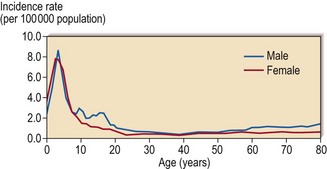
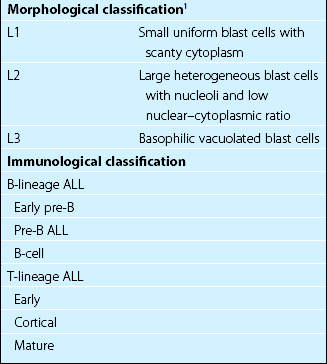
21 ALL has a peak incidence in childhood with a gradual rise in incidence in later years (Fig 21.1). The disease has distinct characteristics in children and adults. Childhood ALL is often curable by chemotherapy whereas cure is elusive in adult ALL. Poorer outcome in adult ALL is due to a combination of a greater frequency of high-risk leukaemia with more drug resistance, and less effective treatment regimens. The French-American-British (FAB) morphological classification is based on characteristics of the blast cells, including cell size, nuclear–cytoplasmic ratio, number and size of nucleoli and the degree of cytoplasmic basophilia (Fig 21.2). Morphological classification is now less important than that based on immunophenotyping, cytogenetics and molecular analysis (Table 21.1). Fig 21.2 Morphology of ALL blast cells. In the selection of treatment it is important to differentiate between three broad groups; T-cell ALL, mature B-ALL and all other types of B-lineage ALL. Genetic abnormalities are becoming increasingly important in classification of ALL as they give vital prognostic information (Table 21.2). Table 21.2 Chromosomal abnormalities in ALL
Acute lymphoblastic leukaemia
Classification
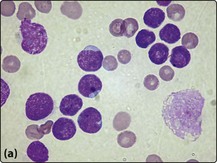
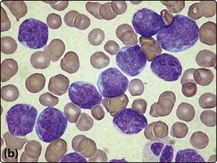
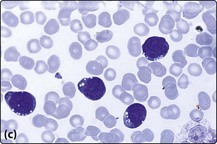
(a) L1 type; (b) L2 type; (c) L3 type. Note that the L2 cells have more cytoplasm and more prominent nucleoli than L1 cells. L3 type cells have cytoplasmic vacuolation.
Abnormality
Prognostic significance
Numerical change
High hyperdiploidy (over 50 chromosomes)
Favourable
Hyperdiploidy (47–50)
Intermediate
Pseudodiploidy (46 with structural/numerical change)
Intermediate
Hypodiploidy (less than 46)
Poor
Structural abnormality
Genes involved
Philadelphia chromosome, t(9;22)1
BCR-ABL
Poor
t(12;21)2
TEL-AML1 (ETV6-RUNX1)
Good
t(1;19)
E2A-PBX1
Good
t(v;11q23)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access