeneration from surviving stem cells.
After the stem cell population is depleted to the point at which it is unable to renew the functional layers of the epithelium, the acute reaction peaks, and further depopulation produces no increase in the severity of the reaction.
The time taken to heal depends on the total dose, provided the weekly dose rate exceeds the regenerative ability of the surviving stem cells. This is because healing is a function of the absolute number of stem cells surviving the course of treatment, and the higher the total dose, the fewer stem cells will survive.
Curability of many cancers (particularly squamous cell carcinomas) is highly dependent on overall treatment time; this has been interpreted in terms of accelerated regeneration of surviving tumor clonogens.
Evidence for accelerated regeneration of surviving tumor cells after therapeutic intervention comes from three observations: time-to-recurrence data for tumors not sterilized by radiation therapy, comparison of split-course and continuous-course treatment regimens, and analysis of tumor control doses as a function of time (with correction for fraction size differences) (
24).
SPLIT-COURSE VERSUS CONTINUOUS-COURSE TREATMENT
Inferior results were found with split-course treatment for head and neck cancer, compared to continuous-course treatment, when daily and total doses were not adjusted to compensate for treatment interruptions (
16).
Approximately 0.6 Gy per day is needed to compensate for a prolongation in treatment time (
8).
LINEAR-QUADRATIC EQUATION
The linear-quadratic equation is internally consistent for a wide range of tissue types and end points.
Clinical application of the model for derivation of new fractionation schedules is limited by a lack of precise estimates of α/β.
The α/β ratios of available human data are consistent with experimentally determined α/β ratios, with wide confidence limits (
Table 5-2).
HYPERFRACTIONATION
Small dose fractions allow higher total doses to be administered within the tolerance of late-responding normal tissues, and a higher biologically effective dose can be delivered to the tumor.
Radiosensitization is achieved through redistribution and lesser dependence on oxygen effect.
More severe acute reactions occur than with conventional fractionation, but a therapeutic gain should be realized in tumors with large α/β ratios.
ACCELERATED FRACTIONATION
Reduction in overall treatment time decreases the opportunity for tumor cell regeneration during treatment and increases the probability of tumor control for a given total dose.
Because overall treatment time has little influence on probability of late, normal tissue injury (provided the size of the dose per fraction is not increased and the interval between dose fractions is sufficient for complete repair to take place), a therapeutic gain should be realized.
When the overall duration of treatment is markedly reduced, the total dose must be reduced as well, to prevent excessively severe acute reactions. Therapeutic gain is realized only if the dose equivalent of regeneration of tumor cells during the time by which treatment is shortened exceeds actual reduction in dose mandated by maximum tolerated dose for acute reactions.
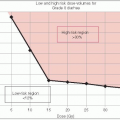
Type A accelerated fractionation is an intensive short course of treatment; overall duration of treatment is markedly reduced, and total dose is substantially decreased.
In types B and C, duration of treatment is more modestly reduced, and total dose is kept in the same range as conventional treatment by using split-course or concomitant-boost technique.
In type D accelerated fractionation, the total dose delivered per week progressively increases during treatment; less-intensive therapy at the outset of treatment stimulates a regenerative response in normal mucosa so that it can better tolerate more intensive treatment as the course progresses. There is a slightly greater reduction in overall time (without decreasing total dose) than with types B and C.
Techniques are differentiated on the basis of the strategy adopted to circumvent intolerable acute reactions: Type A, reduction in dose; type B, break in treatment; type C, reduction in volume of mucosa exposed to accelerated treatment; type D, stimulation of mucosal regenera tive response by starting with a milder fractionation schedule (
4) (
Fig. 5-1).