The classification applies only to carcinomas and concerns the male as well as the female breast. There should be histological confirmation of the disease. The anatomical subsite of origin should be recorded but is not considered in classification. In the case of multiple simultaneous primary tumours in one breast, the tumour with the highest T category should be used for classification. Simultaneous bilateral breast cancers should be classified independently to permit division of cases by histological type. The regional lymph nodes are: Any other lymph node metastasis is coded as a distant metastasis (M1), including cervical or contralateral internal mammary lymph nodes. Note Note Note Note Note Note Excisional biopsy of a lymph node or biopsy of a sentinel node, in the absence of assignment of a pT, is classified as a clinical N, e.g., cN1. Pathologic classification (pN) is used for excision or sentinel lymph node biopsy only in conjunction with a pathologic T assignment. The pathological classification requires the examination of the primary carcinoma with no gross tumour at the margins of resection. A case can be classified pT if there is only microscopic tumour in a margin. The pT categories correspond to the T categories. Note The pathological classification requires the resection and examination of at least the low axillary lymph nodes (level I) (see page 2). Such a resection will ordinarily include 6 or more lymph nodes. If the lymph nodes are negative, but the number ordinarily examined is not met, classify as pN0. Note Post‐treatment ypN Note Not clinically detected is defined as not detected by imaging studies (excluding lymphoscintigraphy) or not detected by clinical examination. Note
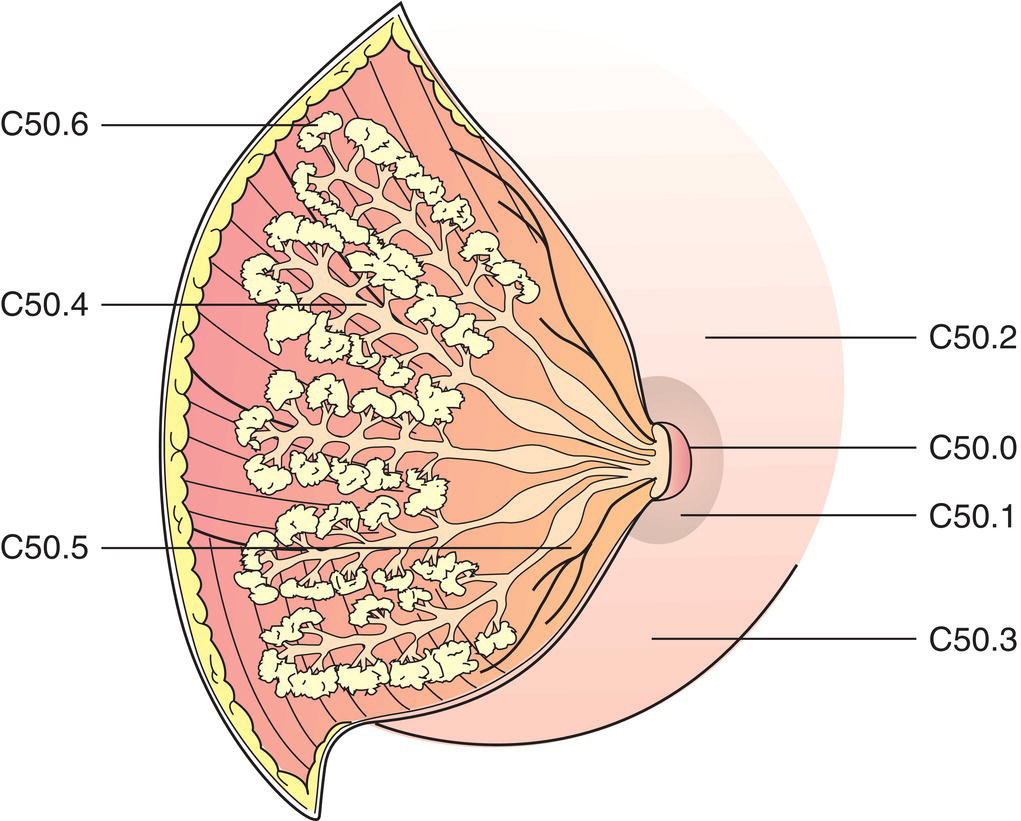
BREAST TUMOURS (ICD‐O‐3 C50)
Rules for Classification
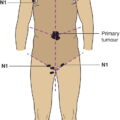
Anatomical Subsites (Fig. 378)
Regional Lymph Nodes (Fig. 379)
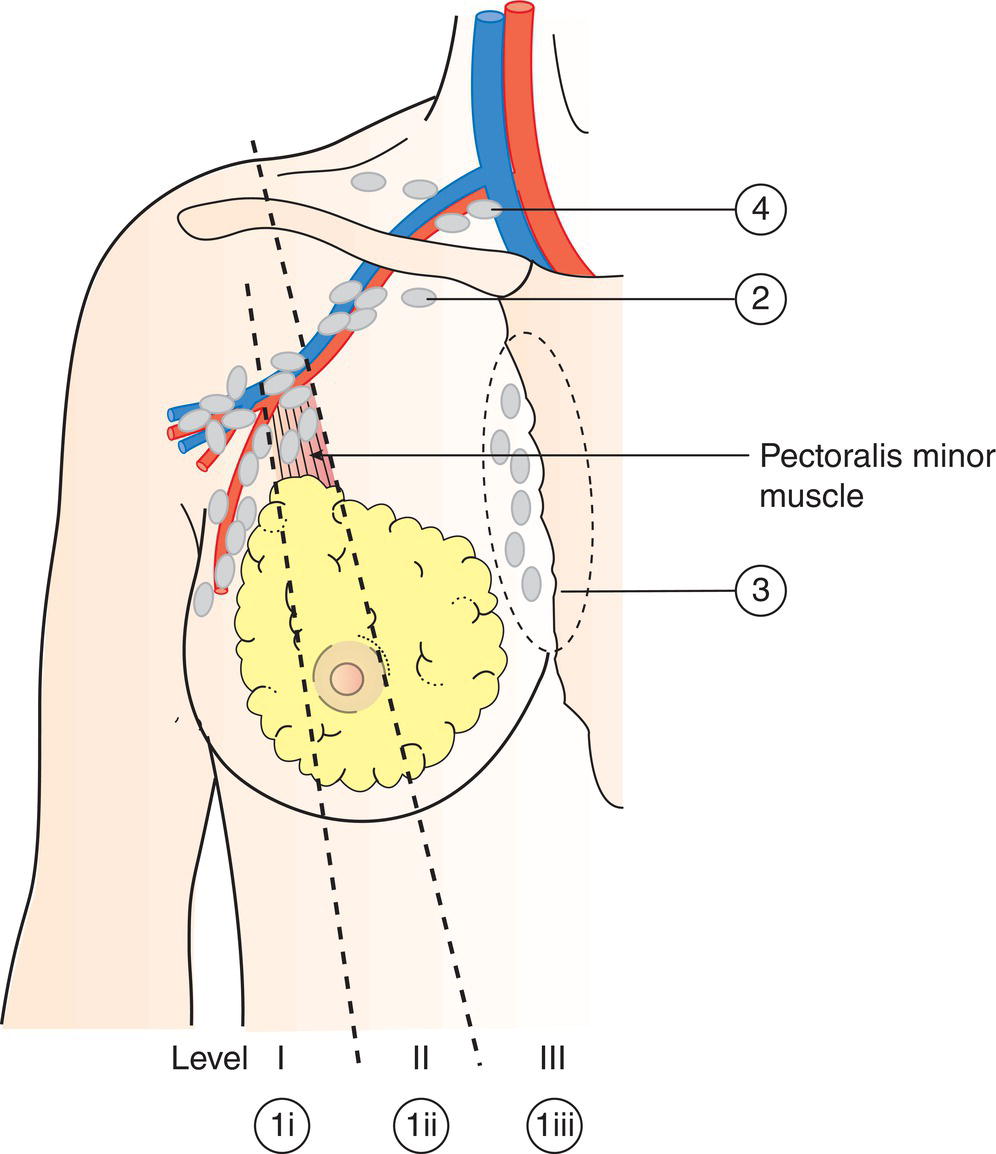
Intramammary lymph nodes are coded as axillary lymph nodes level I.
TNM Clinical Classification
T – Primary Tumour
TX
Primary tumour cannot be assessed
T0
No evidence of primary tumour
Tis
Carcinoma in situ
Tis (DCIS)
Ductal carcinoma in situ
Tis (LCIS)
Lobular carcinoma in situ
Tis (Paget)
Paget disease of the nipple without detectable tumour (Fig. 380)
Tis (Paget) is not associated with invasive carcinoma and/or carcinoma in situ (DCIS and/or LCIS) in the underlying breast parenchyma. Carcinomas in the breast parenchyma associated with Paget disease are categorized based on the size and characteristics of the parenchymal disease, although the presence of Paget disease should still be noted.
T1
Tumour 2 cm or less in greatest dimension
T1mi
Microinvasion 0.1 cm or less in greatest dimension (Fig. 381) 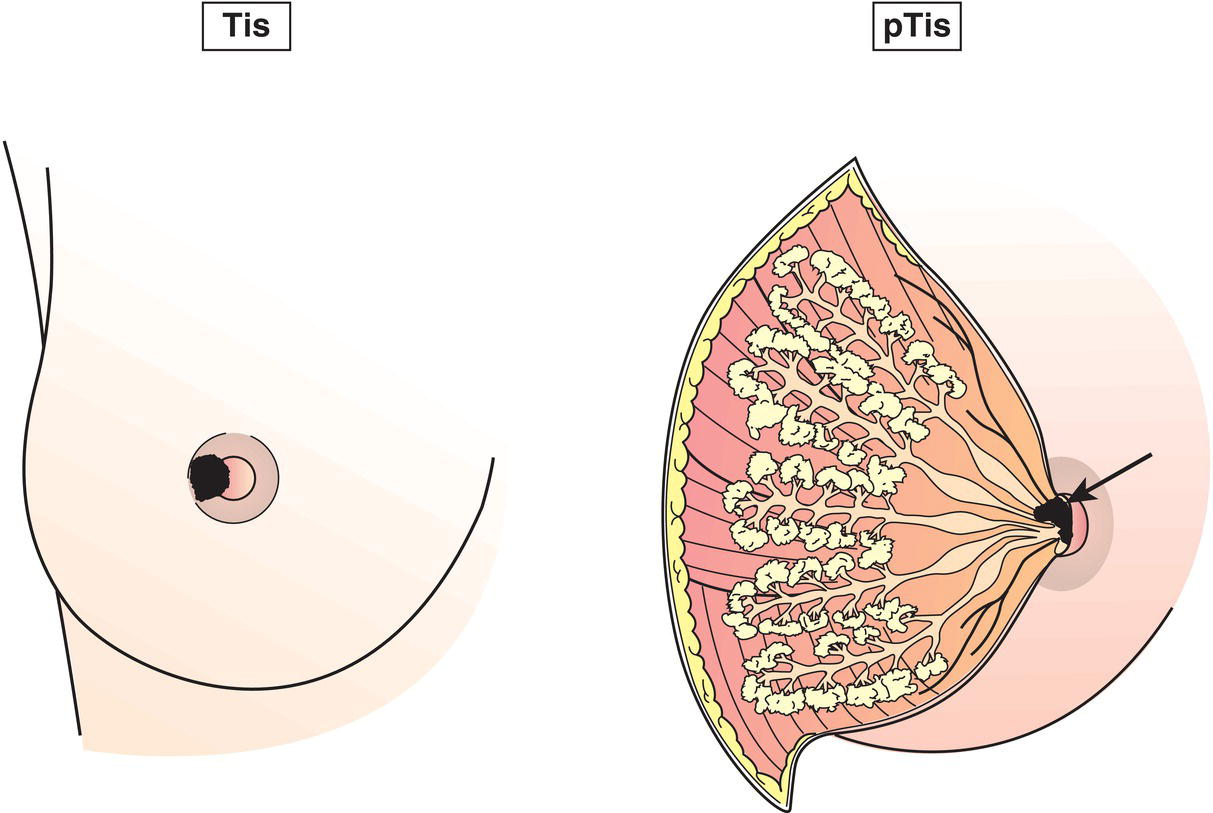
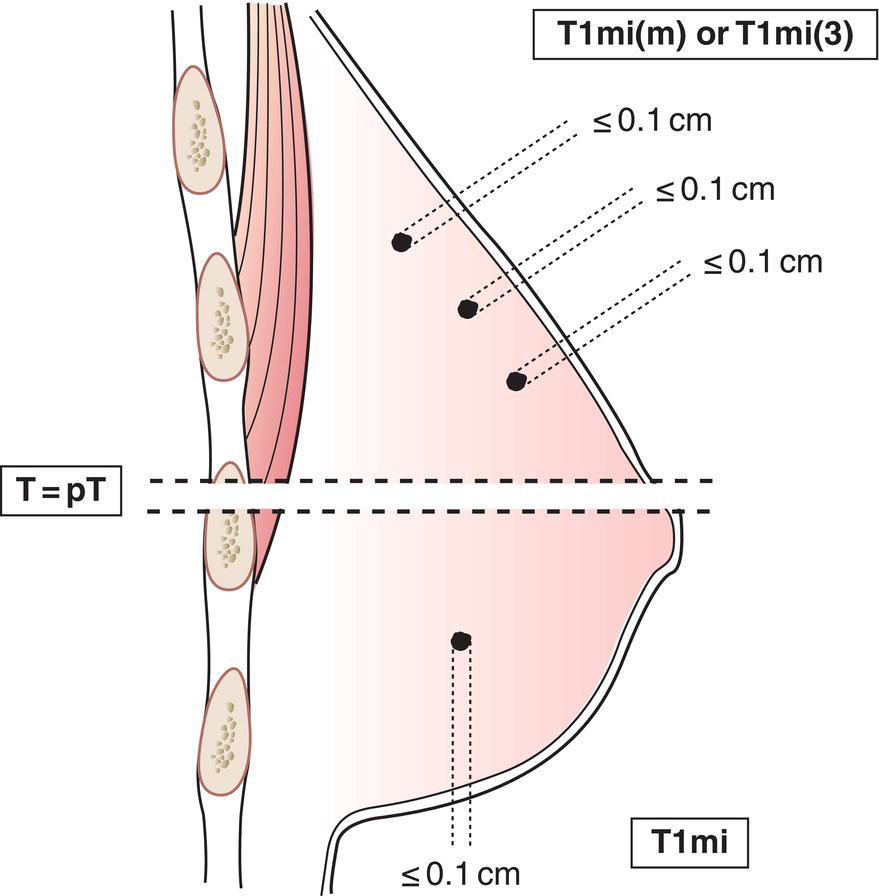
Microinvasion is the extension of cancer cells beyond the basement membrane into the adjacent tissues with no focus more than 0.1 cm in greatest dimension. When there are multiple foci of microinvasion, the size of only the largest focus is used to classify the microinvasion. (Do not use the sum of all individual foci.) The presence of multiple foci of microinvasion should be noted, as it is with multiple larger invasive carcinomas.
T1aMore than 0.1 cm but not more than 0.5 cm in greatest dimension (Fig. 382)
T1b More than 0.5 cm but not more than 1 cm in greatest dimension (Fig. 382)
T1c More than 1 cm but not more than 2 cm in greatest dimension (Fig. 382)
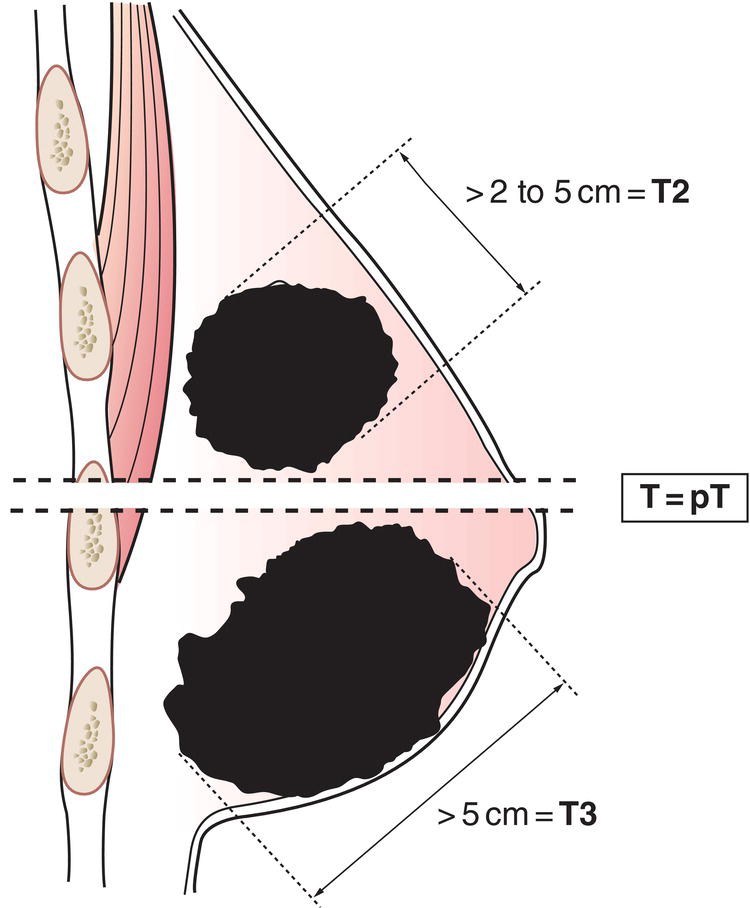
T2
Tumour more than 2 cm but not more than 5 cm in greatest dimension (Fig. 383)
T3
Tumour more than 5 cm in greatest dimension (Fig. 383)
T4
Tumour of any size with direct extension to chest wall and/or to skin (ulceration or skin nodules).
Invasion of the dermis alone does not qualify as T4. Chest wall includes ribs, intercostal muscles, and serratus anterior muscle but not pectoral muscle.
T4a
Extension to chest wall, not including only pectoralis muscle adherence/invasion (Fig. 384)
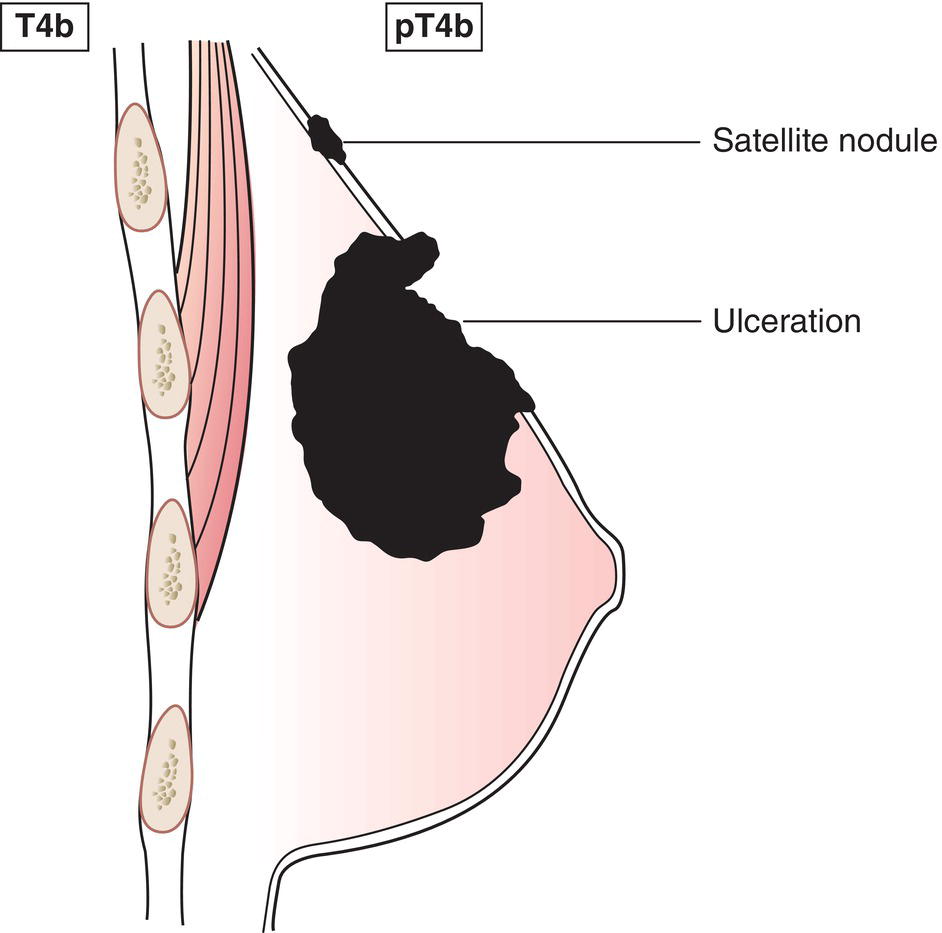
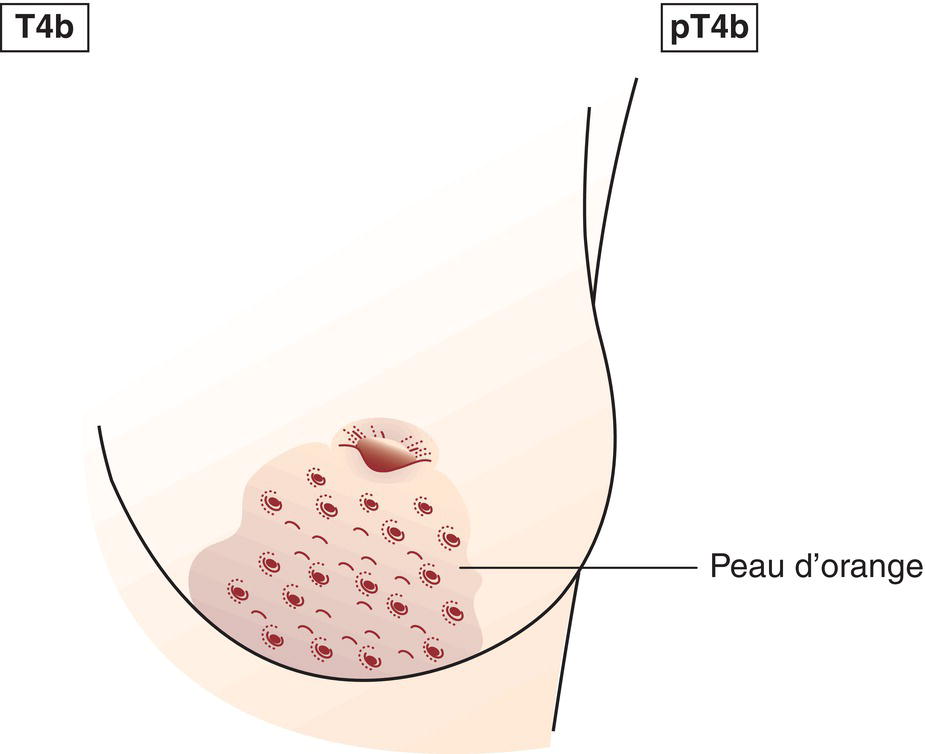
T4b
Ulceration and/or ipsilateral satellite skin nodules and/or oedema (including peau d’orange) of the skin which do not meet the criteria for inflammatory carcinoma (Figs. 385, 386)
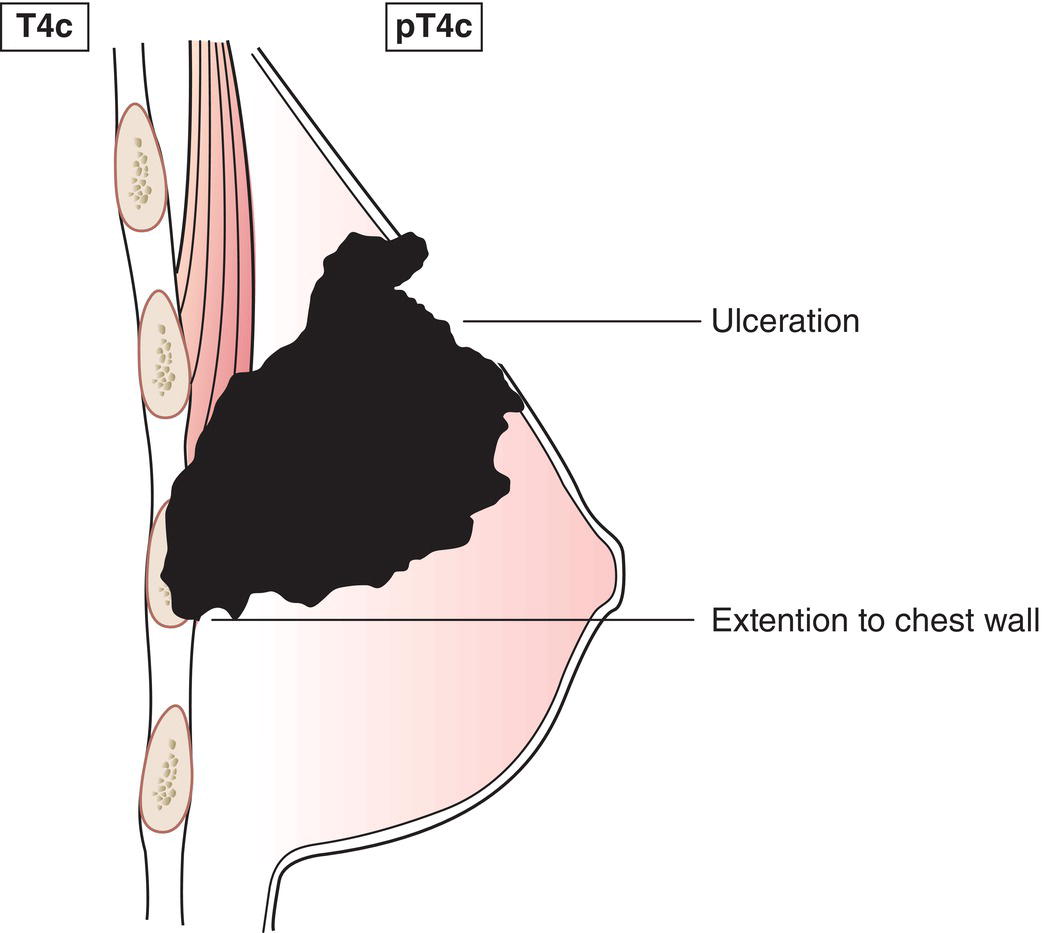
T4c
Both 4a and 4b, above (Fig. 387)
T4d
Inflammatory carcinoma (Fig. 388) 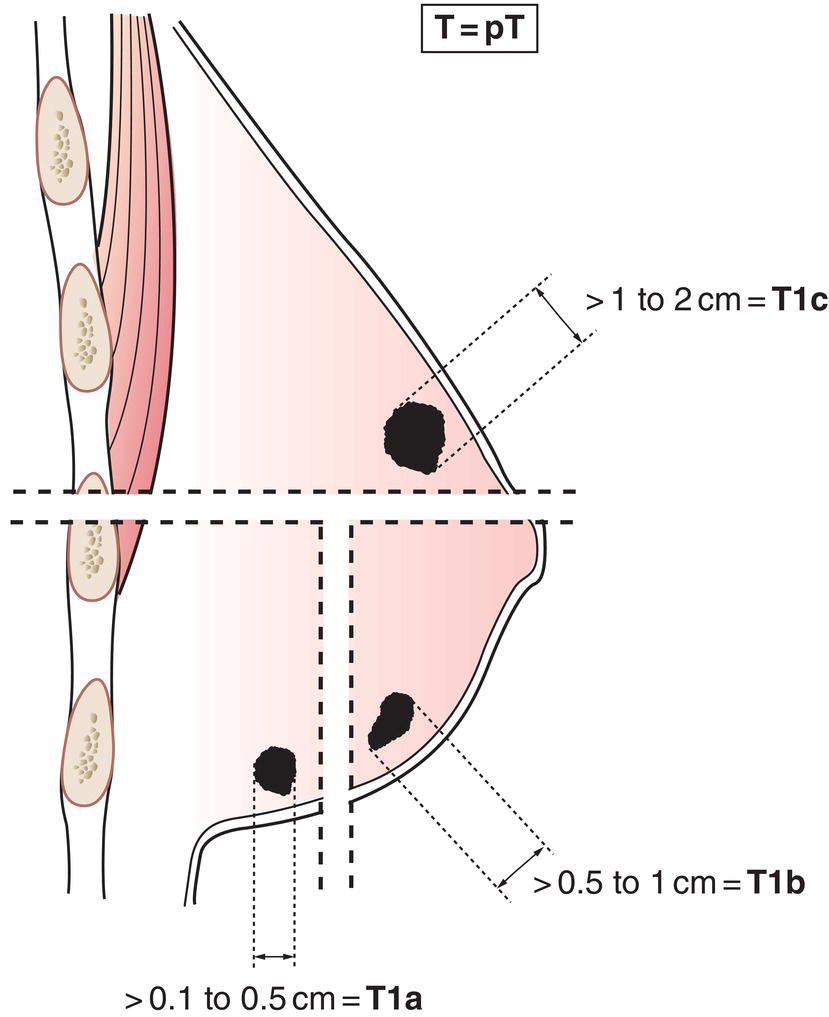

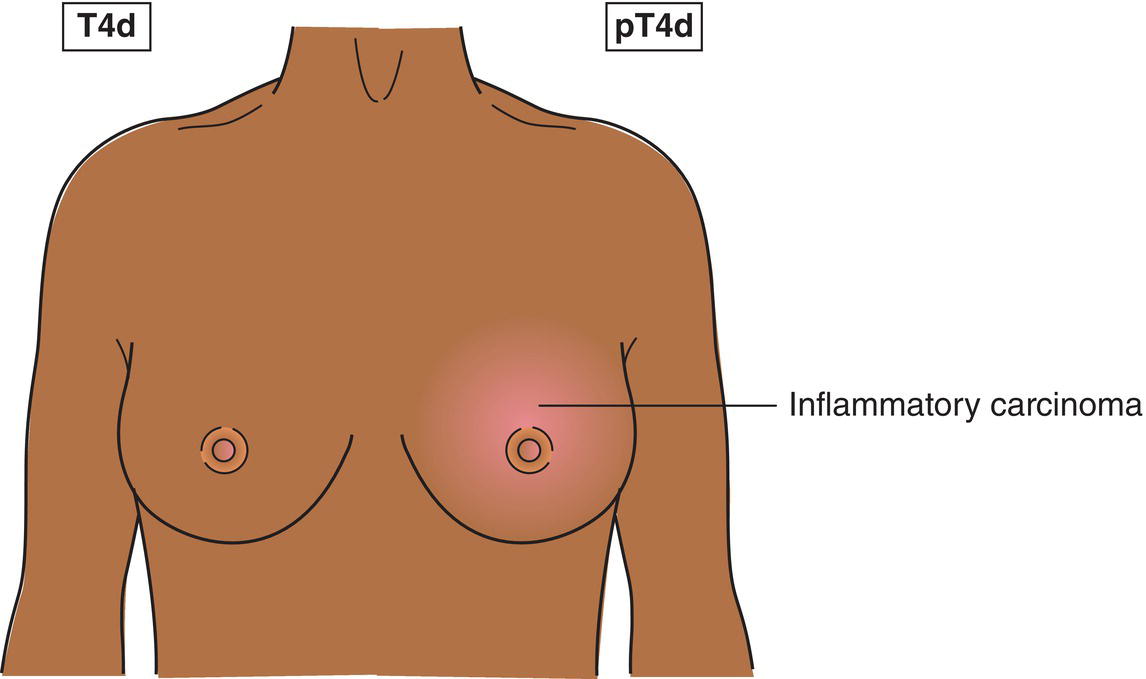
Inflammatory carcinoma of the breast is characterized by diffuse, brawny induration of the skin with an erysipeloid edge, usually with no underlying mass. If the skin biopsy is negative and there is no localized measurable primary cancer, the T category is pTX when pathologically staging a clinical inflammatory carcinoma (T4d). Dimpling of the skin, nipple retraction, or other skin changes, except those in T4b and T4d, may occur in T1, T2, or T3 without affecting the classification.
N – Regional Lymph Nodes
NX
Regional lymph nodes cannot be assessed (e.g., previously removed)
N0
No regional lymph node metastasis
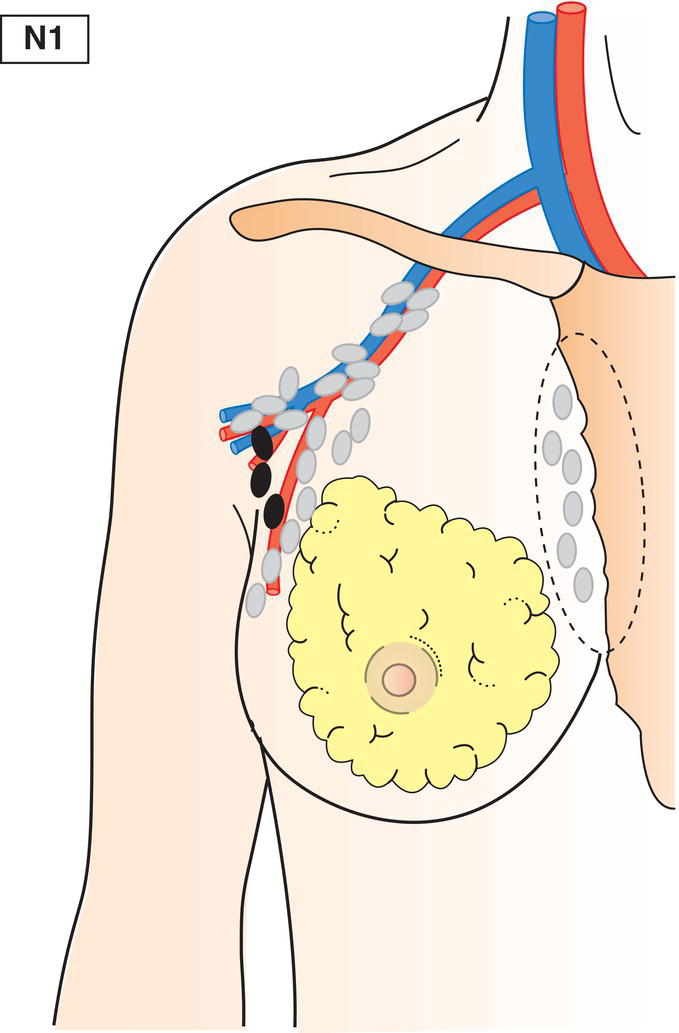
N1
Metastasis in movable ipsilateral level I, II axillary lymph node(s) (Fig. 389)
N2
Metastasis in ipsilateral level I, II axillary lymph node(s) that are clinically fixed or matted; or in clinically detected* ipsilateral internal mammary lymph node(s) in the absence of clinically evident axillary lymph node metastasis
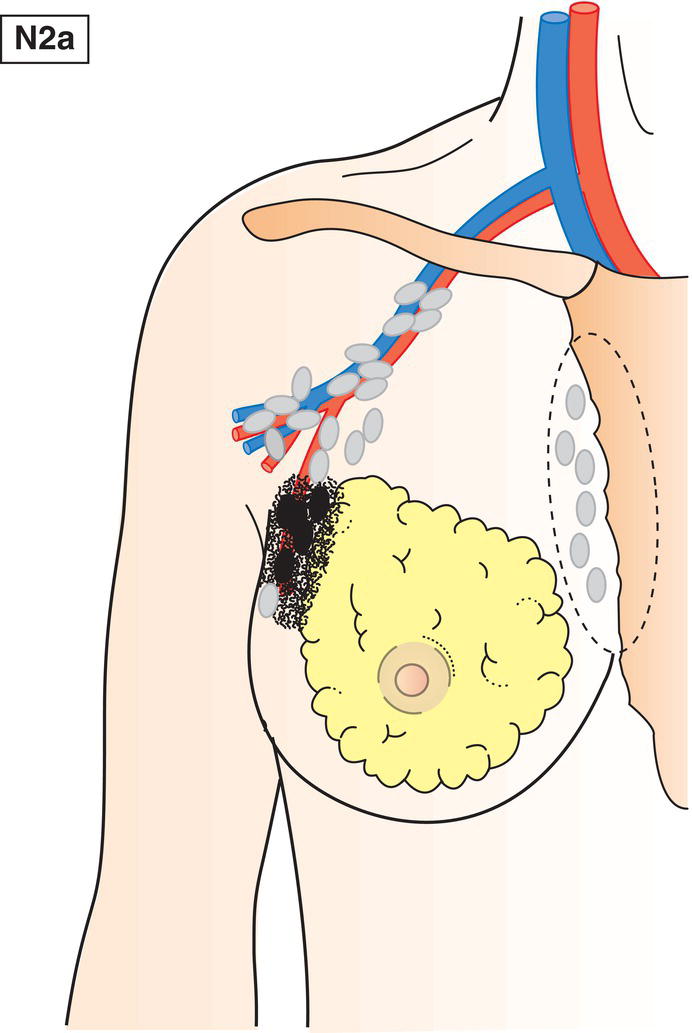
N2a
Metastasis in axillary lymph node(s) fixed to one another (matted) or to other structures (Fig. 390)
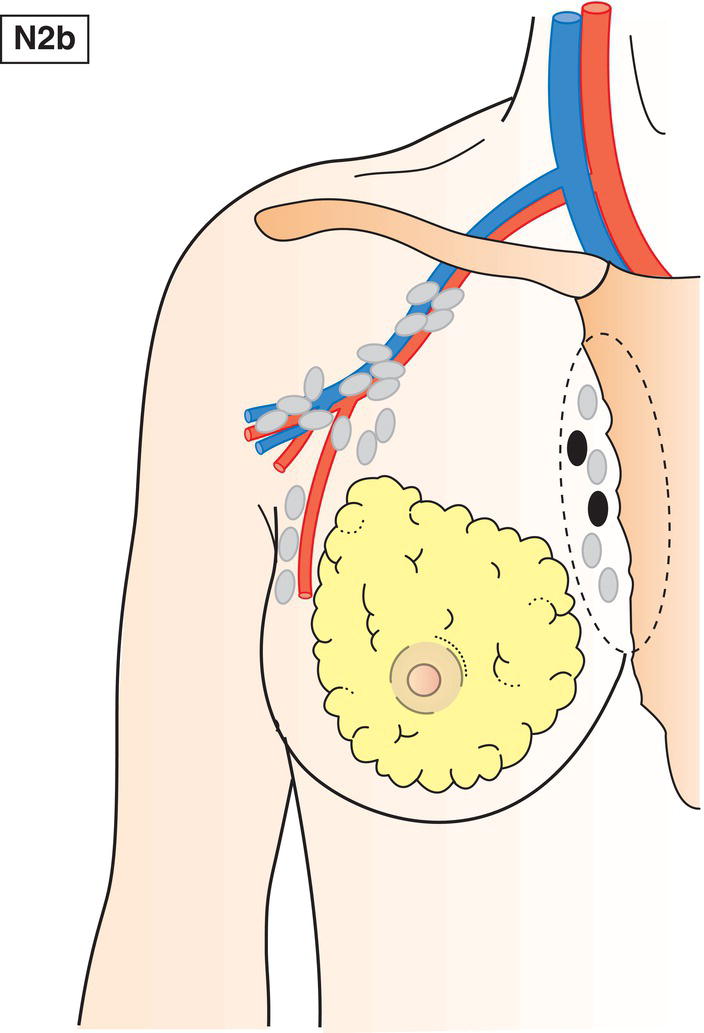
N2b
Metastasis only in clinically detected* internal mammary lymph node(s) and in the absence of clinically evident axillary lymph node metastasis (Fig. 391)
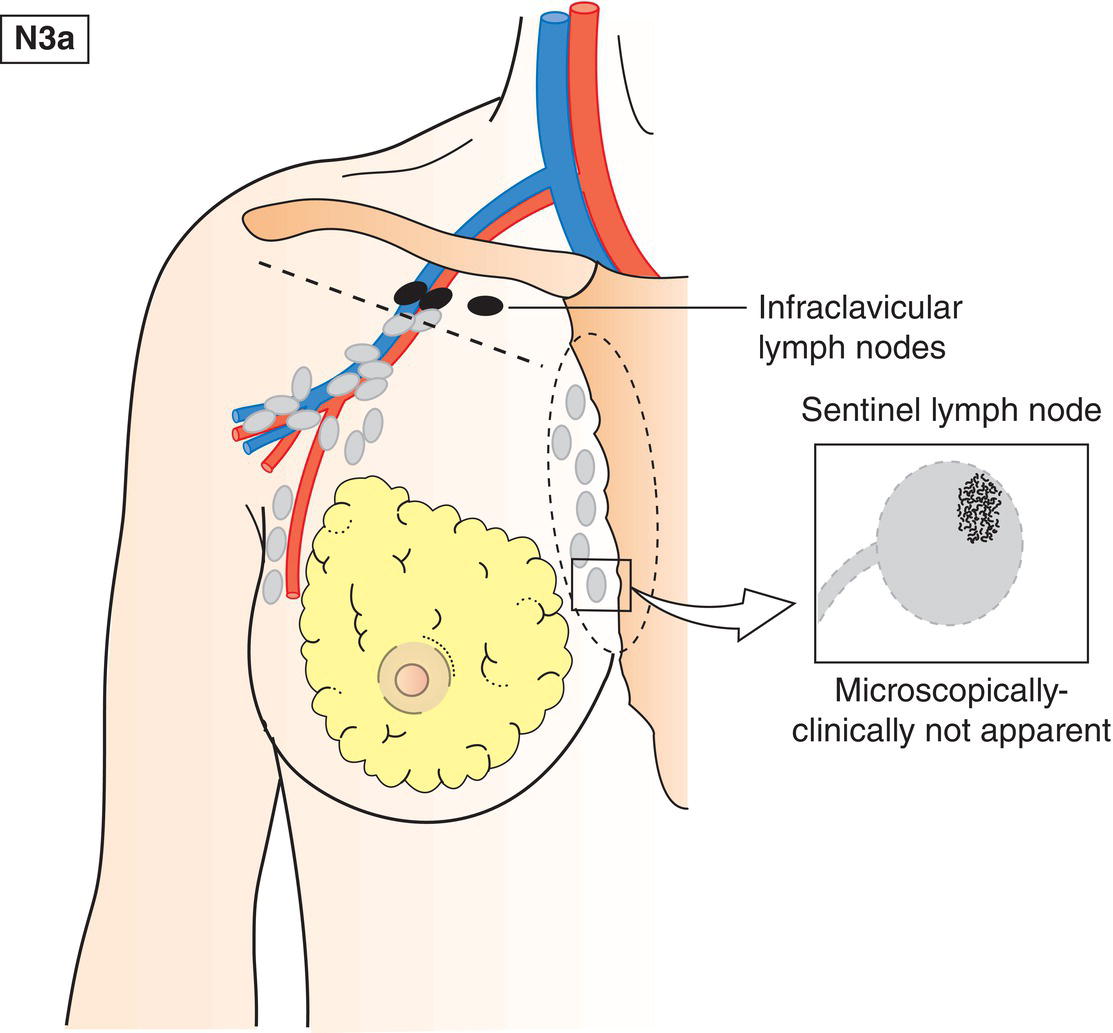
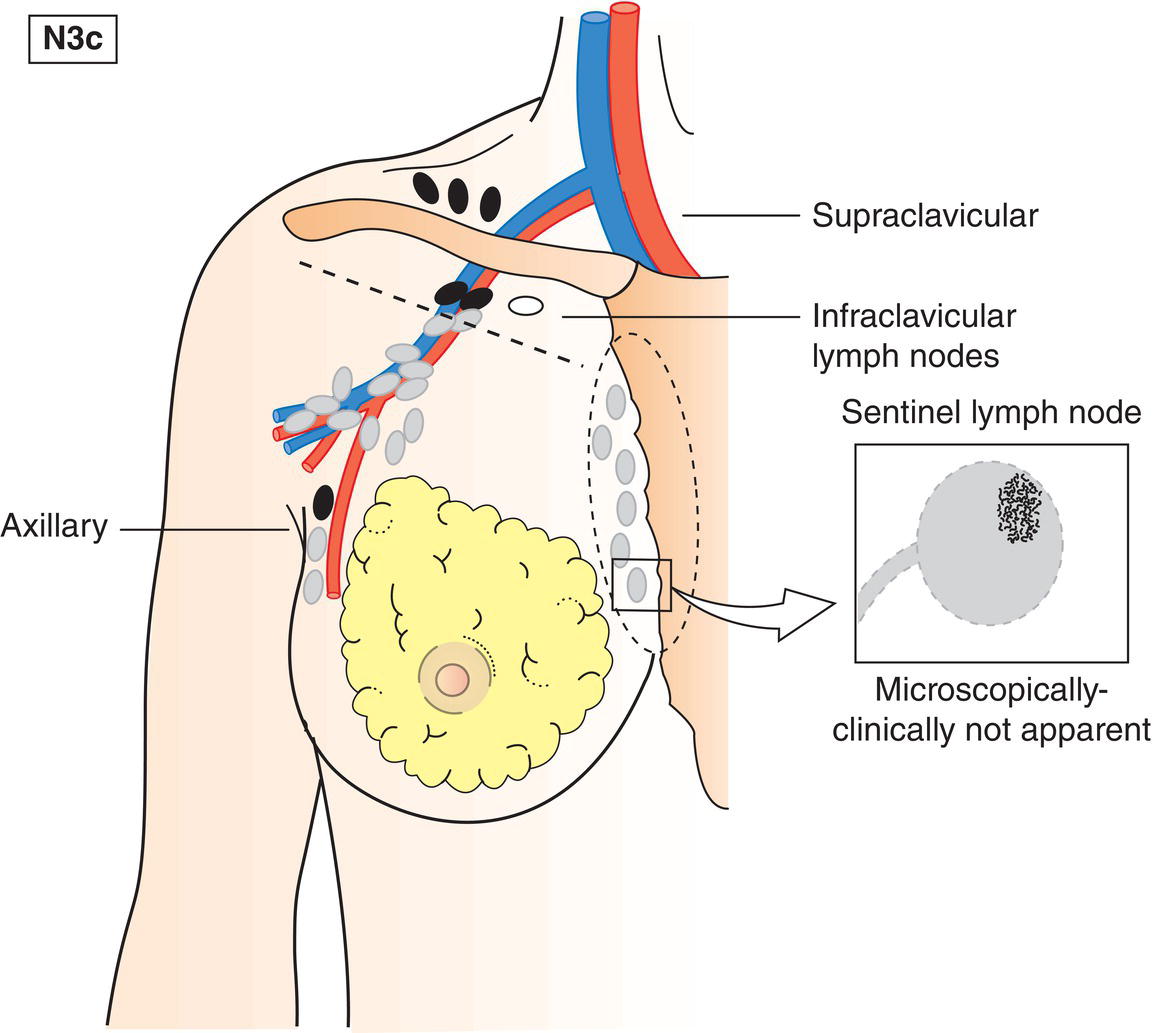
N3
Metastasis in ipsilateral infraclavicular (level III axillary) lymph node(s) with or without level I, II axillary lymph node involvement; or in clinically detected* ipsilateral internal mammary lymph node(s) with clinically evident level I, II axillary lymph node metastasis; or metastasis in ipsilateral supraclavicular lymph node(s) with or without axillary or internal mammary lymph node involvement
N3a
Metastasis in infraclavicular lymph node(s) (Fig. 392)
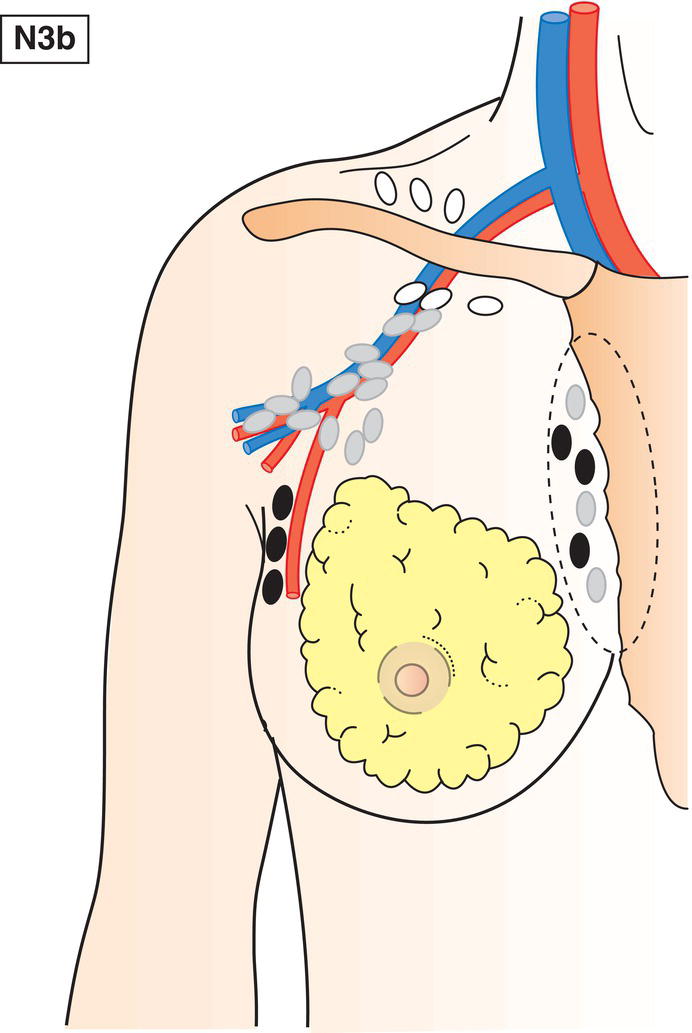
N3b
Metastasis in internal mammary and axillary lymph nodes (Fig. 393)
N3c
Metastasis in supraclavicular lymph node(s) (Fig. 394)
* Clinically detected is defined as detected by clinical examination or by imaging studies (excluding lymphoscintigraphy) and having characteristics highly suspicious for malignancy or a presumed pathological macrometastasis based on fine needle aspiration biopsy with cytologic examination. Confirmation of clinically detected metastatic disease by fine needle aspiration without excision biopsy is designated with an (f) suffix, e.g. cN3a(f).
M – Distant Metastasis
M0
No distant metastasis
M1
Distant metastasis
pTNM Pathological Classification
pT – Primary Tumour
When classifying pT the tumour size is a measurement of the invasive component. If there is a large in situ component (e.g., 4 cm) and a small invasive component (e.g., 0.5 cm), the tumour is coded pT1a.
pN – Regional Lymph Nodes
pNX
Regional lymph nodes cannot be assessed (e.g., previously removed, or not removed for pathologic study)
pN0
No regional lymph node metastasis*
* Isolated tumour cell clusters (ITC) are single tumour cells or small clusters of cells not more than 0.2 mm in greatest extent that can be detected by routine H and E stains or immunohistochemistry. An additional criterion has been proposed to include a cluster of fewer than 200 cells in a single histological cross section. Nodes containing only ITCs are excluded from the total positive node count for purposes of N classification and should be included in the total number of nodes evaluated (see Introduction).
pN1
Micrometastases; or metastases in 1 to 3 axillary ipsilateral lymph nodes; and/or in internal mammary nodes with metastases detected by sentinel lymph node biopsy but not clinically detected*
pN1mi
Micrometastases (larger than 0.2 mm and/or more than 200 cells, but none larger than 2.0 mm) (Fig. 395)
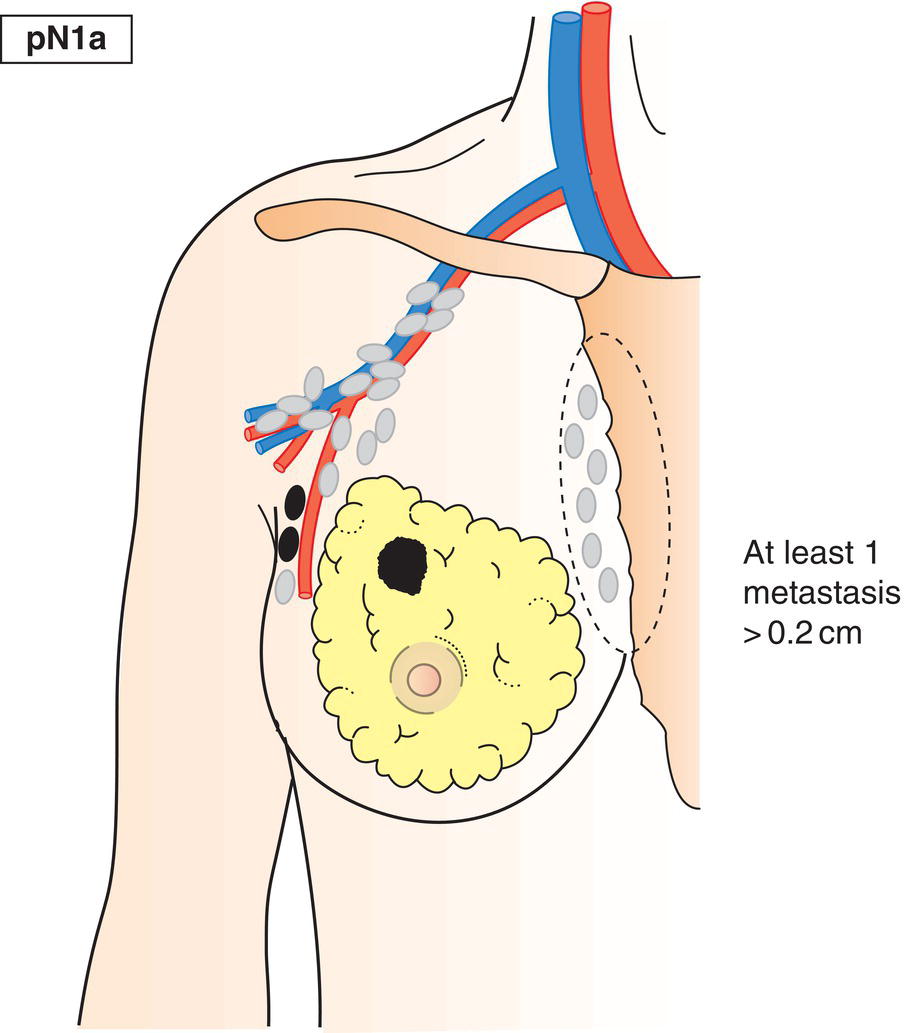
pN1a
Metastasis in 1–3 axillary lymph node(s), including at least one larger than 2 mm in greatest dimension (Fig. 396)
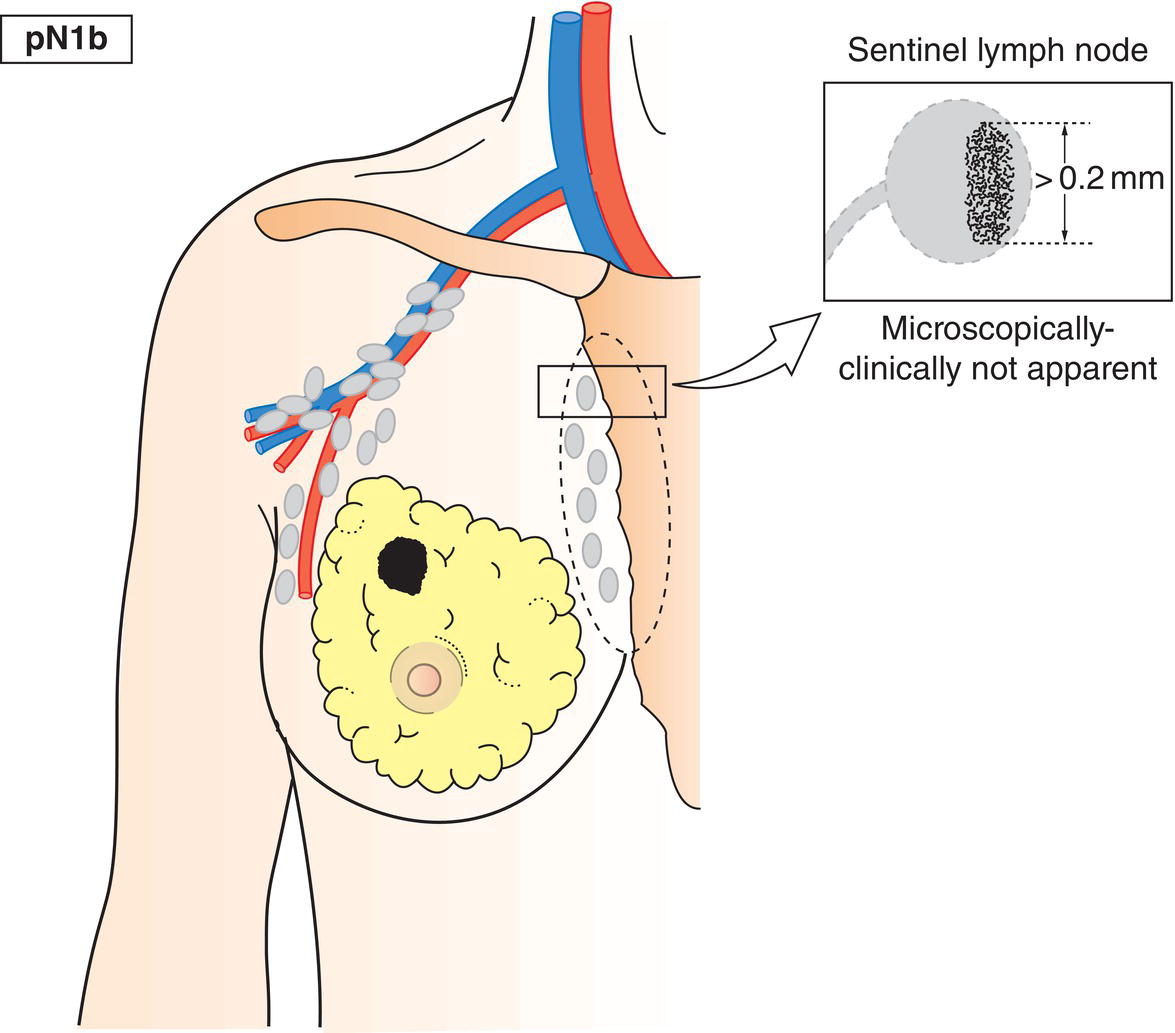
pN1b
Internal mammary lymph nodes not clinically detected (Fig. 397)
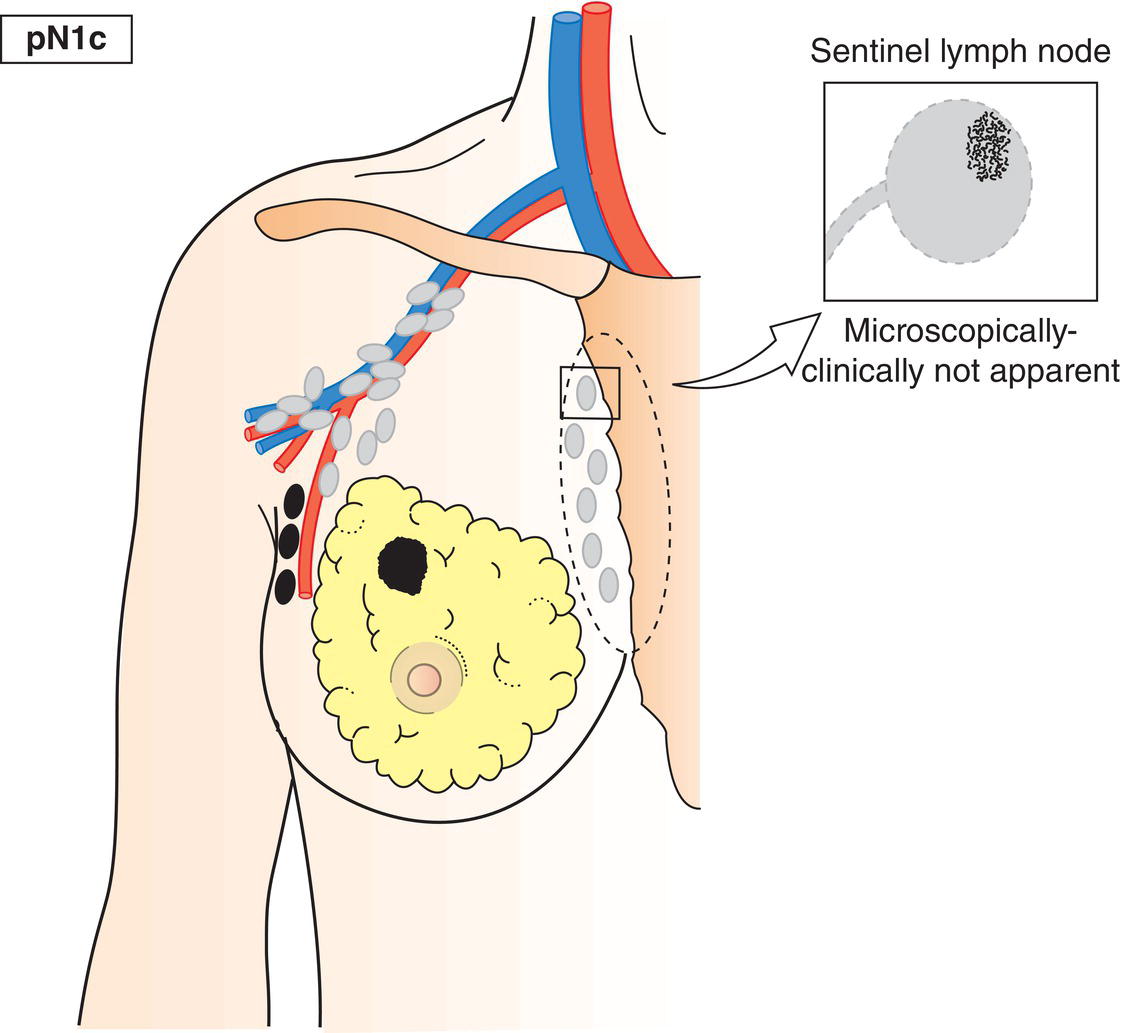
pN1c
Metastasis in 1–3 axillary lymph nodes and internal mammary lymph nodes not clinically detected (Fig. 398)
pN2
Metastasis in 4–9 ipsilateral axillary lymph nodes, or in clinically detected* ipsilateral internal mammary lymph node(s) in the absence of axillary lymph node metastasis
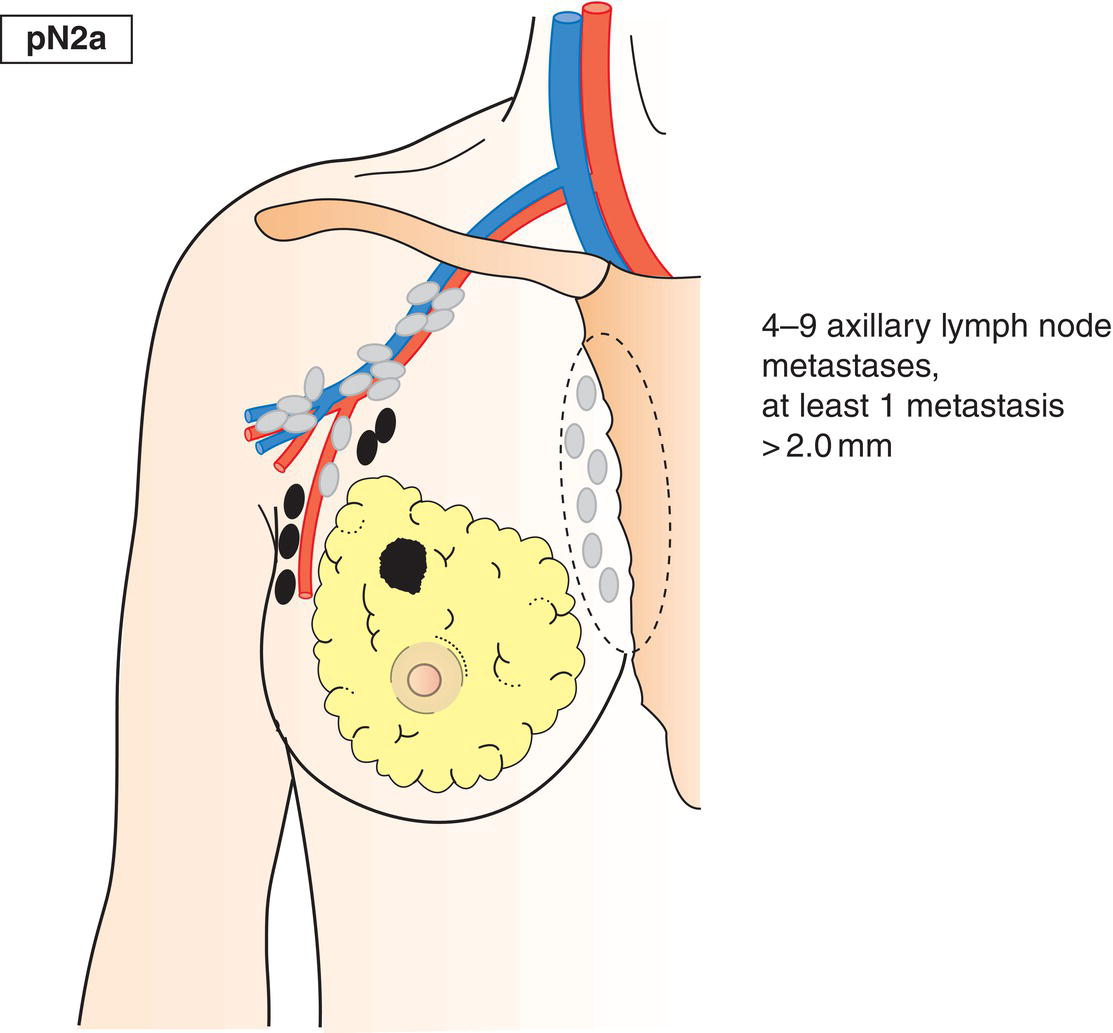
pN2a
Metastasis in 4–9 axillary lymph nodes, including at least one that is larger than 2 mm (Fig. 399)
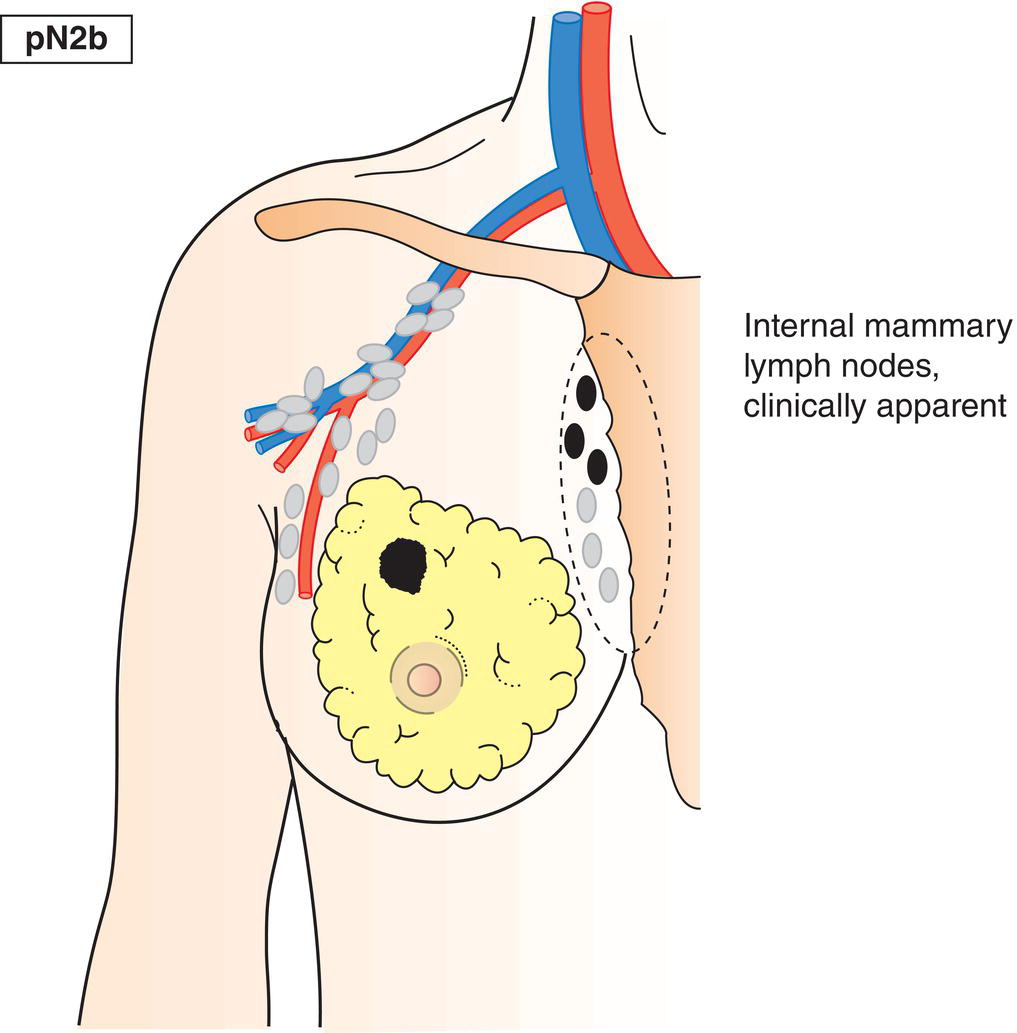
pN2b
Metastasis in clinically detected internal mammary lymph node(s), in the absence of axillary lymph node metastasis (Fig. 400)
pN3
Metastasis in 10 or more ipsilateral axillary lymph nodes; or in ipsilateral infraclavicular lymph nodes; or in clinically detected ipsilateral internal mammary lymph nodes in the presence of one or more positive axillary lymph nodes; or in more than 3 axillary lymph nodes with clinically negative, microscopic metastasis in internal mammary lymph nodes; or in ipsilateral supraclavicular lymph nodes
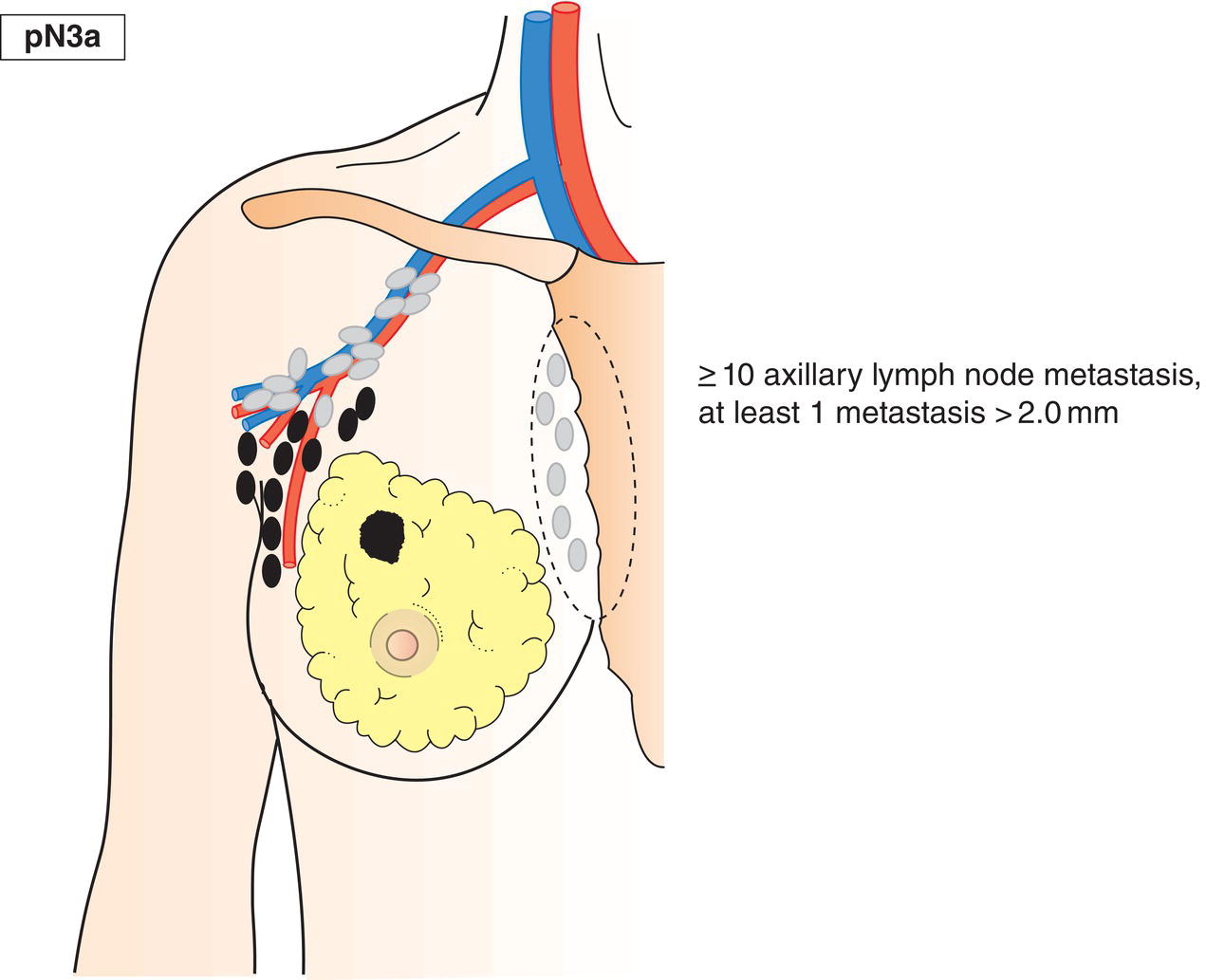
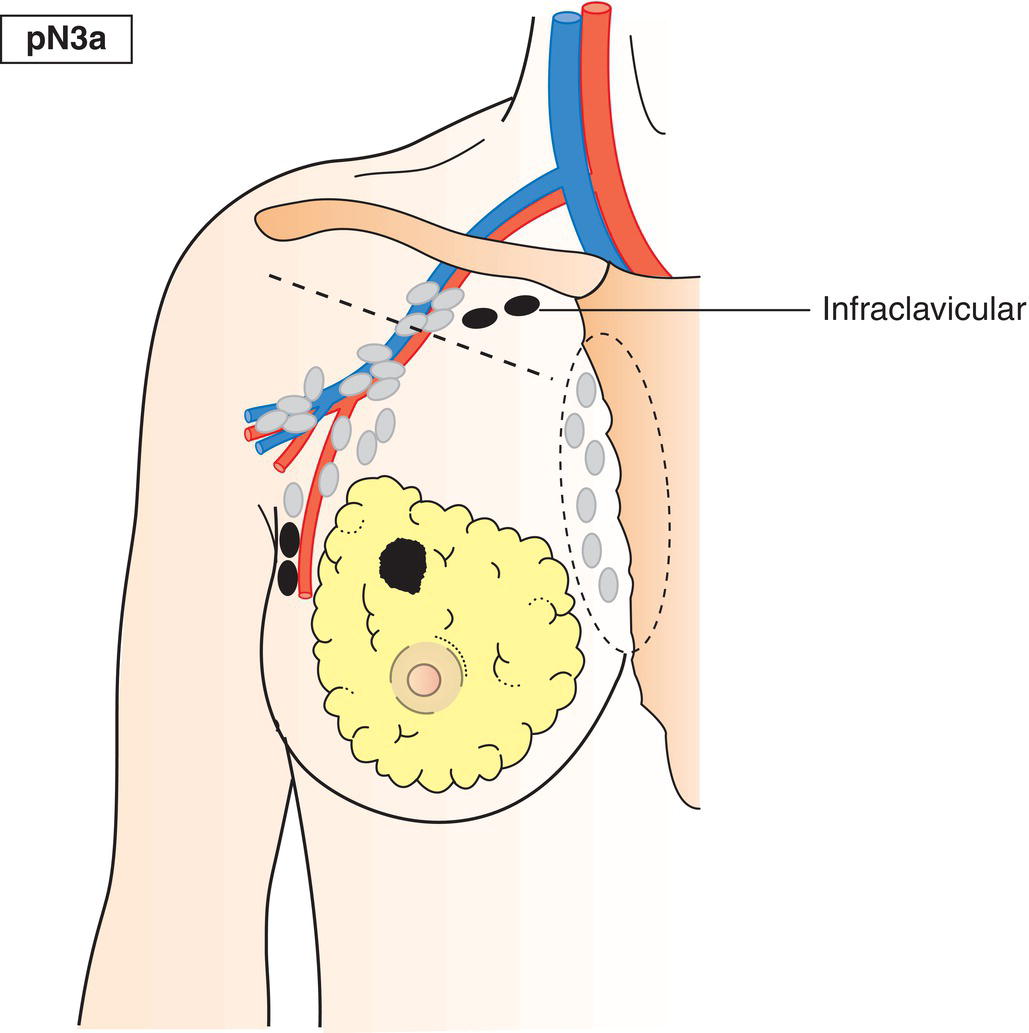
pN3a
Metastasis in 10 or more axillary lymph nodes (at least one larger than 2 mm) or metastasis in infraclavicular lymph nodes/Level III lymph nodes (Figs. 401, 402)
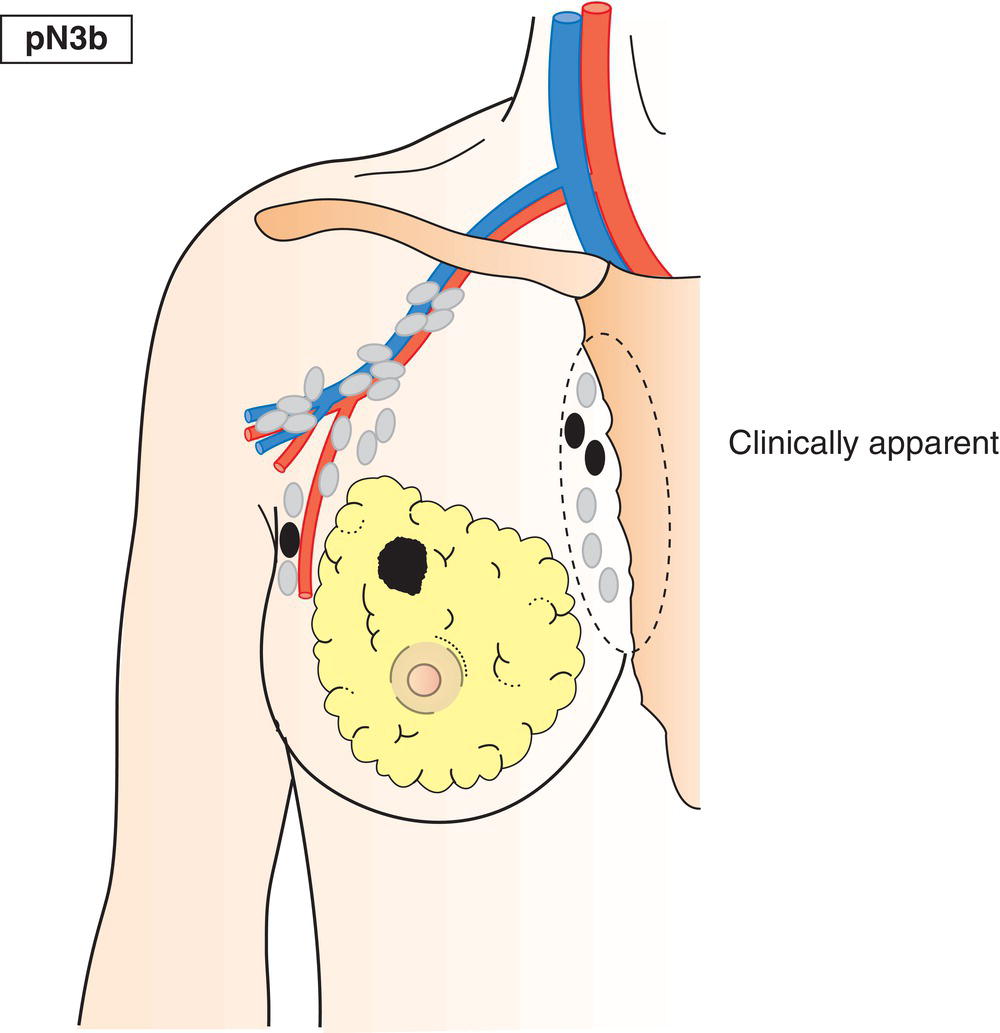
pN3b
Metastasis in clinically detected* internal mammary lymph node(s) in the presence of positive axillary lymph node(s) (Fig. 403); or metastasis in more than 3 axillary lymph nodes and in internal mammary lymph nodes with microscopic or macroscopic metastasis detected by sentinel lymph node dissection but not clinically detected
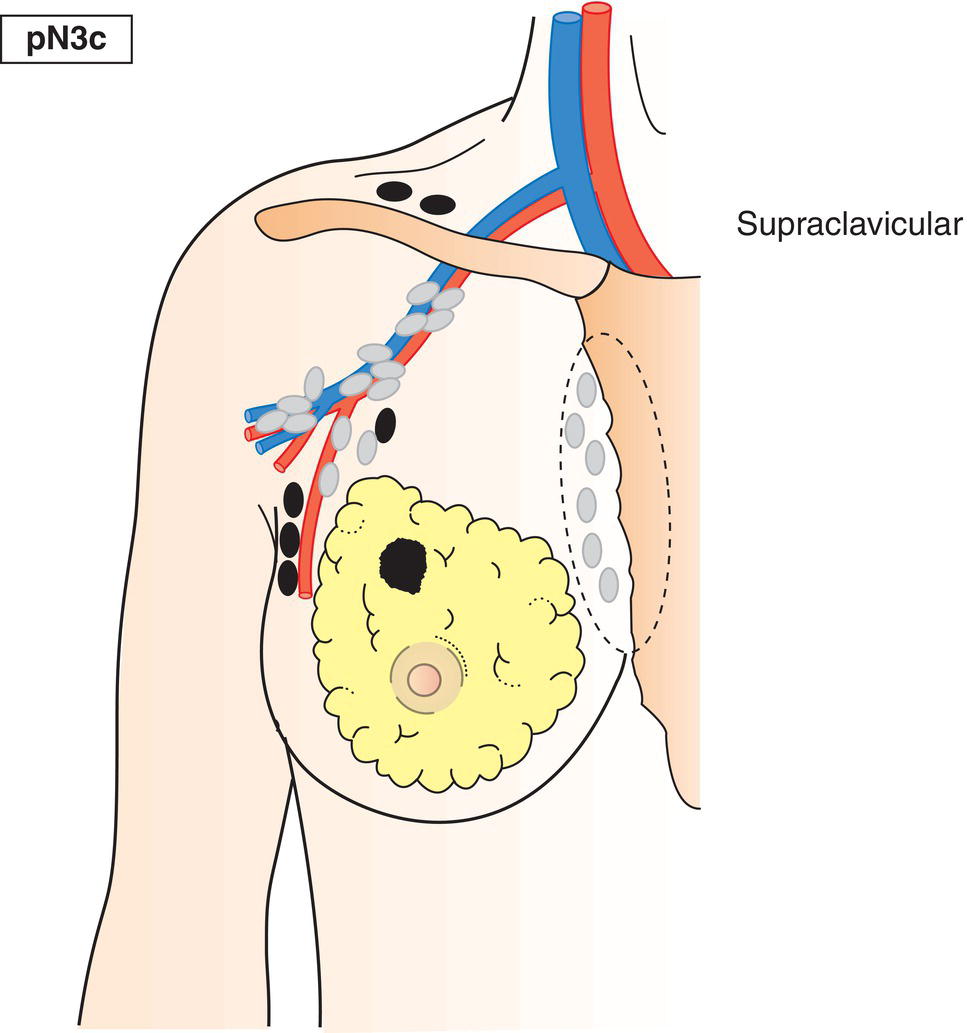
pN3c
Metastasis in supraclavicular lymph node(s) (Fig. 404) 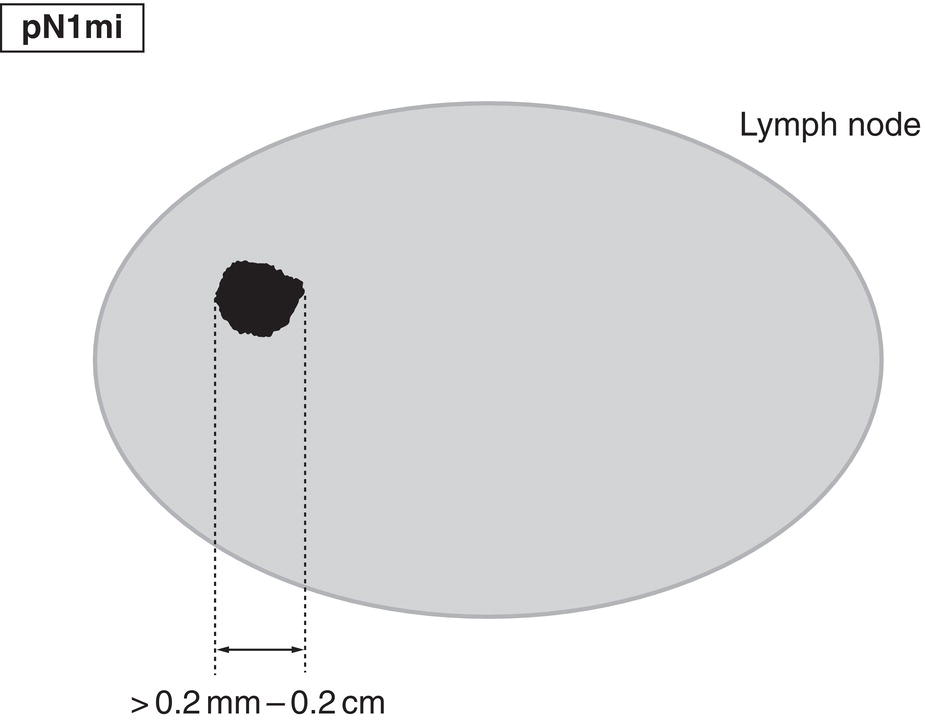
* Clinically detected is defined as detected by imaging studies (excluding lymphoscintigraphy) or by clinical examination and having characteristics highly suspicious for malignancy or a presumed pathologic macrometastasis based on fine needle aspiration biopsy with cytologic examination.
pM – Distant Metastasis
pM1
Distant metastasis microscopically confirmed
pM0 and pMX are not valid categories.
Summary
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree