VARIABLES ROUTINELY MEASURED IN THE ANALYSIS OF THE BIOPSY SPECIMEN
An abundance of quantitative information may be obtained from the biopsy. Because the morphometric analysis is a labor-intensive process, the number of variables evaluated depends on whether the biopsy specimen is being analyzed for diagnostic or research purposes. Listed below are eight indices of trabecular bone that are of particular clinical relevance. A detailed account of the complete analysis of bone biopsy specimens is found in more specialized texts.2,11
The histomorphometric parameters are generally divided into two categories. Static variables provide information on the amount of bone present and the proportion of bone surface engaged in a particular phase of remodeling activity. Dynamic variables yield information on the rate of cell-mediated processes involved in remodeling. This category can be evaluated only in biopsy specimens that have been appropriately labeled with tetracycline. Importantly, inferences about the rate of cellular activities can be made only from an analysis of the dynamic variables. An increase in resorption surface, a static variable, does not necessarily indicate an increase in resorption rate. The bone formation rate may be calculated directly from selected dynamic variables measured in an appropriately labeled biopsy specimen. Resorption rate, on the other hand, can be computed only indirectly, using certain indices of bone formation, in a single biopsy specimen or from two sequential biopsy specimens.11,12
STATIC VARIABLES
The following variables are categorized as static. The terms and abbreviations used are consistent with the recommendation of the Bone Histomorphometry Nomenclature Committee of the American Society for Bone and Mineral Research.13
Cancellous bone volume (Cn-BV/TV, %). This is the fraction of a given volume of whole cancellous bone tissue (i.e., bone + marrow) that consists of mineralized and nonmineralized bone.
Osteoid volume (OV/BV, %). This is the fraction of a given volume of bone tissue (mineralized bone + osteoid) that is osteoid (i.e., unmineralized matrix).
Osteoid surface (OS/BS, %). This is the fraction of the entire trabecular surface that is covered by osteoid seams. Osteoid thickness (O.Th, μm). This is the average width of the osteoid seams.
Eroded surface (ES/BS, %). This is the fraction of the entire trabecular surface that is occupied by resorption bays (Howship lacunae), including both those with and without osteoclasts.
The following variables are categorized as dynamic.
Mineral apposition rate (MAR, μm per day). This is calculated by dividing the average distance between the first and second tetracycline labels by the time interval (e.g., 12 days) separating them. It is a measure of the linear rate of production of calcified bone matrix by the osteoblasts.
Mineralizing surface (MS/BS, %). This is the fraction of trabecular surface bearing double tetracycline labels plus one-half of the singly labeled surface. It is a measure of the proportion of bone surface on which new mineralized bone was being deposited at the time of tetracycline labeling. Bone Formation Rate (BFR/BS, μm3/μm2 per day). This is the volume of mineralized bone made per unit surface of trabecular bone per year. It is calculated by multiplying the mineralizing surface by the mineral apposition rate.
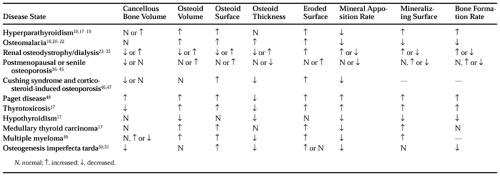
Table 55-1 indicates how each of these variables is altered in different disease states.
NORMAL BONE REMODELING
Bone is remodeled continuously throughout life—old, worn out bone is replaced by new bone. Approximately 25% of trabecular bone and 3% of cortical bone is replaced annually. The remodeling process is a quantum phenomenon because it occurs in discrete units or “packets.” Osteoclasts resorb a preprogrammed volume of old bone. Shortly thereafter, the osteoclasts are replaced by osteoblasts, which refill the resorption cavity with a new packet of bone. The group of cells (osteoclasts and osteoblasts) that creates one new packet of bone is called a bone remodeling unit. In normal trabecular bone, ˜900 bone remodeling units are activated each day. In cortical bone, the activation frequency is ˜180 per day.2,14,15 and 16
HYPERPARATHYROIDISM
Elevated circulating levels of parathyroid hormone (PTH) stimulate the activation frequency of bone remodeling units, resulting in increased numbers of osteoclasts in bone and, because of the coupling process, increased numbers of osteoblasts. Consequently, quantitative analysis of a biopsy specimen from a patient with either primary or secondary hyperparathyroidism reveals increases in eroded surface, osteoid surface, and mineralizing surface (see Fig. 55-4).10,17,18 and 19 The extension of surface double labeled by tetracycline has allowed precise determination of the mineral apposition rate, which has been shown to be reduced. Because the osteoid thickness is normal in this disorder, the reduction in mineral apposition rate indicates a decreased rate of organic matrix production by the osteoblasts, rather than a defect in calcification. However, the extension of mineralizing surface overcompensates for the decrease in mineral apposition rate, so that the overall bone formation rate, the product of these two variables, is still increased. Thus, in hyperparathyroidism, bone resorption and formation rates are increased, which is a situation commonly referred to as a “high turnover” state. Bone turnover is higher in hyperthyroid patients with vitamin D insufficiency.18a Despite the rapid remodeling that occurs in primary hyperparathyroidism, the balance between resorption and formation is generally conserved because cancellous bone volume is normal or may even be increased, and trabecular connectivity is preserved.19 Often accompanying the increased bone turnover rate are increased deposition of immature (woven) bone and marrow fibrosis. These features are particularly prominent in severe secondary hyperparathyroidism.
Because the hallmarks of excessive remodeling activity (e.g., increased eroded surface) accumulate in bone over time, the biopsy can be a sensitive indicator of parathyroid gland hyper activity, especially when this is mild or intermittent. However, the biopsy alone does not distinguish between primary and secondary hyperparathyroidism.
OSTEOMALACIA
Numerous causative mechanisms underlie osteomalacia (see Chap. 63 and Chap. 70). Most of the mechanisms involve processes that decrease the circulating calcium × phosphate product below the levels required for bone mineralization. Although calcification of the organic matrix is inhibited, the osteoblasts continue to synthesize and secrete the matrix. An accumulation of unmineralized matrix (“osteoid”) results (Fig. 55-6). The cancellous bone volume is normal in osteomalacia, but as the osteoid volume is increased, the amount of mineralized bone is actually reduced.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree