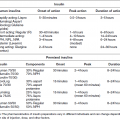
Case 5 Ira B. Lamster, DDS, MMSc; Nurit Bittner, DDS, MS; and Daniel Lorber, MD A 62-year-old male presented with the chief complaint, “I want a check-up. I had a great deal of dental work three years ago, and now everything is coming apart.” He began to notice his teeth were shifting and his crowns were becoming loose about six months ago. The patient did not have any regular dental follow-up in the past three years. Three months ago he had an acute dental emergency, and a number of teeth were extracted. The patient was diagnosed with type 2 diabetes mellitus six months ago. At that time his HbA1c was 9.8%. He was given a course of treatment consisting of lifestyle changes (exercise and diet control) and metformin. He was also diagnosed with high blood pressure, with an initial blood pressure of 160/100 mmHg. He is taking lisiniopril and hydrochlorthiazide for his blood pressure. He also takes atorvastatin (Lipitor® 10 mg daily) for elevated cholesterol, but is otherwise well. At this time his HbA1c is 7.6%, representing improved metabolic control. The dentist reviewed the patient’s history, and discussed the patient’s status with the treating physician. It was suggested that prior to the diagnosis of diabetes, the metabolic syndrome likely was present at the time of the prosthodontic rehabilitation three years ago. The patient has smoked eight cigarettes a day for the past 25 years (10 pack years). He denies recreational drug use. He drinks alcohol socially (one glass of wine/day). The mandibular anterior implant-supported fixed partial denture and the right maxillary first and second molar implant-supported crowns were completed six years ago. Ceramic crowns for the maxillary incisors were completed three years ago (Figures 1 and 2). Figure 1 Maximum intercuspation, anterior view (after initial prosthodontic rehabilitation). Figure 2 Maxillary occlusal view (after initial prosthodontic rehabilitation). The last dental visit was three months ago. The patient did not have a regular dentist and went to a hospital dental clinic for emergency care. The maxillary lateral incisors and maxillary left first molar were extracted due to infection and advanced alveolar bone loss. There were no significant findings on the extraoral examination. Muscles of mastication and facial expression were all within normal limits. The function of the temporomandibular joints was within normal limits. The intraoral examination of the soft tissues, including the tongue, floor of the mouth, hard and soft palate and buccal mucosa, did not reveal any abnormalities. The oral cancer screen was negative. The patient was partially edentulous, missing teeth #1, 2, 3, 5, 7, 10, 12, 14, 16, 17, 23, 24, 25, 26, and 32. Light plaque and calculus accumulations were present. The gingiva was fibrotic and demonstrated moderate inflammation. Two weeks after an initial scaling and root planning session, slight inflammation remained, generalized 3–4 mm probing depths, with some localized areas of 5 mm or greater, with bleeding on probing (Figures 3 and 4). Figure 3 Maximum intercuspation, anterior view (current presentation). Figure 4 Maxillary occlusal view (current presentation). The maxillary central incisors presented with grade-two mobility. The maxillary left second premolar and the mandibular first molars demonstrated class 2 furcation involvement. No carious lesions were observed. The canine relationship was Class I Angle’s classification. The occlusal scheme observed was anterior guidance in protrusion and canine guidance on lateral movements. There were no interferences observed on any of the excursive movements. The maxillary central incisors demonstrated fremitus. Full-mouth series of radiographs were taken. Radiographic evaluation revealed generalized horizontal bone loss. The implants placed in the mandibular lateral incisors and the maxillary right first and second molar sites demonstrated bone loss of more than 2 mm, with a trough-like appearance. Radiographs were obtained from three years ago, taken after the completion of care. Radiographs were taken after the recent extractions and demonstrated progression of bone loss in the three-year period (Figures 5 and 6). Figure 5 Full mouth series of radiographs (after initial prosthodontic rehabilitation). Figure 6 Full mouth series of radiographs (current presentation). After evaluation of the medical and dental history and clinical and radiographic findings, the following problems list was identified: The initial dental treatment plan consisted of full mouth scaling and root planing. Based on the gingival response, pocket reduction periodontal surgery may be necessary in the mandibular posterior sextants. Extractions were suggested due to the poor periodontal prognosis of the maxillary central incisors. At this time, a maxillary removable partial denture was the best prosthodontic option. This denture will ensure that the remaining teeth are maintained as long as possible until acceptable metabolic control, and control of blood pressure, are demonstrated over a longer period of time. If good metabolic control is not maintained, this will be the final restoration. A removable denture will facilitate the transition to a complete denture if other teeth in the maxillary arch display continued bone loss and require extraction. An alternate treatment plan was proposed if the patient demonstrates good metabolic control over an extended period of time (six months). This would involve implant placement in the maxillary lateral incisors and maxillary left first molar sites. The final prosthesis will be a porcelain fused to metal implant-supported fixed partial denture for the maxillary incisors with the central incisors as pontics and a single implant crown on the maxillary left first molar. Upon completion of the prosthodontic treatment the patient will be closely followed for periodontal maintenance, including scaling and root planning every three months. After initial scaling and root planing, the maxillary central incisors were extracted, and a maxillary immediate interim removable partial denture was inserted. After re-evaluation of the periodontal condition following scaling and root planning, it was decided that periodontal surgery for pocket reduction was necessary in the mandibular posterior areas. Periodontal surgery would ideally be performed if the patient demonstrates adequate metabolic control. At this time metabolic control is improved (HbA1c = 7.9%). Periodontal surgery was performed as open debridement for root access. Pocket elimination surgery was not attempted, because it was felt that there was a risk of poor wound healing. It is also conceivable that the existing periodontal disease was contributing to the less than ideal metabolic control. The areas demonstrating peri-implantitis were treated with open surgical debridement and debridement of the implant surface with adjunctive use of antibiotics. During the three-month healing time after the last periodontal surgery, the patient was seen by his physician to monitor the metabolic status. His last medical evaluation revealed that the patient continued smoking six cigarettes a day, his blood pressure was 135/90 mmHg, and his HbA1c was 8.1% on metformin alone. Following recommendation from his physician, due to the poor metabolic control heightened by the patient’s high blood pressure, implant surgery was postponed. After discussion with the patient, his physician recommended addition of a GLP-1 agonist to his metabolic management. The GLP-1 agonists are injectable medications given twice daily (Byetta®), once daily (Victoza®), or once weekly (Bydureon®). GLP-1 agonists enhance insulin secretion, suppress glucagon, slow gastric emptying, and enhance satiety. The patient lost 8 lbs and his HbA1c decreased to 6.9%. The interim maxillary partial denture that was delivered was fabricated with a metal base and rest seats on #4, 6, 11, 13, and 15. As evidenced by a detailed history, it was suggested that this patient had “metabolic syndrome” at the time of initial presentation three years ago. The metabolic syndrome is a complex of insulin resistance, abdominal obesity, hypertension, dyslipidemia (high triglycerides and low HDL cholesterol), and elevated fasting glucose (greater than 100 mg/dL). The metabolic syndrome is associated with a significantly increased risk of atherosclerotic cardiovascular disease and type 2 diabetes mellitus (Table 1 [1]). Data from the NHANES 2003–2006 revealed that more than one-third of American adults have the metabolic syndrome [2]. A systematic review found a significant association between periodontal disease and the presence of the metabolic syndrome [3]. Table 1 Criteria for the diagnosis of metabolic syndrome (National Cholesterol Education Program Adult Treatment Panel III). Grundy SM, Brewer HB Jr., Cleeman JI, Smith SC Jr., Lenfant C; American Heart Association: National Heart, Lung, and Blood Institute. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation, 2004 Jan 27; 109(3):433–8. The Diabetes Prevention Program (DPP) investigated the effects of lifestyle change or metformin on incidence of type 2 diabetes in a high risk cohort. Approximately 53% of the participants in the Diabetes Prevention Program had metabolic syndrome. Lifestyle change in the DPP consisted of intensive coaching, with the aim of achieving and maintaining at least 7% weight reduction by diet and at least 150 minutes a week of moderate exercise [4]. Lifestyle change resulted in a 58% reduction in development of type 2 diabetes over a 2.8-year follow-up. Metformin was somewhat less effective, resulting in a 31% reduction in diabetes incidence. Lifestyle change reduced the prevalence of metabolic syndrome by one-third. Metformin, although decreasing the incidence of new diabetes mellitus, had no impact on the prevalence of metabolic syndrome. This case illustrates the importance of complete patient evaluation prior to beginning dental care. It also illustrates the importance of close follow-up after prosthodontic care. In this case the re-established masticatory function was adversely affected by the medical status of the patient, specifically the onset of the diabetes mellitus, and the loss of support about teeth and implants. Diabetes mellitus adversely affects the severity of periodontitis, and poor periodontal health may also adversely influence metabolic control [5]. Furthermore, the effect of poor metabolic control on dental implant outcomes is controversial [6], as there is evidence of delayed healing of implants when the HbA1c level is above 8% [7]. In addition, medical complications of diabetes mellitus occur more commonly when metabolic control is poor. If the HbA1c level is above 8–8.5% the diabetes is considered poorly controlled and a more conservative restorative approach may be advisable. In patients with poorly controlled diabetes, the dental restorative treatment should focus on maintaining the remaining teeth for as long as possible because treatment with implants is invasive, time consuming, and expensive. Fixed partial dentures to replace the missing teeth is the treatment of choice for small edentulous areas. For large edentulous areas, removable partial dentures are indicated. In this case, the decision was made to retain the implants that had previously been placed and restored, but to treat the peri-implantitis. A conservative approach was chosen. A systematic review [8] has shown this approach to be an effective means of reducing clinical signs of inflammation and halting the progression of bone loss about the implants. However, when a removable complete or partial denture is necessary for poorly controlled diabetic patients, a closer follow-up schedule should be reinforced, which may include assessment of salivary flow, and if required, treatment of xerostomia with rinses and special chewing gums [9]. Also, to improve retention of the dentures, periodic relining of the prosthesis may be necessary; the patient should be made aware of the importance of a frequent recall schedule to monitor all possible complications. These patients should also be periodically evaluated for carious lesions because an elevated prevalence of root caries in type 2 diabetic patients has been reported [10]. To prevent caries, a topical fluoride supplement protocol (fluoride rinse and fluoride varnish) should be considered [11].
A patient diagnosed with diabetes mellitus after comprehensive prosthodontic rehabilitation
Medical history
Dental history and history of the current problem
Treatment plan
Treatment
Discussion
Any three of the following:
Waist circumference > 102 cm (men); 88 cm (women)
Triglycerides ≥ 150 mg/dL
HDL cholesterol < 40 mg/dl (men); < 50 mg/dL (women)
BP ≥ 130/85
Fasting glucose ≥ 100 mg/dL
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree