Adrenocortical carcinoma (ACC) presents with overt symptoms of hormone excess (usually androgen, cortisol, or combined hypersecretion) in 30%–40% of cases. Notably, even patients with incidentally discovered ACC or those presenting with symptoms of mass effect may have undiagnosed adrenal hormone excess. Uncontrolled or unrecognized overt Cushing syndrome (CS) carries additional morbidity and is a negative prognostic factor in patients with ACC. These patients are at high risk for deep venous thrombosis and pulmonary embolism, as well as infections. Surgical resection is the best therapy for ACC-related CS. However, when surgery is not possible, aggressive medical therapy for hypercortisolism should be initiated. Here, we present a case of metastatic ACC with severe CS of rapid onset.
Case Report
The patient was a 57-year-old man who was referred for evaluation of a newly found large adrenal mass. This was initially found on the ultrasound that was ordered to evaluate abdominal discomfort. In addition to abdominal pain, he reported other new symptoms for around 6 months. The symptoms included fatigue, mood changes, weight loss of around 10 pounds but with development of abdominal obesity, upper and lower extremity weakness, facial rounding and erythema, skin fragility and bruising, and curling hair. In addition, he developed uncontrolled hypertension and hypokalemia.
On physical examination, blood pressure was 152/86 mmHg, heart rate was 76 beats per minute, and body mass index was 25.1 kg/m 2 . Physical examination was positive for facial rounding and erythema, supraclavicular pads, abdominal obesity, multiple bruises over extremities and abdomen, and several skin tears. No significant myopathy was noticed on examination. He had bilateral 1+ lower extremity edema.
INVESTIGATIONS
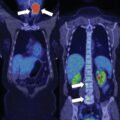
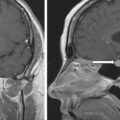
Clinical presentation was highly suspicious for ACC and severe CS. Computed tomography (CT) of the abdomen, pelvis, and chest was performed for a better characterization of the adrenal mass and staging. A left lobulated heterogeneous adrenal mass measuring 18 × 14 × 15 cm was demonstrated ( Fig. 28.1 ). In addition, several hepatic lesions measuring up to 12 cm were consistent with metastases. Other possible metastases included a vertebral T11 lesion of 1.2 cm and several indeterminate lung nodules measuring 3–5 mm.

Because of clinical findings of lower extremity edema and suspected severe hypercortisolism, the patient was considered at high risk for deep venous thrombosis. A lower extremity ultrasound was obtained and revealed an acute deep venous thrombosis through the right lower extremity (mid-low femoral vein, extending throughout the popliteal, posterior tibial, peroneal, soleal, and gastrocnemius veins).
Laboratory evaluation confirmed severe adrenal-dependent hypercortisolism, as well as androgen, estrogen, progesterone, and glucocorticoid and androgen precursor excess ( Table 28.1 ).
| Biochemical Test | Result | Reference Range |
| Cortisol, mcg/dL | 27 | 7–21 |
| ACTH, pg/mL | <5 | 7.2–63 |
| DHEA-S, mcg/dL | 3477 | 44–332 |
| Androstenedione, ng/dL | 1880 | 30–200 |
| Total testosterone, ng/dL | 181 | 240–950 |
| Estradiol, pg/ml | 83 | 10–40 |
| Progesterone, ng/mL | 2.5 | <0.2 |
| 17-Hydroxypregnenolone, ng/dL | 1140 | 55–455 |
| Pregnenolone, ng/dL | 371 | 33–248 |
| 17-Hydroxyprogesterone, ng/dL | 207 | <220 |
| 11-Deoxycortisol, ng/dL | 832 | 10–79 |
| Aldosterone, ng/dL | <4 | <21 |
| Plasma renin activity, ng/mL per hour | 1.7 | ≤0.6–3 |
| 24-Hour urine cortisol, mcg/24 h | 1723 | <45 |
| Plasma metanephrine, nmol/L | <0.2 | <0.5 |
| Plasma normetanephrine, nmol/L | 0.24 | <0.9 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree