Chapter 65 Acute Coronary Syndromes
Table 65-1 Pharmacologic Characteristics of Fibrinolytic Drugs Used in the Management of Patients With ST-Segment Elevation Myocardial Infarction
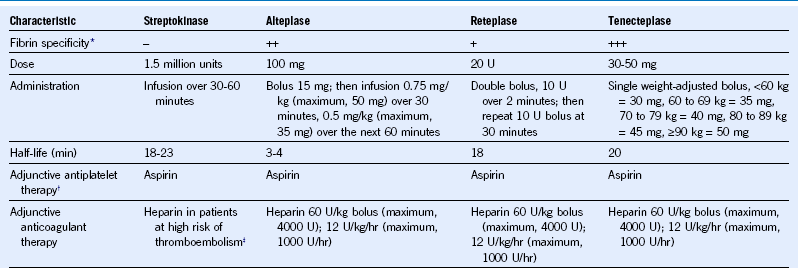
* Less fibrin specificity is associated with more systemic fibrinogen depletion.
Case 1: Bleeding After Fibrinolytic Therapy
Comment
Fibrinolytic trials report a 1% to 6% incidence of major bleeding and a 10% incidence of moderate bleeding during the first 30 days. The most common sources of major bleeding are the gastrointestinal tract and procedure-related bleeding. The principles of management of major bleeding in STEMI patients treated with fibrinolytic therapy are summarized in Table 65-2. Steps include (1) stop antithrombotic therapies; (2) use local measures when possible to control bleeding; (3) draw blood to measure fibrinogen, prothrombin time (PT), aPTT, and possibly anti-Xa levels (to measure the anticoagulant effect of low-molecular-weight heparin) and to crossmatch blood; and (4) administer therapies to mitigate or reverse the effects of fibrinolytic, antiplatelet, and anticoagulant drugs.
Table 65-2 Management of Major Bleeding in Patients With ST-Segment Elevation Myocardial Infarction Treated With Fibrinolytic Therapy
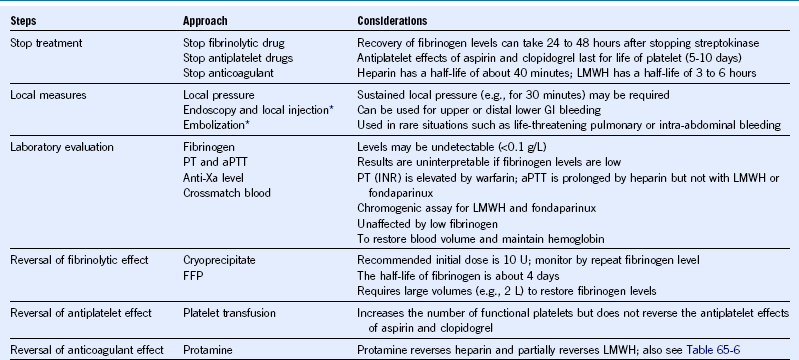
aPTT, Activated partial thromboplastin time; FFP, fresh-frozen plasma; GI, gastrointestinal; INR, international normalized ratio; LMWH, low-molecular-weight heparin; PT, prothrombin time
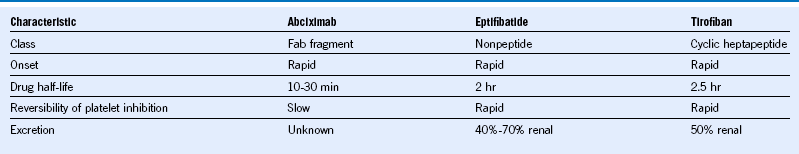
Table 65-3 Pharmacologic Characteristics of Oral Antiplatelet Drugs Commonly Used in the Management of Acute Coronary Syndromes
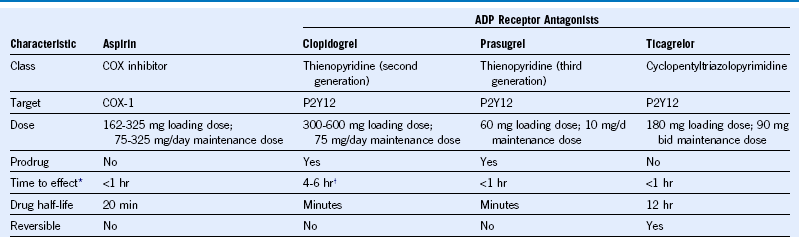
ADP, Adenosine diphosphate; bid, twice daily; COX, cyclooxygenase.