REGULATION OF VITAMIN D METABOLISM
Part of “CHAPTER 54 – VITAMIN D“
The metabolic activation of vitamin D is subject to both coarse-and fine-control mechanisms operating at the principal enzymatic steps.17 Hepatic 25-hydroxylation is more efficient at low levels of substrate, and the absolute amount of 25(OH)D in the circulation declines when the supply of vitamin D increases. Nevertheless, the degree of regulation of 25(OH)D synthesis is not sufficient to prevent vitamin D intoxication after the ingestion of large amounts of vitamin D.18
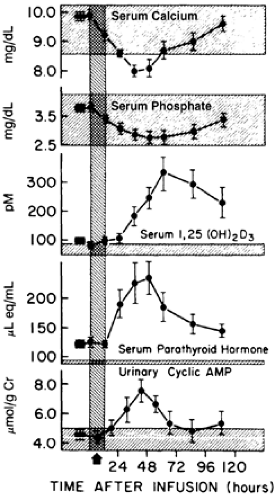
In contrast to the relatively coarse control of hepatic 25- hydroxylation, renal 1 α-hydroxylation is regulated strictly and represents the most important regulatory mechanism in the metabolism of vitamin D. In normal adults, serum concentrations of 1,25(OH)2D change little in response to repeated dosing with vitamin D, and remain normal or even decline in vitamin D intoxication. The three major factors that regulate the enzyme’s activity are blood parathyroid hormone (PTH), calcium, and phosphorus.
PARATHYROID HORMONE
Parathyroid hormone is the main hormonal stimulus for 1 α-hydroxylation, increasing systemic 1,25(OH)2D levels after administration to human research subjects.19 Hypocalcemia also stimulates 1 α-hydroxylation, but this effect is achieved largely through a feedback loop (see Chap. 58) involving the parathyroid glands17; hypocalcemia stimulates PTH secretion, which raises serum 1,25(OH)2D concentrations. 1,25(OH)2D enhances calcium absorption, and the increased serum calcium concentration then inhibits PTH secretion (Fig. 54-4). Some experimental studies suggest that the extracellular calcium concentration can directly influence the renal 1 α-hydroxylase.
PHOSPHORUS
The blood phosphorus concentration is the third major control factor. In rats and in humans, hypophosphatemia stimulates 1 α-hydroxylase activity and increases the 1,25(OH)2D concentration in serum, whereas hyperphosphatemia inhibits formation of the metabolite (see Fig. 54-4). This adaptive effect does not depend on PTH, but it may require insulin-like growth factor-I.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree