When a patient is incidentally discovered with an adrenal mass, two questions need to be answered: (1) Is the adrenal mass malignant? (2) Is the adrenal mass hormonally active? Age, patient’s history, tumor size, and imaging characteristics are useful in assessing the potential for adrenal malignancy. Adrenal “incidentaloma” is frequently ignored by clinicians. However, 3% of all adrenal incidentalomas are malignant. When imaging characteristics of the adrenal mass do not clearly exclude malignancy (i.e., malignancy is excluded if the unenhanced computed tomography [CT] attenuation is <10 Hounsfield units [HU]), , further action is needed and may include imaging monitoring, another imaging test, or adrenalectomy.
Case Report
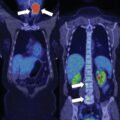
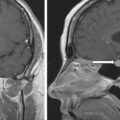
The patient was a 29-year-old woman who presented for evaluation of a large adrenal mass. One year before referral, she discontinued oral contraceptive therapy in attempt to conceive. Six months before referral, she was evaluated by her gynecologist for secondary amenorrhea (she did not resume her menses since stopping oral contraceptive therapy). Workup at that time revealed elevated dehydroepiandrosterone sulfate (DHEA-S) and testosterone, and abdominal imaging was obtained and demonstrated a 7.3 × 5.8 × 7.0–cm left adrenal mass (unenhanced CT attenuation = 35 HU). The patient was then referred to our institution. Notably, the patient reported that more than 3 years prior, she had a CT scan for abdominal pain that demonstrated an incidental adrenal nodule. She was advised that the adrenal incidentaloma was a benign finding that needed no further follow-up. She did not have workup for adrenal hormone excess at that time. On physical examination her body mass index was 33.6 kg/m 2 and blood pressure 145/104 mmHg. She was not cushingoid. Acne was present on her face, shoulders, and chest.
INVESTIGATIONS
Laboratory tests were obtained ( Table 23.1 ). Marked hyperandrogenemia was noted with significantly elevated androstenedione and testosterone and mild elevation of DHEA-S. In addition, despite the absence of clinical features of Cushing syndrome, glucocorticoid autonomy was demonstrated with an abnormal dexamethasone suppression test. Workup for primary aldosteronism and catecholamine excess was negative.
| Biochemical Test | Result | Reference Range |
| Post–1-mg DST cortisol, mcg/dL | 8.3 | <1.8 |
| ACTH, pg/mL | 24 | 10–60 |
| Aldosterone, ng/dL | <4 | ≤21 |
| Plasma renin activity, ng/mL per hour | 1.2 | ≤0.6–3 |
| DHEA-S, mcg/dL | 485 | 44–332 |
| Total testosterone, ng/dL | 256 | 8–60 |
| Androstenedione, ng/dL | 2010 | 30–200 |
| Plasma metanephrine, nmol/L | <0.2 | <0.5 |
| Plasma normetanephrines, nmol/L | 0.26 | <0.9 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree