##
Establishing corticotropin (ACTH) dependence is a crucial step in the diagnostic evaluation of hypercortisolism and relies on measurement of ACTH. In ACTH-dependent hypercortisolism, pituitary magnetic resonance imaging (MRI) is the first localization test, whereas in ACTH-independent hypercortisolism, computed cross-sectional adrenal imaging is recommended. Discordant findings in the diagnostic evaluation should raise suspicion for a laboratory error.
Case Report
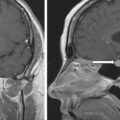
A 26-year-old woman was referred for the evaluation of Cushing syndrome (CS). For 2 years before the diagnosis of CS, she noticed development of striae, weight gain of 25 pounds, headaches, and hypertension. She was referred to a local endocrinologist who suspected and confirmed hypercortisolism with elevated levels of 24-hour urinary free cortisol and midnight salivary cortisol. ACTH-dependent hypercortisolism was diagnosed after the plasma ACTH was found to be elevated. MRI of pituitary gland was performed and was negative for pituitary lesions. The patient was referred to a tertiary center for further evaluation. On physical examination, she was noted to have facial rounding, facial erythema, supraclavicular pads, and dorsocervical pad. Oral examination demonstrated thrush. She had several abdominal striae. Her body mass index was 26.6 kg/m 2 , and blood pressure was 142/95 mmHg. Her only medical therapy at the time of evaluation was spironolactone, 100 mg daily.
INVESTIGATIONS
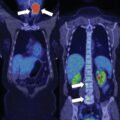
Hypercortisolism was confirmed at our institution ( Table 17.1 ). However, baseline testing revealed discrepant workup for ACTH dependence: whereas ACTH was elevated at 119 pg/mL (normal, 10–60), dehydroepiandrosterone sulfate (DHEA-S) was low-normal at 53 mcg/dL (normal, 44–332), suggestive of ACTH-independent hypercortisolism. This discrepancy prompted further communication with our laboratory medicine team, and it was decided to reanalyze ACTH with an alternate assay, suspecting an interference affecting the Siemens Immulite ACTH assay. When reanalyzed with the Roche Elecsys assay, ACTH was undetectable ( Table 17.1 ). After confirmation of ACTH-independent hypercortisolism, adrenal imaging was obtained. MRI of abdomen revealed a 4.2-cm well-circumscribed, homogeneously enhancing mass arising from the left adrenal gland ( Fig. 17.1 ). Adrenalectomy was recommended.
| Biochemical Test | Result | Reference Range |
| Midnight salivary cortisol, ng/dL | 620 | <100 |
| Midnight salivary cortisol, ng/dL | 927 | <100 |
| Morning serum cortisol, mcg/dL | 26 | 7–25 |
| ACTH, pg/mL (Siemens Immulite assay) | 119 | 10–60 |
| ACTH, pg/mL, reanalyzed by a different assay (Roche Elecsys assay) | <5 | 7.2–63 |
| DHEA-S, mcg/dL | 53 | 44–332 |
| Aldosterone, ng/dL (on spironolactone) | 22 | <21 |
| Plasma renin activity, ng/mL per hour (on spironolactone) | 8.4 | 2.9–10.8 |
| Plasma metanephrine, nmol/L | 0.22 | <0.5 |
| Plasma normetanephrine, nmol/L | 0.25 | <0.9 |
| Urine free cortisol, mcg/24 h | 120 | 3.5–45 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree