Summary of Key Points
- •
The acute and late toxicity of radiotherapy (RT) for lung cancer usually involves the lungs, esophagus, and heart.
Lung
- •
Post-RT, there are multiple biochemical and molecular events involving type II pneumocytes, surfactant protein transudation into alveolar spaces, with subsequent inflammation with associated capillary obstruction, and then much later tissue fibrosis.
- •
The risk for clinical lung injury has been associated with various dosimetric factors (e.g., mean lung dose), clinical factors (e.g., preexisting pulmonary comorbidities), and cytokines (e.g., IL-6, IL-8, and TGF-β1).
- •
Prednisone is typically effective in treating patients with troublesome symptoms of radiation peumonitis.
Esophagus
- •
Acute esophageal injury is common and is manifest by pain with swallowing, reflecting mucosal injury. Late injury is typically manifest as partial obstruction or fistula.
- •
Various dosimetric and clinical factors (e.g., concurrent chemotherapy) have been associated with acute and late injury.
- •
Acute symptoms are treated with dietary changes, proton pump inhibitors, analgesics, local anesthetics, promotility agents, intravenous fluids, and/or nasogastric tube or gastrostomy tube insertion. Late esophageal stenosis or fistulae may require repeated dilatations or stents.
Heart
- •
Radiation can accelerate atherosclerosis of “large vessels” (often seen only many years/decades post-RT) and/or cause subclinical microvascular injury (within months of RT). Pericardial inflammation and thickening may also occur.
- •
Additional work is needed to better understand the radiation dose/volume/risk relationships and clinical relevance of heart injury in patients with lung cancer.
Acknowledgment
Supported in part by US NIH grant CA 69579, the Department of Defense, and the Lance Armstrong Foundation (LBM).
The organs most commonly at risk of injury during and shortly after thoracic radiotherapy for lung cancer are the lungs and esophagus. Injury to the heart is usually a late effect and is conditional on the patient living long enough for it to become clinically evident.
Pulmonary Toxicity
Pathophysiology
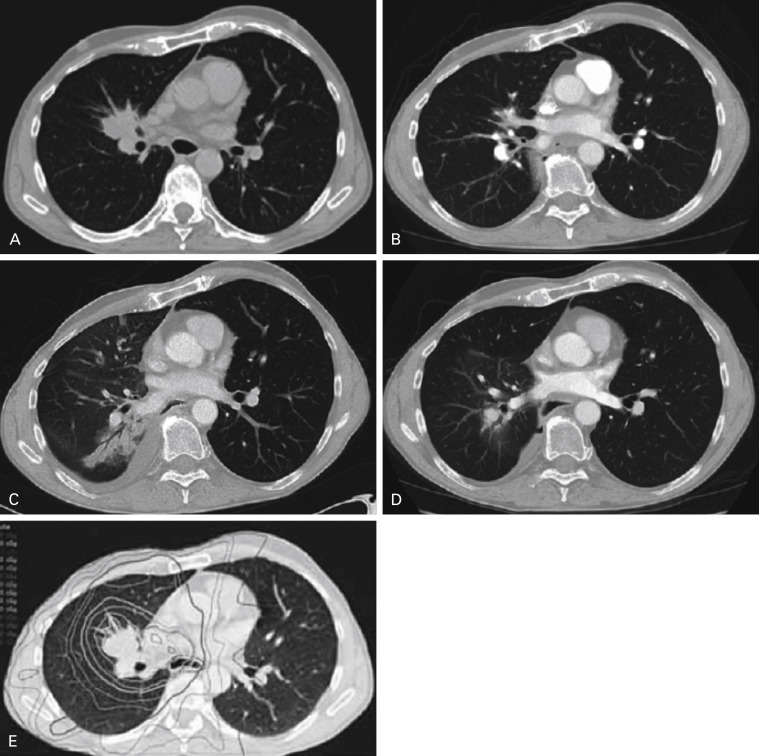
Radiation pneumonitis (RP) can be divided into three stages—latent, acute, and late. Following radiation there is a latent phase in which there is no apparent symptomatic or radiologic changes. However, microscopically there is degranulation and loss of type II pneumocytes, loss of surfactant, swelling of the basement membrane, and protein transudation into the alveolar spaces. Due to an influx of macrophages and fibroblasts, there is a release of cytokines such as transforming growth factor-beta (TGF-β), interleukin (IL)-2, fibronectin and growth factors such as IGF-1, platelet-derived growth factor, and tumor necrosis factor-alpha (TNF-α). During the acute phase there can be imaging changes and clinical symptoms. The chest x-ray or computerized tomography (CT) scan may show the typical changes of a diffuse infiltrative process corresponding to the radiation field ( Fig. 42.1 ). The symptoms are classically a nonproductive cough, fatigue, shortness of breath, and/or fever. This acute phase occurs within 6–7 months of the delivery of radiation, with a peak incidence of 2–3 months. Microscopically there is a continued inflammatory response with capillary obstruction and an increase in leukocytes, plasma cells, macrophages, fibroblasts, and collagen fibers. The alveolar septa appear thickened and the alveolar space smaller. In the late phase of RP, the imaging will show dense consolidation and volume loss of lung tissue. Some of the acute symptoms such as fever, cough, and fatigue often resolve although it would not be uncommon to have chronic shortness of breath. Pathologically, there is fibrosis of the endothelium and an increase in the thickness of the alveolar septa with obliteration of many alveolar spaces.
The trachea and bronchi are lined with pseudostratified ciliated columnar epithelial cells and mucus-producing goblet cells. A mild to moderate dry cough is common during the acute phase of lung radiation due to depletion of the mucosa. This cough usually resolves shortly after 60–66 Gy radiation therapy, and severe late complications are relatively unusual. In 88 stage III nonsmall cell lung cancer (NSCLC) patients treated to 66 Gy or higher, Lee et al. observed bronchial stenosis in three patients between 2–7 months, representing 11% of all late complications. Miller et al. reported an actuarial rate of treatment-related bronchial stenosis at 1 and 4 years of 7% and 38%, respectively. Radiation dose was suspected to be a factor, with bronchial stenosis observed in 4% and 25% of patients treated to 74 Gy and 86 Gy, respectively. The correlation of mainstem bronchial stenosis with doses of 73 Gy or more was confirmed in a further study by Kelsey et al. This narrowing of the bronchi occurred as early as 3 months following radiation. The caliber of the trachea on the other hand was unchanged following even high doses of radiation.
Grading of Lung Toxicity
Radiation-induced pulmonary toxicity after radical radiotherapy or chemoradiation is complex to score in lung cancer patients because it is difficult to distinguish from tumor progression and exacerbation of preexisting pulmonary comorbidities. The Common Terminology Criteria for Adverse Events (CTCAE) grading system, in common use worldwide for scoring of toxicity, has been modified over the years ( http://www.eortc.be/services/doc/ctc/ ).
The Radiation Therapy Oncology Group (RTOG) had its own grading system initially but has adopted the CTCAE over the last 10 years. An important difference between the RTOG and CTCAE grading system is that the RTOG differentiates between acute (pneumonitis) and late (fibrosis) toxicity based upon the time interval (90 days) after treatment. The choice of 90 days is somewhat arbitrary as the active inflammatory phase of pneumonitis can persist beyond 90 days. Tables 42.1 and 42.2 summarize the RTOG grading systems as well as the CTCAE version for pneumonitis and pulmonary fibrosis. In all these grading systems grade 5 toxicity is death ( http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_40 ).
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | |
|---|---|---|---|---|
| RTOG | Mild symptoms of dry cough or dyspnea on exertion. | Persistent cough requiring narcotic or antitussive agents. Dyspnea with minimal effort but not at rest. | Severe cough, unresponsive to narcotic antitussive agent or dyspnea at rest. Clinical or radiologic evidence of acute pneumonitis. Intermittent oxygen or steroids may be required. | Severe respiratory insufficiency. Continuous oxygen or assisted ventilation. |
| CTCAE v4.0 2009 | Asymptomatic; clinical or diagnostic observations only; intervention not indicated. | Symptomatic; medical intervention indicated; limiting instrumental activities of daily living. | Severe symptoms; limiting self-care ADL; oxygen indicated. | Life-threatening respiratory compromise; urgent intervention indicated (e.g., tracheotomy or intubation). |
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | |
|---|---|---|---|---|
| CTCAE v4.0 2009 | Mild hypoxemia; radiologic pulmonary fibrosis <25% of lung volume. | Moderate hypoxemia; evidence of pulmonary hypertension; radiographic pulmonary fibrosis 25–50%. | Severe hypoxemia; evidence of right-sided heart failure; radiographic pulmonary fibrosis >50–75%. | Life-threatening consequences (e.g., hemodynamic/pulmonary complications); intubation with ventilatory support indicated; radiographic pulmonary fibrosis >75% with severe honeycombing. |
Changes in Pulmonary Function Tests
The RTOG grading system was heavily dependent on the prescription of drugs or oxygen, which varies greatly from physician to physician. The CTCAE grading systems did away with that in the later versions, but still require subjective assessment of symptom severity, its effect on activities of daily living, and the indication for oxygen. More objective criteria to measure pulmonary toxicity have been sought such as changes in pulmonary function tests (PFTs).
Miller et al. summarized the changes in PFTs in 13 patients who had been treated definitively with radiation therapy and were thought to have no tumor recurrence for 2 years or longer. These patients had been followed prospectively with PFTs approximately every 6 months. PFTs included spirometry with forced expiratory volume in 1 second (FEV 1 ) and forced vital capacity (FVC), diffusing capacity for carbon monoxide (DLCO), and lung volumes. There was a decline in the 6-month median FEV 1 , FVC, and DLCO that reverted to baseline by 1 year. This improvement at 1 year following radiation therapy was attributed to tumor response. However, there was then a yearly reduction in the median FEV 1 , FVC, and the DLCO of 7%, 9.5%, and 3.5%, respectively. The changes in FEV1 and FVC were significant. Ten of these 13 patients developed some new respiratory symptoms that developed at 6 weeks to 21 months following treatment, with a median of 6 months. The authors attributed this progressive decline in PFTs to progressive/evolving radiation-induced lung injury, possibly due to the continuous cycle of tissue hypoxia resulting in an influx of proinflammatory cells that release cytokines that perpetuate the process.
Observations such as this of progressive decline in lung function have resulted in a reluctance of some clinicians to prescribe high-dose radiotherapy to patients with poor pulmonary reserve. However, there is evidence that the extent of decline is linked to pretreatment function such that patients with poor PFTs pretreatment are at less risk of symptomatic lung toxicity or reduction in FVC or FEV 1 compared with patients with good spirometry. These somewhat paradoxic observations suggest that poor PFTs should not by themselves be a contraindication to high-dose radiotherapy.
One prospective study of 185 patients given PFTs before and after thoracic RT found that the median maximal percentage reductions in FEV 1 , uncorrected DLCO (not corrected for hemoglobin levels), and DLCO were 11.5%, 14.9%, and 15.3%, respectively. Reductions in corrected and uncorrected DLCO were larger than that observed for FEV1. Reductions in uncorrected DLCO were associated with the mean lung dose (MLD) and percentage of perfused lung (measured by SPECT) receiving 30 Gy or more (V30). However, the changes in the SPECT scans were relatively smaller than the observed changes in PFTs in many patients. In a later analysis in an expanded group of patients, the correlation between the predicted drop in DLCO and subsequent pneumonitis was not considered high enough to be very clinically useful.
Others have found a significant correlation between preradiation and postradiation therapy DLCO and pulmonary toxicity. In one large institutional retrospective study 85% of patients with NSCLC had a postradiation reduction of DLCO. The mean reduction in pretreatment and posttreatment DLCO was 20%. The proportional drop in DLCO differentiated between patients who developed RP grade 1 versus grade II (common toxicity criteria [CTC] v3). This reduction in DLCO correlated with RP grade ≤1 versus ≥2 in patients who were age 65 years or more, had advanced stage (III–IV vs. I–II), were smokers, received chemotherapy, had V20 Gy ≥ 30% (the percentage of normal lung receiving 20 Gy or more), and had baseline DLCO or FEV 1 equal to or more than 60% of predicted. Patients who had higher proportional reductions in DLCO had significant higher rates of severe RP. However, the reductions in DLCO still varied widely between the grades of RP, making it less useful to use in routine clinical practice.
Radiation Pneumonitis
RP typically presents between 1 to 7 months after treatment of external-beam radiotherapy. Clinical symptoms range from shortness of breath, unproductive cough, and occasionally mild fever to death from respiratory failure. RP is diagnosed in approximately 30% of the patients irradiated with radical intent. In patients with respiratory comorbidity such as chronic obstructive pulmonary disease it is often difficult to distinguish whether an acute episode of cough and dyspnea is related to RP or an (postobstructive) infection, disease progression, or preexisting lung disease. RP has a considerable impact on the patient morbidity (quality of life) and less on mortality.
Cooperative group studies of concurrent chemoradiation therapy in stage III NSCLC using 2-dimensional (2-D) or 3-D CT planning have demonstrated grade 3 or higher RP rates in the range of 8% to 18% ( Table 42.3 ). The lack of clarity as to how toxicity was calculated or graded makes it difficult to compare rates of RP from study to study. The RTOG designed its dose escalation studies with an upper limit of 15% grade 3 or higher toxicity, most of which were pulmonary. Other studies have accepted higher rates of toxicity. In a large institutional experience in patients with stage III disease treated with concurrent chemoradiation with 3-D planning technique, where the incidence of pneumonitis was calculated on an actuarial basis, the risk of symptomatic pneumonitis was more than 30%.
| Study Author (Y) | Treatment | Toxicity Grading | Pneumonitis |
|---|---|---|---|
| SWOG 0023 Kelly et al. (2008) | 61 Gy qd Cisplatin/etoposide | Pulmonary CTCv2 >Gr 3 | 8.3% Overall |
| RTOG 9410 Curran et al. (2011) | 60 Gy qd or 69.6 bid Gy Cisplatin/vinblastine or cisplatin/etoposide | Pulmonary RTOG >Gr 3 | 14% Sequential 15% Concurrent |
| HOG/US Oncology Hanna et al. (2008) | 59.4 Gy Cisplatin/etoposide | Pneumonitis CTCv3 >Gr 3 | 1.4% Concurrent with no consolidation 9.6% Concurrent with consolidation docetaxel |
| CALGB 39801 Vokes et al. (2007) | 66 Gy Carboplatin/paclitaxel | Pneumonitis CTCv2 >Gr 3 | 10% Induction and concurrent 4% Concurrent |
| EORTC 08972-22973 Belderbos et al. (2007) | 66 Gy/24 fx qd | Pneumonitis RTOG/EORTC >Gr 3 | 14% Sequential (gemcitabine-cisplatin) 18% Concurrent (daily dose cisplatin) |
Dosimetric Factors
Estimation of the probability of developing RP after treatment with high-dose RT is important for patients with inoperable lung cancer. An important question is could the lung toxicity be predicted from the delivered dose and historical toxicity models? The total dose for an organ-at-risk after conventional fractionated radiotherapy is calculated as the biologic effective dose or normalized total dose in 2 Gy per fraction (NTD2Gy) according to the linear–quadratic model. Studies of the risk of RP relative to the radiation dose received to a certain volume of “normal” lung have used various theoretic models. These studies were only possible with the adoption of CT planning. In two of these models the dose–volume histogram is first reduced to a single parameter, which is subsequently related to the incidence of radiation pneumonitis. Single parameters are the MLD and the volume of the lung receiving more than a certain threshold dose (Vx). The MLD is defined as the average dose throughout the lungs (minus the gross tumor volume). One of the seminal articles by Graham et al. that studied the risk for 99 lung cancer patients with the incidence of RP found that it was correlated with the percent of normal lung receiving 20 Gy or more (V20). In this analysis Graham subtracted the planning target volume (PTV) from the total bilateral lung volume. The PTV is the volume that contains the gross disease, areas thought to represent microscopic extension with an additional margin to account for daily set-up variation. This method of calculating the V20 was continued in several RTOG radiation dose escalation studies. However, RTOG 0617, which is a phase III study comparing 60 Gy with 74 Gy with concurrent carboplatin/paclitaxel, calculated normal irradiated lung as the total lung minus the clinical target volume, i.e., the volume thought to contain only gross tumor and microscopic extension. Wang et al. demonstrated that the differences in the calculated mean lung dose or other dosimetric parameters varied greatly depending on which formula was used to define “normal lung.” The choice of which of the various formulas to use can lead to significant variation in the prediction of subsequent pulmonary toxicity. The most conservative approach is to subtract only the gross tumor volume (or the internal target volume if using 4-D CT simulation technique). Multiple authors have recommended this approach since the choice of the clinical target volume or PTV margin is more variable from physician to physician.
Marks et al. reviewed over 70 articles that correlated dose–volume parameters with subsequent RP following conventionally fractionated radiation therapy of NSCLC. This review, part of the Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC) initiative, cautioned that there was no MLD below which there was no risk of RP. There is also the issue of overestimating RP in these patients due to exacerbation of preexisting pulmonary comorbidities, or tumor progression producing similar complaints. The correlation of MLD and the risk of RP was not linear but had a mildly exponential increase that was more pronounced with increasing MLD. The risk of symptomatic RP with MLD of 20 Gy and 30 Gy was approximately 20% and 40%, respectively. A significant variation in the risk of RP with increasing normal lung volumes, i.e., V20, V30, etc., was reported within the 14 studies summarized by QUANTEC. For example, for V20 of 30% the reported symptomatic RP varied from less than 10% to approximately 50%. There was less variation among the 10 studies that correlated MLD and subsequent symptomatic RP.
In addition to looking at the radiation dose to the total normal lung, there may also be an association between the ipsilateral normal lung dose and the risk of RP. Ramella et al. found that if the V20, V30, and MLD of the total lung volume did not exceed 31%, 18%, and 20 Gy, respectively, there was additional predictive value to the ipsilateral (affected) lung constraints. For example, if the ipsilateral V20 was 52% or less, the risk of RP was 9%, whereas if it was greater than 52%, the risk of RP was 46%. These dosimetric values were calculated by subtracting the PTV from the ipsilateral affected lung.
The use of intensity modulated radiation therapy (IMRT) has been reported to be associated with less pneumonitis compared with 3-D conformal radiotherapy, but it is difficult to understand why if normal lung parameters such as MLD or V20 are similar. IMRT plans are characterized by a more conformal dose distribution and steeper dose fall off and result in a decrease of the V20 and MLD, although the volume of lung receiving a low dose (V5) will be higher. It has been recommended that contralateral lung V5 be kept below 60% to reduce the risk of potentially fatal pneumonitis.
RTOG 0617, a phase III study comparing 60 Gy versus 74 Gy for locally advanced NSCLC, stratified patients according to 3-D CT or IMRT treatment planning. Preliminary results of this study indicate that quality of life was superior in patients treated with IMRT. There is unlikely to be a phase III study directly comparing 3-D CT and IMRT treatment planning. A population-based study of comparative effectiveness found similar rates of early and late pulmonary toxicity for both techniques.
Fewer studies have been done to predict the risk of RP following treatment of limited SCLC. However, there is likely a similar correlation between the dosimetric factors and subsequent RP. For example, Tsujino et al. looked at the risk of RP in patients with limited small cell lung cancer (SCLC) who were treated with cisplatin-based chemotherapy and concurrent thoracic radiation of 45 Gy given two fractions daily, over 15 treatment days. The 12-month cumulative incidence of symptomatic RP was 0%, 7.1%, 25%, and 42.9% in patients with a V20 of <20%, 21% to 25%, 26% to 30%, and >31%, respectively.
Clinical Factors
The impact of nondosimetric factors in predicting the risk of RP has been an area of intense study. Appelt et al. analyzed the patient data used to make the QUANTEC recommendations to look for clinical risk factors. Factors found to significantly increase the risk of RP were preexisting pulmonary comorbidity, mid or inferior tumor location, current smoking, age older than 63 years, and sequential (as opposed to concurrent) chemotherapy.
Other studies have found that sequential or concurrent chemotherapy involving cisplatin/etoposide does not appear to increase the risk of RP. RTOG 8808/ECOG 4588 was a three-arm phase III study comparing radiation only, 60 Gy in 2 Gy daily fractions (considered “standard”), or 69.6 Gy in 1.2 Gy fractions twice daily, or sequential cisplatin/vinblastine chemotherapy and standard radiation therapy. The 18-month cumulative incidence of toxicity, primarily pulmonary, was almost 30% in the combined modality arm, as compared with 20% to 25% incidence in the radiation therapy–only arms. The statistical significance between the pulmonary toxicity in the various arms is not stated although the authors said the toxicity was acceptable. Most of the toxicity occurred within the first 3 to 6 months in all treatment arms, with a relative flattening of the incidence after 9 months.
Given the difference from study to study in the nondosimetric variables predicting the risk of pneumonitis, meta-analyses have been done. Vogelius et al. reviewed the English language lung cancer literature between 1990–2010 in which RP was correlated with some patient or treatment variables. In the 31 studies analyzed, the statistically significant risk factors for increased RP were older age, mid-lower lung disease location, and presence of pulmonary comorbidity. The use of sequential rather than concurrent chemotherapy was found to increase the risk of RP but the authors suspected this was likely due to patient selection rather than a “real” predictive factor. Interestingly, smoking at the time of treatment was found to protect against RP. Even a prior history of smoking was associated with a decreased risk of RP, although this did not reach statistical significance.
Patients with collagen vascular diseases (CVD) are likely at increased risk of RP. In an excellent review by Lee et al. it appears that cytokines such as TGF-β are chronically elevated in such patients. There is often preexisting lung fibrosis. Radiation therapy may cause a patient with quiescent CVD to develop active CVD. These patients are also noted to have increased late toxicity as compared with patients without CVD. Lung fibrosis may extend outside of the high-dose region, so treatment volumes should be reduced when possible, although there is no reason to omit radiation therapy if it is indicated. Interestingly, tumors developing in patients with CVD may be more radiosensitive, prompting consideration of a radiation dose reduction of at least 10%.
Combined Dosimetric and Clinical Factors
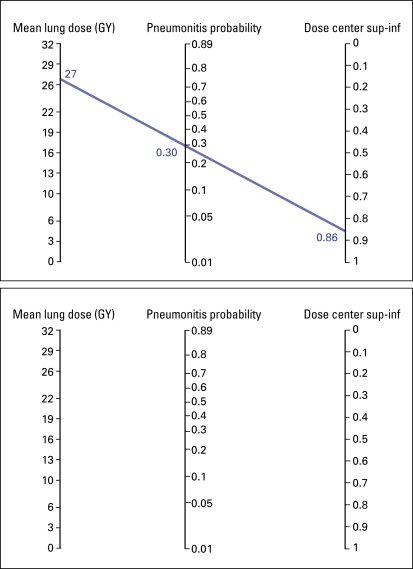
Dosimetric and nondosimetric factors can be combined to increase the ability to predict RP. Bradley et al. proposed a nomogram to predict RP based on mean lung dose and the tumor location, superior to inferior ( Fig. 42.2 ).
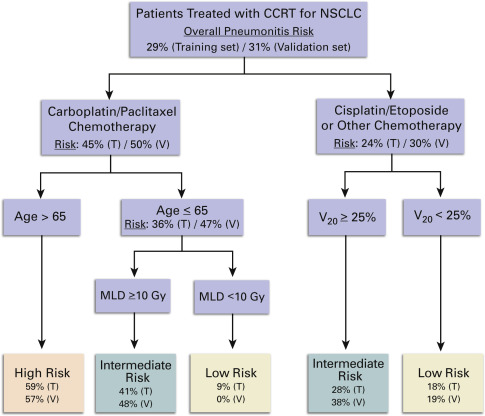
Taking it one step further, Palma et al. performed a meta-analysis of both dosimetric and nondosimetric factors based on individual patient data. The authors did a search of articles published between 1993 and 2010, in which clinical and dosimetric factors of patients treated with concurrent chemoradiation therapy were available to be correlated with RP. These data were then utilized to conduct a recursive partitioning analysis (RPA) from a 557-patient dataset, and then the RPA was validated using another 279-patient dataset. Factors predicting greater risk of pneumonitis were carboplatin/paclitaxel chemotherapy (vs. cisplatin/etoposide), age greater than 65 years, V20, and MLD ( Fig. 42.3 ).
Biomarkers
Inflammatory cytokines are made by many cells within the lung, including the alveolar macrophages, type II pneumocytes, T lymphocytes, and lung fibroblasts. The blood levels of these cytokines pre-RT, during, and post-RT have been an area of intense interest. For example, Chen et al. found that circulating IL-6 levels pre-RT, during, and post-RT have been correlated with an increased risk of RP. In that study, TNF, another inflammatory cytokine, was not associated with an increased risk of RP.
TGF-β1 is a cytokine that has been extensively studied as a marker predictive of RP. It was noted that patients with NSCLC have increased pretreatment levels of TGF-β1 and that increased levels were associated with a higher MLD and a higher incidence of RP. Several studies showed that the absolute levels of TGF-β1 were not as predictive of RP as the observation of an increasing ratio of pretreatment to intratreatment TGF-β1 for stage III NSCLC treated with definitive radiation, with or without chemotherapy. The predictive value of the TGF-β1 ratio was even higher when combined with the MLD. The combination of a MLD of more than 20 Gy and a TGF-β1 ratio of more than 1 was associated with a 66% incidence of RP. Similarly, IL-8 levels pretreatment and then at weeks 2 and 4 of radiation therapy were associated with RP. Patients with RP grade 2 or higher tended to have higher baseline IL-8 levels and these had a slight downward trend during radiation therapy, as opposed to low and stable IL-8 levels in patients without RP. Combining IL-8, TGF-β1, and MLD into a single model led to an improved ability to predict RP as compared with either variable alone.
Certain polymorphisms of the VEGF gene have been correlated with the incidence and severity of RP.
Recall Radiation Pneumonitis
Recall RP is when symptoms of RP are activated by administration of a drug sometime after completion of radiotherapy, with worse than expected RP. Recall RP has been associated with multiple chemotherapy drugs such as taxanes, gemcitabine, vinca alkaloids, doxorubicin, and epirubicin. Tyrosine kinase inhibitors such as erlotinib and sunitinib have also been associated with radiation recall pneumonitis and increased risk of severe RP following palliative or definitive radiation therapy.
Prevention and Management
Amifostine
Amifostine, a thiol derivative, is a scavenger of free radicals generated during radiation therapy. Other possible mechanisms of action include increasing the consumption of oxygen within the cells and condensation of DNA, making the strands more resistant to free radicals. A small phase III study in stage III NSCLC patients given radiation and concurrent chemoradiation therapy (paclitaxel or carboplatin) found a significant decrease in the rate of symptomatic RP. The rate of grade 3 or higher (RTOG grading system) in the amifostine versus nonamifostine arms was 56.3% and 19.4%, respectively ( p = .002). However, a larger phase III study, RTOG 9801, investigated the ability of amifostine to reduce chemoradiation-induced esophagitis. Amifostine did not reduce treatment-related esophagitis in that study when it was given daily with carboplatin/paclitaxel and concurrent thoracic radiation for stage III NSCLC. A subsequent report indicated that amifostine also did not reduce either median survival or late toxicities, including RP.
Pentoxifylline and Vitamin E
The combination of pentoxifylline and vitamin E has been shown to decrease radiation-related soft-tissue fibrosis of the breast and extremities. Pentoxifylline is a methylxanthine derivative developed and prescribed for impaired microcirculation. It improves blood perfusion by erythrocyte deformability and decreased blood viscosity. Pentoxifylline appears to decrease fibroblast, cellular matrix, and collagen production by blocking the activity of TNF, decreasing IL and oxygen radicals, and stimulating collagenase activity. Vitamin E, a tocopherol, acts as an antioxidant and protects membrane phospholipids from oxidative damage by scavenging reactive oxygen species generated during oxidative stress. Vitamin E also inhibits TGF and collagen production.
A small randomized study of pentoxifylline 400 mg versus placebo three times a day during radiation therapy for either lung or breast cancer demonstrated superiority in the pentoxifylline arm in the posttreatment patient-reported breathing function, DLCO, and imaging studies. Larger studies should be done to validate this finding.
Steroids
Surprisingly, there has been little clinical research into the use of prophylactic steroids to reduce the incidence and severity of RP. A rodent study found that small doses of steroids three times a week for 15 weeks starting 10 to 11 weeks from delivery of thoracic radiation significantly delayed the onset of and death due to RP. A prospective study in humans would be clinically relevant.
Angiotensin-Converting Enzyme Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors have been studied in both animals and humans. The mechanism of its protective effect is not clear but may have something to do with the reduction in pulmonary arterial pressure, resulting in less severe edema. Rodent studies established the rationale for angiotensin-converting enzyme inhibitors, such as captopril, in the reduction of acute pneumonitis following radiation therapy. This effect was most notable at moderate doses of radiation therapy. Following very high doses of hemithoracic radiation, i.e., 80 Gy in 10 fractions, captopril had no significant protective effect. Retrospective studies also confirmed the apparent protective effect of ACE inhibitors on pulmonary toxicity following concurrent chemoradiation for stage III NSCLC. A phase II cooperative group study (RTOG 0213) was initiated to test this hypothesis but closed due to poor accrual. The study was designed to test the ability of captopril to alter the incidence of pulmonary damage at 12 months from completion of radiation treatment in SCLC or NSCLC patients receiving at least 45 Gy.
TGF-β Tyrosine Kinase Inhibitors
There are no human clinical studies of inhibitors of TGF-β to reduce RP, but preclinical studies suggest potential utility. Flechsig et al. found that a 4-week course of a tyrosine kinase inhibitor to TGF-β improved the survival of rodents following whole thoracic radiation.
Treatment of Radiation Pneumonitis
There are no prospective studies evaluating the effectiveness of treatment of RP. Most cases are self-limiting. Patients with troublesome symptoms from presumed RP are usually started on prednisone 50–60 mg per day for 1–2 weeks and then decreased slowly by 10 mg per week, assuming the symptoms are improved or stable. Oxygen may be needed and a referral to a pulmonologist should be considered if the symptoms are severe or do not improve as anticipated.
Esophagus Toxicity
Pathophysiology
Radiation-induced esophagitis is an inflammation of the esophagus, which develops 2 to 3 weeks after the initiation of radiation therapy. Radiation affects the part of the esophagus within the irradiated area. The normal esophageal mucosa undergoes continuous cell turnover and renewal. These mucosal cells are sensitive to irradiation-induced damage. Acute radiation esophagitis is primarily due to effects on the basal epithelial layer. This causes a thinning of the mucosa, which can progress to denudation.
In 1960, the onset of radiation effects in the esophagus was first studied in rats and displayed timelines and clinical findings. Four days after radiation a submucosal infiltration of leucocytes was seen, mucosal necrosis was seen at 7 days, and a moderate inflammation of the muscularis of the esophagus and some submucosal telangiectasia was seen 10 days after radiation. By 20 days most of the rats showed reepithelization of the esophagus. However, in animals killed more than 3 months after exposure, defects in the muscle walls and atrophy of the epithelium were seen.
Grading of Esophagus Toxicity
Esophagus toxicity is scored using the CTCAE (version 4.0). Grade 2 is scored in case of symptomatic dysphagia and altered eating and intravenous fluids may be indicated for a period shorter than 24 hours. Grade 3 esophagus toxicity is scored in case of symptomatic and severely altered eating/swallowing and the use of intravenous fluids, tube feedings, or total parenteral nutrition equal to or more than 24 hours. Grade 4 esophagus toxicity includes life-threatening consequences for the patients, and grade 5 is scored in case of death. The CTC scoring system, however, does not differentiate between early and late symptoms. The RTOG/EORTC scoring system differentiates between acute esophagus toxicity (AET), symptoms within 3 months after concurrent chemoradiation therapy, and late esophagus toxicity (LET), symptoms persisting or occurring more than 3 months after the end of treatment ( Table 42.4 ). AET influences the quality of life of the patient and may result in treatment interruption, but generally resolves after treatment. Patients who develop esophagus stenosis, perforation, or fistula are categorized as severe LET (grade 3–5). Severe LET seriously affects the patients’ quality of life or even leads to death. Although several models are available to predict the incidence and severity of AET, for LET predictive models are sparse. So far, several studies have reported the incidence of severe LET using 3-D–conformal-radiotherapy (3DCRT) and IMRT ( Table 42.5 ). Using 3DCRT, the reported crude incidence of severe LET in concurrent RCT varies from 5% to 16%. Without solid evidence, several implications can be drawn from previous studies: severe AET is associated with severe LET.
| Grade 0–1 | Mild fibrosis; slight difficulty in swallowing solids; no pain on swallowing. |
| Grade 2 | Unable to take solid food normally; swallowing semisolid food; dilatation may be indicated. |
| Grade 3 | Severe fibrosis; able to swallow only liquids; may have pain on swallowing; dilatation required. |
| Grade 4 | Necrosis/perforation fistula. |
| Grade 5 | Death. |
| Author (Y) | Patients | Radiotherapy | Chemotherapy | Criteria | Median Follow-Up (Mo) | Median Overall Survival (Mo) | Crude Incidence LET |
|---|---|---|---|---|---|---|---|
| Byhardt et al. (1998) | Stage II, IIIA/B N = 136 | 3DCRT 60 Gy/6 wk (QD) | Sequential | RTOG | — | 13.6 | 2% ≥G3 LET |
| N = 82 | 3DCRT 63 Gy/6.5 wk | Sequential/Concurrent | RTOG | — | 16.3 | 4% ≥G3 LET | |
| N = 170 | 3DCRT 69.6 Gy/6 wk (BID) | Concurrent | RTOG | — | 15.8 | 8% ≥G3 LET | |
| Maguire et al. (1999) | Stage I∼IIIA/B N = 66 | 3DCRT 64.2∼85.6 Gy (QD/BID) | None/Sequential/Concurrent | RTOG | — | — | 3% ≥G3 LET |
| Uitterhoeve et al. (2000) | T1∼T4, N0∼N2 N = 40 | 3DCRT 60.5∼66 Gy/30∼32 d (Hypo) | Concurrent | RTOG | 21 | 13.5 | 5% ≥G3 LET |
| Rosenman et al. (2002) | Stage IIIA/B N = 62 | 3DCRT 60∼74 Gy (QD) | Sequential + Concurrent | RTOG | 43 | 24 | 6% ≥G3 LET |
| Komaki et al. (2002) | Stage II, IIIA/B N = 81 | 3DCRT 63 Gy/7 wk (QD) | Sequential + Concurrent | RTOG | — | 16.4 | 4% ≥G3 LET |
| N = 82 | 3DCRT 69.6 Gy/6 wk (BID) | Concurrent | RTOG | — | 15.5 | 16% ≥G3 LET | |
| Singh et al. (2003) | N2/N3, T3/T4 N = 207 | 3DCRT 60∼74 Gy (QD) | None/Sequential/Concurrent | RTOG | 24 | — | 6% ≥G3 LET |
| Bradley et al. (2004) | Stage I∼IIIA/B N = 166 | 3DCRT 60∼74 Gy (QD) | None/Sequential/Concurrent | RTOG | — | — | 3% ≥G3 LET |
| Belderbos et al. (2007) | Stage I∼IIIA/B N = 76 | 3DCRT 66 Gy/30∼32 d (Hypo) | Sequential | RTOG | 39 | 16.2 | 4% ≥G3 LET |
| N = 66 | 3DCRT 66 Gy/30∼32 d (Hypo) | Concurrent | RTOG | 39 | 16.5 | 5% ≥G3 LET | |
| van Baardwijk et al. (2012) | Stage III N = 137 | 3DCRT 51∼69 Gy (BID + QD) | Concurrent | CTCAE | 30.9 | 25.0 | 7.3% ≥G3 LET |
| Chen et al. (2013) | Stage II∼IIIA/B N = 171 | IMRT 66 Gy/30∼32 d (Hypo) | Concurrent | RTOG/EORTC | 33 | 24 | 6% ≥G3 LET |
Radiation Esophagitis
The improved survival of patients with locally advanced NSCLC who are treated with concurrent radiochemotherapy comes at a price of increased esophagus toxicity. Due to overlap with the target volume because of involvement of mediastinal lymph nodes or mediastinal tumor invasion a part of the esophagus is often irradiated in lung cancer. Acute toxicity is manifested clinically as dysphagia, odynophagia, and substernal discomfort and usually occurs within 2 to 3 weeks after the initiation of radiation therapy. Patients may describe a sudden, sharp, severe chest pain radiating to the back. Patients with insufficient intake due to radiation esophagitis are at risk for premature discontinuation of therapy. Predicting the risk of esophagus toxicity makes it possible to take appropriate precautions, such as preventive medication or tube feeding. Identifying the low-risk patients for radiation esophagitis gives the opportunity to escalate the dose of radiotherapy to improve tumor control.
Dosimetric Factors
Estimation of the probability and severity of esophagus toxicity after concurrent chemoradiation treatment is crucial. This allows the individual prescription of tumor doses based on normal tissue complication probabilities. Several prediction models have been reported to estimate the risk of AET based on the planned dose distributions. Currently used models to predict AET in lung cancer patients after intensity IMRT and concurrent chemotherapy were mainly derived from patients treated with 3-D chemoradiation.
When using IMRT and concurrent chemoradiation in patients with NSCLC, reported were a dose–effect relationship of AET in 185 patients, severe LET in 171 patients, and dose–volume parameters of the esophagus. Severe LET was defined as grade equal to or greater than 3 RTOG/EORTC ( Table 42.6 ). In these Dutch studies, hypofractionated IMRT treatment up to 66 Gy in 24 fractions and concurrent daily low-dose cisplatin (6 mg/m 2 with a maximum of 12 mg) was administered in consecutive patients. Cisplatin was administered as a bolus injection 1 hour to 2 hours before each fraction. The dose distributions were first converted to normalized total doses to account for fractionation effects with an α/β-ratio of 10 Gy for AET and α/β-ratio of 3 Gy for LET. Equivalent uniform dose (EUD) to the esophagus and the volume percentage receiving more than x Gy (Vx) were evaluated by the Lyman-Kutcher-Burman model. A total of 22% patients with NSCLC developed AET toxicity greater than or equal to grade 3, and 6% severe LET was observed. The median time to AET grade 3 was 30 days, with a median duration of >80 days. The median onset time of severe LET was 5 months (range 3∼12). All 11 patients expressed LET within 1 year. Eight patients developed esophagus stenosis (grade 3), which could be treated by dilatation. A fistula was diagnosed in three patients, and these patients were treated with intraluminal stent. All three patients with fistulae died from respiratory insufficiency caused by pneumonia shortly after the stent was placed (up to 3 months). Pathologically proven tumor progression was the cause of esophageal fistulae in three other patients (28, 31, and 31 months) and not scored as LET. Severe LET occurred in 7% of the patients (4 of 61) with grade 2 AET and 19% of the patients (7 of 37) with grade 3 AET. Severe LET was significantly ( p = 0.002) associated with the maximum grade of AET. Patients with unrecovered AET had a significantly ( p < 0.001) higher risk of developing severe LET, compared with patients without AET or with a recovered AET. In the EUD, n = 0.03 model, all severe LET patients had a NTD greater than 70 Gy on the esophagus. In the EUDn-LKB model, the fitted values and 95% confidence intervals (CIs) were TD50 = 76.1 Gy (73.2∼78.6), m = 0.03 (0.02∼0.06) and n = 0.03 (0∼0.08). In the Vx-LKB model, the fitted values and 95% CIs were Tx50 = 23.5% (16.4∼46.6), m = 0.44 (0.32∼0.60) and x = 76.7 Gy (74.7∼77.5).