Paraproteinaemia
This is the presence of a monoclonal immunoglobulin band in the serum. Normally, serum immunoglobulins are polyclonal and represent the combined output from millions of different plasma cells. A monoclonal band (M-protein), or paraprotein, reflects the synthesis of immunoglobulin from a single clone of plasma cells. This may occur as a primary neoplastic disease or secondary to an underlying benign or neoplastic disease affecting the immune system (Table 21.1).
Table 21.1 Diseases associate ed with monoclonal immunoglobulins.
| Neoplastic |
| Multiple myeloma |
| Solitary plasmacytoma |
| Monoclonal gammopathy of undetermined significance (MGUS) |
| Waldenström macroglobulinaemia |
| Non-Hodgkin lymphoma |
| Chronic lymphocytic leukaemia |
| Primary amyloidosis |
| Heavy-chain disease |
| Benign |
| Chronic cold haemagglutinin disease |
| Transient (e.g. with infections) |
| HIV infection |
| Gaucher’s disease |
Multiple myeloma (myelomatosis) is a neoplastic disease characterized by plasma cell accumulation in the bone marrow, the presence of monoclonal protein in the serum and/or urine and, in symptomatic patients, related tissue damage. Ninety-eight per cent of cases occur over the age of 40 years with a peak incidence in the seventh decade. The term asymptomatic (smouldering) multiple myeloma is used for cases with similar laboratory findings but no organ or tissue damage. Retrospective analysis of serum samples has shown that almost all cases of myeloma develop from a pre-existing monoclonal gammopathy of undetermined significance (MGUS; see below). Other plasma cell neoplasms are listed in Table 21.2.
Table 21.2 Plasma cell neoplasms (WHO, 2008).
| Monoclonal gammopathy of undetermined significance (MGUS) |
| Plasma cell myeloma |
| Variants: |
| Asymptomatic (smouldering) myeloma |
| Non-secretory myeloma |
| Plasma cell leukaemia |
| Plasmacytoma |
| Solitary plasmacytoma of bone |
| Extraosseous (extramedullary) plasmacytoma |
| Immunoglobulin deposition diseases |
| Primary amyloidosis |
| Systemic light and heavy chain deposition diseases |
| Osteosclerotic myeloma (POEMS syndrome) |
The myeloma cell is a post-germinal centre plasma cell that has undergone immunoglobulin class switching and somatic hypermutation and secretes the paraprotein that is present in serum. Immunoglobulin heavy and light chain genes are clonally rearranged. Plasma cells naturally home to the bone marrow and this characteristic is retained by the tumour cell. The aetiology of the disease is unknown but it is more common in certain racial groups such as black individuals. Tumour cells accumulate complex genetic changes but dysregulated or increased expression of cyclin D (see p. 278) is believed to be an early unifying event.
Diagnosis
Symptomatic myeloma is diagnosed if there is:
1 Monoclonal protein in serum and/or urine (Fig. 21.1)
2 Increased clonal plasma cells in the bone marrow (Fig. 21.2) and
3 Related organ or tissue impairment.
Figure 21.1 Serum protein electrophoresis in multiple myeloma showing an abnormal paraprotein in the γ-globulin region with reduced levels of background β-and γ-globulins.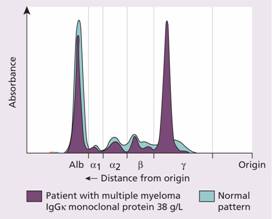
Figure 21.2 (a) The bone marrow in multiple myeloma showing large numbers of plasma cells, with many abnormal forms. (b) Low power view showing sheets of plasma cells replacing normal haemopoietic tissue. (c) Immunohistochemical staining of the bone marrow in myeloma with antibody to CD138 revealing extensive numbers of plasma cells.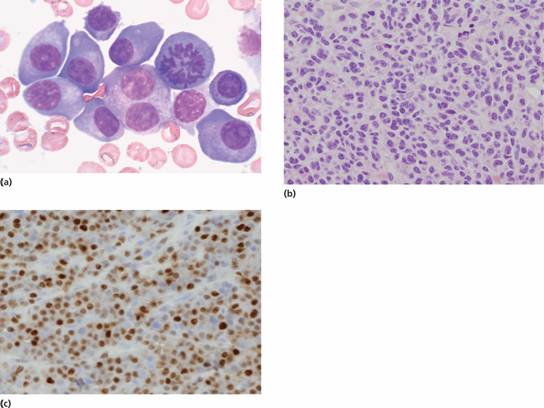
A useful acronym for tissue damage is CRAB (hypercalaemia, renal impairment, anaemia, bone disease). Also, amyloid, hyperviscosity and recurrent infection may also be present.
Asymptomatic (smouldering) myeloma is diagnosed if there is an M protein in serum at myeloma levels (>30g/L) and/or 10% or more of clonal plasma cells in the marrow but no related organ or tissue impairment (e.g. CRAB or myeloma-related symptoms).
Clinical features
1 Bone pain (especially backache) resulting from vertebral collapse and pathological fractures (Fig. 21.3a ,b).
2 Features of anaemia, e.g. lethargy, weakness, dyspnoea, pallor, tachycardia.
3 Recurrent infections: related to deficient antibody production, abnormal cell-mediated immunity and neutropenia.
4 Features of renal failure and/or hypercalcaemia: polydipsia, polyuria, anorexia, vomiting, constipation and mental disturbance.
5 Abnormal bleeding tendency: myeloma protein may interfere with platelet function and coagulation factors; thrombocytopenia occurs in advanced disease.
6 Amyloidosis occurs in 5% with features such as macroglossia, carpal tunnel syndrome and diarrhoea.
7 In approximately 2% of cases there is a hyperviscosity syndrome with purpura, haemorrhages, visual failure, central nervous system (CNS) symptoms, neuropathies and heart failure.
Figure 21.3 (a) Multiple myeloma: X-ray of lumbar spine showing severe demineralization with partial collapse of L3. (b) Magnetic resonance imaging (MRI) of spine: T2-weighted study. There is infiltration and destruction of L3 and L5 with bulging of the posterior part of the body of L3 into the spinal canal compressing the corda equina (arrowed). Radiotherapy has caused a marrow signal change in vertebrae C2–D4 because of replacement of normal red marrow by fat (bright white signal). (Courtesy of Dr A. Platts.)
Laboratory findings include the following:
1 Presence of a paraprotein Serum and urine should be screened by immunoglobulin electrophoresis. The paraprotein is immunoglobulin G (IgG) in 60% of cases, IgA in 20% and light chain only in almost all the rest. Less than 1% have IgD or IgE paraprotein and a similar number are non-secretory.
2 Elevated serum immunoglobulin-free light chains Immunoglobulin-free light chains (FLC) are κ or λ light chain proteins, synthesized by plasma cells that have not been paired with heavy chain (Fig. 21.4). They are normally made in small quantities and filtered from the serum into the kidney but can be measured in serum. Free light chains are produced by almost all malignant plasma cells and so the serum free light chain assay is useful in diagnosis and monitoring of myeloma and other forms of malignant paraproteinaemia. Typically in myeloma there is an increase in either the κ or λ serum free light chain value. The normal κ: λ serum free light chain ratio of 0.6 (range 0.26–1.65) is also skewed with an excess of either κ or λ chains. Light chain assays have largely replaced the need for analysis of urine paraproteinaemia.
3 Normal serum immunoglobulin levels (IgG, IgA and IgM) are reduced, a feature known as immune paresis. The urine contains free light chains, Bence-Jones protein, in two-thirds of cases. Rare cases of myeloma are non-secretory and therefore not associated with a paraprotein or Bence-Jones proteinuria although some will still show a disturbed free light chain ratio in the serum.
4 There is usually a normochromic, normocytic or macrocytic anaemia. Rouleaux formation is marked in most cases (Fig. 21.5). Neutropenia and thrombocytopenia occur in advanced disease. Abnormal plasma cells appear in the blood film in 15% of patients and can be detected by sensitive flow cytometry in over 50%.
5 High erythrocyte sedimentation rate (ESR).
6 Increased plasma cells in the bone marrow (usually > 20%) often with abnormal forms (Fig. 21.2). The characteristic immunophenotype of malignant plasma cells is CD38high CD138high and CD45low. Anti-CD138 is used to measure the number of plasma cells in the marrow biopsy (Fig. 21.2). Interleukin 6 is a potent growth factor for myeloma cells and is often active by an autocrine mechanism (secreted by, and acting on, the same cell).
7 Radiological investigation of the skeleton reveals bone lesions such as osteolytic areas without evidence of surrounding osteoblastic reaction or sclerosis in 60% of patients (Fig. 21.6) or generalized osteoporosis in 20% (Fig. 21.3). Twenty per cent have no bone lesions. In addition, pathological fractures or vertebral collapse (Fig. 21.3b) are common. The osteolytic lesions are caused by osteoclast activation resulting from high serum levels of RANKL (receptor activator of nuclear factor-κ B (NF-κ B) ligand), produced by plasma cells and bone marrow stroma, which binds to activatory RANK receptors on the osteoclast surface.
8 Serum calcium elevation occurs in 45% of patients. Typically, the serum alkaline phosphatase is normal (except following pathological fractures).
9 The serum creatinine is raised in 20% of cases. Proteinaceous deposits from heavy light chain proteinuria, hypercalcaemia, uric acid, amyloid and pyelonephritis may all contribute to renal failure (Fig. 21.7).
10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


