18 Locally Advanced Glottic Cancer: Supracricoid Laryngectomy
Abstract
There are many treatment options for advanced or moderately advanced laryngeal squamous cell carcinoma (SCC). After the 1990s, chemoradiation has become the first choice of treatment for these cancers. However, other treatment options have evolved, mainly in Europe and Brazil. One good option for moderately advanced cancer of the larynx is supracricoid laryngectomy with cricohyoidoepiglottopexy (CHEP) or cricohyoidopexy (CHP). Organ preservation and local control with surgery are comparable to that of chemoradiation, although the voice is not functional in some cases. In this chapter, we discuss a patient with cT2N0M0 cancer of the glottis who has upgraded to T4N0M0 after reviewing the imaging studies. We discuss the surgical and nonsurgical treatment options. Trying to explain the advantages of this technique in treating advanced and moderately advanced laryngeal cancer, we present a comparison of vertical partial laryngectomy and supracricoid laryngectomy for patients with T2 glottic cancer, including local control and complications. We also discuss nonsurgical treatment options and other surgical options such as endoscopic laser resection. We suggest that supracricoid laryngectomy is a good treatment option in selected cases and also discuss the contraindications of the procedure.
18.1 Case Report
A 59-year-old male, trader, presented to our hospital with a history of progressive hoarseness for 4 months. He smoked one pack of cigarettes per day for 25 years. He had no comorbidies and was able to climb six flights of stairs to his apartment every day.
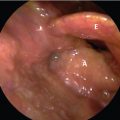
At first medical consultation, he was in a good performance status presenting with hoarseness as the main symptom. During the routine oroscopy, no lesion was identified, and the examination of the neck did not reveal any enlarged lymph nodes neck. Videolaryngoscopy, with a 70-degree optic, revealed an infiltrative white lesion of the right vocal fold reaching the anterior commissure; with reduction of the mobility of the right vocal fold, the left vocal fold was normal ( Fig. 18‑1). The disease was classified at this moment as cT2N0M0.
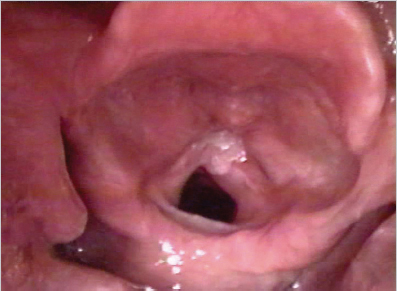
A CT scan was performed to evaluate the endolaryngeal extension A review of the scan disclosed a tumor invasion through the anterior commissure reaching to and destroying the thyroid cartilage ( Fig. 18‑2); no neck metastasis was detected. The patient was reclassified as T4aN0M0. A squamous cell carcinoma was the histopathologic diagnosis obtained following a direct laryngoscopy and biopsy.
During our service tumor board, the patient was discussed and it was suggested that the patient be treated with supracricoid laryngectomy with cricohyoidoepiglottopexy (CHEP).
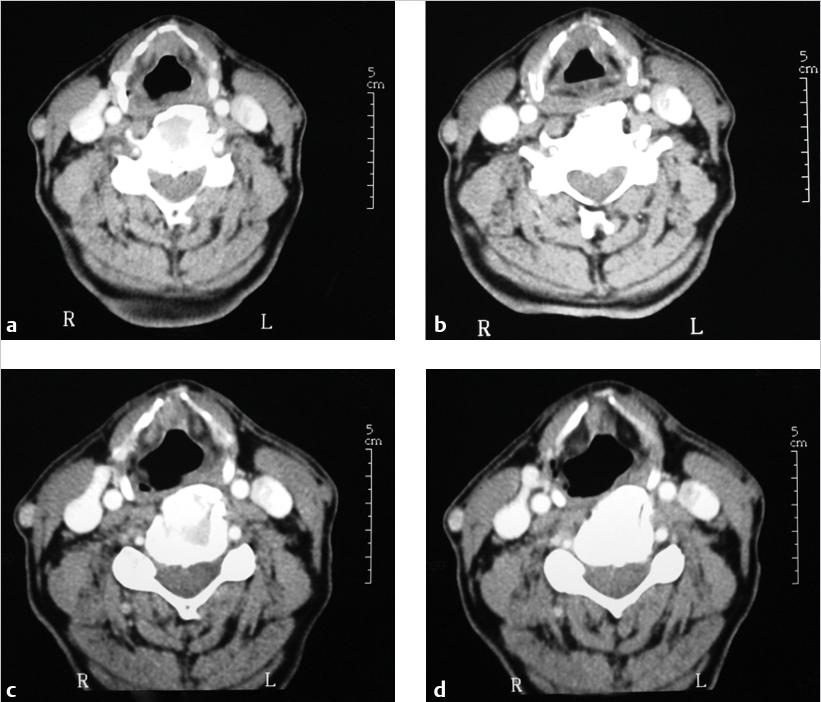
The patient underwent a bilateral lateral neck dissections, levels II to IV, and supracricoid laryngectomy with CHEP reconstruction. The entire thyroid cartilage was removed along with the paraglottic space and the vocal folds bilaterally sparing the arytenoid cartilage were ( Fig. 18‑3).
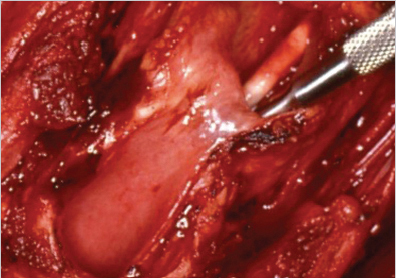
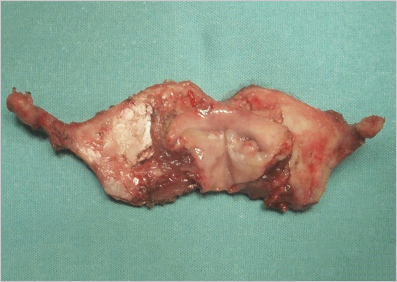
The pathology from the surgical specimen ( Fig. 18‑4) revealed squamous cell carcinoma with free margins, and focal destruction of the thyroid cartilage.
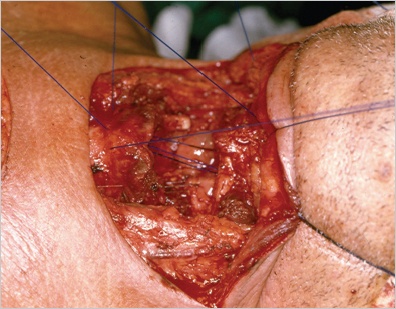
The reconstruction was with CHEP ( Fig. 18‑5).
The patient had a good outcome without fistulas or infection. He was successfully decannulated after 15 days and began oral feeding at 21 days, with successful voice recovery at 16 days. The local control was successful during 60 months.
18.2 Discussion
The conventional surgical treatment for advanced squamous cell carcinoma of the laryngeal consists of total laryngectomy or total laryngectomy and postoperative radiotherapy. 1 , 2 , 3 Since a laryngectomy results in substantial loss of function and a high degree of morbidity, organ-preservation protocols with chemoradiation have been proposed to maintain the larynx function. 4 , 5
Other surgical treatment options are near-total laryngectomy and supracricoid laryngectomy, which have been offered for patients with limited T3/T4 laryngeal cancer. 6 , 7 , 8 , 9
Supracricoid laryngectomy with CHEP has been employed to treat glottic cancer with impaired vocal cords (T2) and selected cases of fixed vocal cords (T3/T4). 9 , 10 , 11
According to Laccourreye et al 12 ( Table 18‑1), the local control and survival are better with supracricoid laryngectomy for T2 lesions.
The objective of preservation surgery for advanced cancer of the glottis is to achieve better local control while preserving the voice. A supracricoid laryngectomy with CHEP for the treatment of cancer of the glottis had its first reference in the English literature in 1990; 36 cases of CHEP were reported, mainly for T1 and T2 although cancers of the glottis; with a fixed vocal cord were excluded from this study. 13
Jean-Jacques Piquet 14 in 1991, published a study of 104 patients with cancer of the glottis treated with CHEP, 77 patients with T2 cancer and 15 patients with T3 cancer. After these two publications, this technique gained international acceptance.
Most patients come to our Department for the first time with advanced cancer of the larynx. This has influenced our team to extend the CHEP indications for selected cases of T3/T4 cancer of the glottis. The 5-year survival for all stages reported in the literature is 75 to 95%. 10 , 13 , 14
Lefèbvre and Chevalier 10 reported local recurrences in 4.8% and a 5-year overall survival of 76.8%; the most common cause of death was metachronous cancer. Chevalier et al 15 reported a 5-year actuarial local control and 5-year cause-specific survival rates for patients with a fixed vocal cord of 95.4 and 94.1%, respectively. Dufour et al 9 reported a 5-year actuarial local control of 91.4% for patients with endolaryngeal glottic and supraglottic T3 cancer. Eighty-one patients underwent CHEP and 37 patients cricohyoidopexy (CHP). In this publication, 100 patients had preoperative induction chemotherapy with cisplatin and fluorouracil.
Anatomopathological studies 16 , 17 indicated that the fixation of the vocal fold in cancer of the glottis resulted from invasion of the paraglottic space with extensive invasion of the thyroarytenoid muscle. Hirano et al 18 reported that the fixation of the vocal fold resulted from an extensive invasion of the thyroarytenoid muscle.
The survival rates reported in a series of T3 cancers treated by surgery ranges from 54 to 80%. 19 , 20
The larynx-preservation protocols successfully preserve the larynx in 50 to 66%, regarding the extent and site of the disease.
The Veterans Affairs Laryngeal Cancer Study Group 4 preserved the larynx in 101 of 166 patients (66%); 64% retained a functioning larynx. Another study carried out by Shirinian 5 reported 44% successful larynx preservation in 25 patients with cancer of the larynxstages III and IV. Lefèbvre and Chevalier 10 in a study with 207 patients who underwent CHEP preserved the larynx in 200. Ten (4.8%) presented local recurrences; 3 were salvaged with a completion laryngectomy and 7 were not salvaged. In the same study, 17 patients had stenosis and 7 required a permanent tracheostomy. Although only 16 patients were T3 cancer of the glottis, the overall larynx preservation rates were 96.6%, with 91.8% full-functioning larynx.
Endoscopic laser resection for T3 laryngeal cancer has been reported in the international literature as a laryngeal preservation option. Motta et al 21 in a study of 516 patients with cancer of the glottis treated by endoscopic laser resection reported only 7.1% with T3 carcinoma. Other published series 22 , 23 with more than 100 patients did not include T3 cancer of the glottis in the group of glottic cancers treated by endoscopic laser resection. Thirty-eight patients in our series 24 retained their larynx over a 5-year survival period. Our successful overall laryngeal preservation rate was 83.7%.
The differences in survival of patients with invasion of the laryngeal cartilage and exolaryngeal extension have been reported. 25 The occurrence of thyroid cartilage erosion or invasion by the cancer without reaching the exolaryngeal tissues have not been correlated with the prognosis.
A previous study at our institution demonstrated the importance of careful evaluation by imaging in the correct staging of cancer of the glottis. 26
A previous study conducted in our Department revealed pathological cartilage invasion in a surgical specimen of 11 patients; this finding did not influence the survival rates. 24
One controversy regarding the treatment of cancer of the glottis is the elective neck dissection associated with CHEP, because of the low rate of neck metastasis in this group of patients (9%). 15
Previous publications 27 revealed a 10% incidence of occult neck metastasis in cancer of the glottis. In these publications, the overall rate of metastasis for cancer of the glottis was 22.2%, with extra capsular spread in 12 (37.5%) patients. Another option, instead of elective neck dissection associated with CHEP for T3 tumors, is the watchful-waiting attitude; nevertheless, the rates of salvage neck dissection are as low as 11 to 56%. 28 , 29
Successful decannulation with CHEP ranges from 93 to 98%. 30 , 31
Naudo et al 32 reported a 9-day mean time to decannulation and found a relation between increased time with tracheostomy and advanced age and postoperative edema of the arytenoid. Bron et al 33 reported a 27-day mean time to decannulation; 62 patients with one arytenoid cartilage resected presented a mean time with tracheostomy of 29 days. Nine patients had no arytenoid resected, with a mean time to decannulation of 36 days.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree