15 Locally Advanced Supraglottic Cancer: Larynx Preservation by Transoral Laser Microsurgery
Abstract
Transoral laser microsurgery (TLM) is now accepted in the treatment of early cancer of the supraglottis, as recent clinical practice guidelines confirm. However, there is ongoing debate as to whether TLM is appropriate for the management of locally advanced cancer of the supraglottis. We discuss diagnostic and management challenges in the clinical context of the case of a 78-year-old male patient with several comorbidities. The case presentation is followed by a review of the current literature. Our plan of management and the oncologic and functional outcomes following treatment are described.
15.1 Case Presentation
The following case presentation was approved by the ethics committee of the Medical Faculty of Kiel University (D 418/18) and consented by the patient. A 78-year-old retired male presented with a 3-month history of dysphagia and odynophagia with no associated dyspnea or stridor. He was a current smoker of 20 cigarettes per day for 50 years, and he had stopped drinking alcohol in the 1980s. His Eastern Cooperative Oncology Group performance status was 2, and he had several comorbidities. He suffered from chronic obstructive pulmonary disease (COPD), insulin-dependent type 2 diabetes mellitus, diabetic nephropathy with impaired renal function (glomerular filtration rate [GFR]: 60 mL/min), moderate sensorineural hearing loss, hypertension, coronary heart disease, and severe peripheral vascular disease resulting in an above-knee amputation 4 years ago. He was wheelchair dependent.
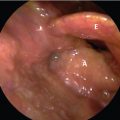
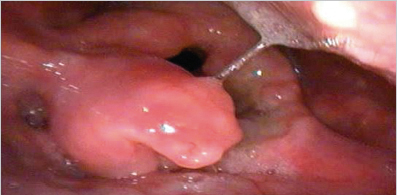
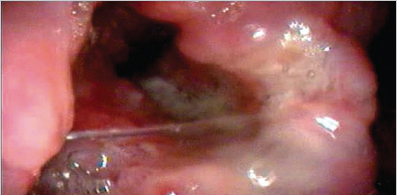
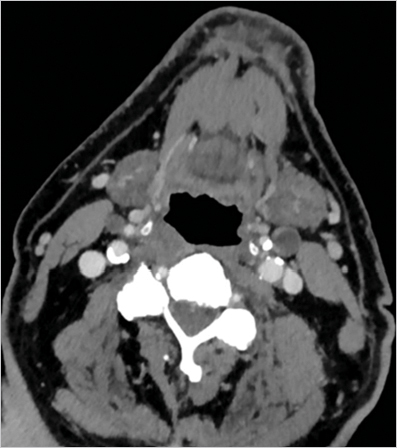
At flexible laryngoscopy, a tumor was detected involving the epiglottis, both ventricular folds, and the aryepiglottic fold on the left with extension to the mucosa above the arytenoid cartilage. Both vocal folds were mobile. ( Fig. 15‑1 , Fig. 15‑2). Microlaryngoscopy revealed the tumor extension described earlier and with superficial involvement of the postcricoid mucosa with no extension beyond the midline. The ventricle of Morgagni was uninvolved on both sides. Panendoscopy excluded a second primary cancer in the head and neck sites, lung, and esophagus. There were no palpable cervical lymph nodes. Biopsy revealed moderately differentiated squamous cell carcinoma (SCC). Ultrasound-guided fine-needle aspiration cytology from enlarged lymph nodes in level IIa bilateral was positive for SCC. CT scan of the larynx demonstrated a supraglottic tumor with infiltration of the pre-epiglottic space, the ventricular folds, and the left aryepiglottic fold. There were no signs of tumor extension to the paraglottic space at the glottic level, no signs of cartilage infiltration, or infiltration of the base of the tongue. One enlarged lymph node in level IIa (left 12-mm diameter, right 10-mm diameter), with central necrosis suspicious for metastatic disease was diagnosed bilaterally ( Fig. 15‑3 , Fig. 15‑4). CT scan of the lungs was unremarkable, as was the ultrasound examination of the abdominal organs.

The diagnosis was locally advanced SCC of the supraglottic larynx. The clinical stage according to the seventh edition of the Union for International Cancer Control (UICC) TNM (tumor size, node involvement, and metastasis status) classification system was cT3cN2cM0, UICC stage IVa.
15.2 Discussion
15.2.1 Treatment Options
Transoral laser microsurgery (TLM) is now accepted for the treatment of early cancer of the supraglottis, as a recent clinical practice guideline confirmss. Literatur and there is consensus that a single-modality treatment should be performed. In patients with locally advanced cancer of the supraglottics, several treatment options are available. The surgical treatment options are total laryngectomy or supraglottic laryngectomy (SGL), either by open-neck or by a transoral approach with the CO2 laser (TLM), for the treatment of the primary cancer. With limited metastases to the neck, the surgical treatment of the regional lymphatics consists in bilateral selective neck dissection of levels II to IV (SND II–IV). 2 Depending on the histopathologic findings regarding resection margins and the status of the neck nodes, adjuvant radiotherapy or chemoradiotherapy of the primary site and both sides of the neck might be indicated. The nonsurgical treatment options are radiotherapy alone, induction chemotherapy followed by radiotherapy, and concurrent chemoradiotherapy. Well-recognized issues to be considered when selecting a particular treatment option are accurate staging of the disease, the general health of the patient, and prospects for a good functional outcome.
The Surgical Options
Success of a surgical approach to larynx preservation depends on complete resection of the cancer (R0 resection), experience of the surgeon, and appropriate patient selection. The key issue to address when considering surgical options is the anatomic extent of the cancer. Standard SGL includes the resection of the epiglottis together with the pre-epiglottic fat and both ventricular folds. The vocal folds and both arytenoid cartilages are preserved. The resection can be extended to the aryepiglottic fold (medial wall of the piriform sinus), one arytenoid cartilage, one vocal fold, and/or the postcricoid area. The resection can be done either open through the neck or by the TLM approach. In open resections, the supraglottic portion of the thyroid cartilage is removed but in endoscopic resections it is usually preserved. Contraindications for open-neck and endoscopic SGL in T3 supraglottic cancer are bilateral vocal cord fixation, bilateral paraglottic space invasion, and/or invasion of the inner cortex of the thyroid cartilage at the glottic level.
In case the cancer is amenable to SGL, it must be determined whether a potential candidate is likely to compensate for the functional impairments caused by the operation. Because smoking and alcohol abuse are the major risk factors for supraglottic cancer, many patients also suffer from other tobacco-associated diseases, such as COPD. Age older than 70 years and severe comorbid diseases may exclude patients with a cancer otherwise amenable to partial resection from the operation. All authors who have reported on TLM of supraglottic cancers agree that swallowing rehabilitation proceeds more quickly and has better outcomes than open-neck SGL. 3 , 4 The rate of secondary total laryngectomy for persistent aspiration after open-neck SGL is in the range of 3.5–12.5%. 3 Due to considerable surgery-associated morbidity and postoperative functional impairment, open-neck SGL often does not qualify as a treatment option, particularly in elderly patients with preexisting poor pulmonary function. However, from clinical experience and reports in the literature, it is known that with TLM the indication for surgery can be extended to that patient group. After TLM, 95% of these patients are reported to have adequate swallowing function without the need for a gastrostomy tube. 5 , 6 , 7 , 8 , 9 The reason for this observation is that the endoscopic approach is less invasive, tracheostomy is usually not necessary and TLM does not interfere with the elevation of the larynx and the mobility of the base of tongue during swallowing. Preservation of complete glottic closure is helpful and the sensory innervation might be better by preservation of the internal branches of the superior laryngeal nerves.
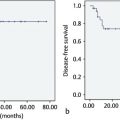
There is evidence from single center cohort studies that the oncologic outcomes following TLM are comparable to open-neck SGL and to total laryngectomy. Steiner’s group retrospectively reviewed 104 patients with pT3 cancers of the supraglottis. The 5-year overall, recurrence-free, and disease-specific survival rates were 67, 68, and 84%, respectively, thus comparable to open-neck SGL. The 5-year local control rate was 77.3% and the larynx preservation rate was 92% (97 of 104 patients). 6 Grant et al 10 reported on a series of 38 patients with supraglottic carcinoma (T1/T2 22 patients, T3/T4 16 patients). The 2-year local control rate was 97%. Ambrosch et al 5 treated 50 patients with pT3 supraglottic carcinomas (40 stage III, 10 stage IV) with TLM. The 5-year larynx preservation rate was 96%. The 5-year recurrence-free survival rate was 71%. All patients were on an unrestricted oral diet after removal of the feeding tube. Special swallowing training was not required. Peretti et al 7 reported on a series of 56 patients treated with TLM, among them 20 patients with pT3 supraglottic lesions. In 21 of 22 patients larynx preservation was achieved, the 5-year disease-free survival rate was 76.3%. Vilaseca et al 8 treated 96 patients with T3 cancer of the supraglottis. The 5-year local control rate, overall, and disease-specific survival rates were 69.8, 45.8, and 61.8%, respectively. Vilaseca et al 9 in a follow-up publication, published the up-to-now largest series including 128 patients with pT3 and 25 patients with pT4a cancer of the supraglottis treated with TLM. The 5-year laryngectomy-free survival with preserved function was 74.5%, and the 5-year overall and disease-specific survival rates were 55.6 and 47%, respectively. Recently, Ambrosch et al 11 reported a 5-year larynx preservation rate of 89% for pT3 and a 5-year disease-free survival rate of 64% for stage III and IVa supraglottic carcinomas treated with TLM.
TLM is associated with lower morbidity than open surgery and the functional results with respect to swallowing function and voice are optimal, when TLM is used as single modality. The need for postoperative adjuvant radiotherapy or chemoradiotherapy increases morbidity. Adjuvant radiotherapy is not indicated for patients with complete removal of the primary cancer and histopathologically cancer-free cervical lymph nodes. Adjuvant (chemo)radiotherapy is indicated for patients in whom microscopic residual cancer is assumed to be present at the primary site (R1 resection), in patients with more than one lymph node positive for cancer and in patients with lymph node metastases having extracapsular spread. 12 , 13 Whether postoperative radiotherapy after open-neck SGL and TLM has an adverse effect on laryngeal function is controversial. We did not see that patients receiving postoperative radiotherapy with maximum doses of 60 Gy to the larynx were more likely to need lifelong gastrostomy tube feeding or were more likely to develop airway obstruction due to persisting laryngeal edema.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree