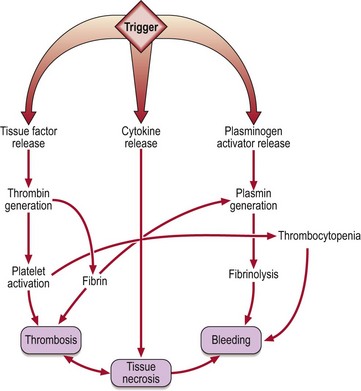
38 DIC is a complex clinical syndrome which complicates many serious illnesses (Table 38.1). It is characterised by intravascular deposition of fibrin and accelerated degradation of fibrin and fibrinogen caused by excess activity of proteases, notably thrombin and plasmin, in the blood (Fig 38.1). DIC is heterogeneous both in its pathophysiology and clinical manifestations. In most cases it probably begins when circulating blood is exposed to tissue factor released from damaged tissues, malignant cells or injured endothelium. This in turn leads to generation of thrombin which causes formation of soluble fibrin, activation of circulating platelets, and secondary fibrinolysis. Table 38.1 DIC can cause bleeding, large vessel thrombosis and haemorrhagic tissue necrosis (Fig 38.2). The coagulation defect arises from consumption of coagulation factors and platelets and increased fibrinolytic activity. In clinical practice acute DIC usually presents as widespread bleeding in an ill patient. Oozing of blood from cannulation sites is characteristic. Microthrombus formation can lead to irreversible organ damage; the kidney, lungs and brain are frequent targets. DIC is not necessarily a fulminant syndrome; more chronic forms may be seen particularly in association with malignancy (e.g. prostatic carcinoma).
Acquired disorders of coagulation
Disseminated intravascular coagulation (DIC)
Acquired disorders of coagulation