20 Locally Advanced Glottic Cancer: Supratracheal Laryngectomy
Abstract
Following the current European Laryngological Society (ELS) classification, supratracheal laryngectomy (STPL) or type III open partial horizontal laryngectomy (OPHL) is an OPHL aimed at resecting some intermediate to advanced glottic cancers with subglottic extension. Furthermore, type III OPHL represents the most extensive function sparing surgical option currently available in the surgical armamentarium. In selected patients, STPLs show promising long-term oncologic and functional outcomes, similar to those of supracricoid partial laryngectomy. The core indication for STPL is glottic/transglottic cT3 cancer with subglottic extension ≥10 mm from the free edge of the true vocal cord, calculated at its midline. Other local indications are cancer of the glottis (T2) tumors with anterior subglottic extension reaching the cricoid ring and some selected cT4a with limited anterior or lateral extralaryngeal extension. The application of STPL in the context of a modular surgical approach to the larynx affected by intermediate/advanced cancer can be considered a valid and effective therapeutic choice, not only in terms of oncologic results but also with regard to functional outcome. The main criticisms of STPL are poor voice quality outcomes, slight dysphagia with aspiration pneumonia, and soft-tissue laryngeal stenosis occurring in about 20% of cases.
20.1 Clinical Case 1
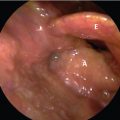
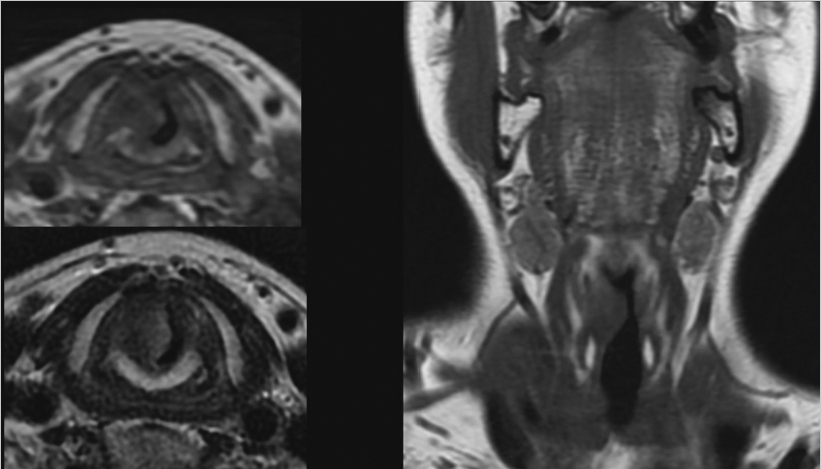
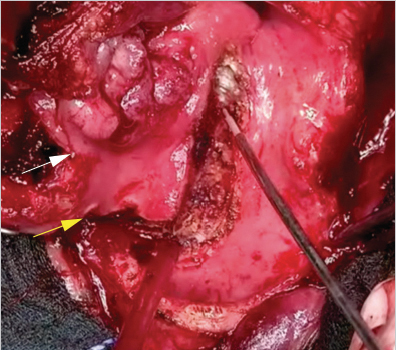
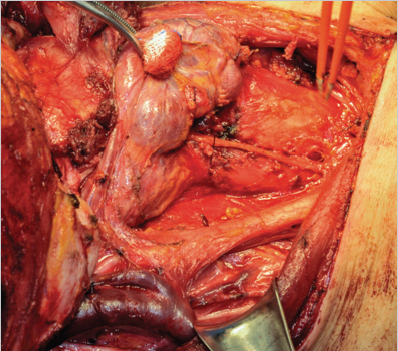
This patient was a 63-year-old male, in good general condition, with a Karnofsky index of 90, and who was a drinker and a cigarette smoker. Because of persistent dysphonia, he underwent laryngoscopic examination during which a suspected glottic neoplasm with subglottic extension was identified, with vegetating aspects, involving the right hemilarynx, with fixation of the true vocal cord (TVC) and arytenoid. Nopalpable lymph nodes were present. During the evaluation of the patient, neck MRI with surface coils ( Fig. 20‑1) and CT scans were performed disclosing a glottic tumor with subglottic extension of about 10 to 12 mm from the free edge of the TVC measured at its midline, involvement of the superior and inferior paraglottic space, no involvement of the thyroid cartilage wing or the cricoid plate, apparent involvement of the anterior commissure, involvement of the cricoarytenoid joint, and absence of cervical and/or level VI pathologic lymph nodes. In the course of direct microlaryngoscopy, subglottic extension of about 12 mm was noted; posteriorly, the margin between the lesion and the posterior commissure was 3 mm. The pathological report on the biopsy sample revealed a squamous cell G2 carcinoma staged as glottic cT3N0. During the tumor board meeting, an open partial horizontal laryngectomy (OPHL) type III was proposed as the first therapeutic option or, as an alternative, concurrent chemoradiotherapy. The patient chose the partial laryngectomy option. A CO2 fiber laser OPHL type IIIa + right cricoarytenoid unit (CAU) + selective neck dissection (SND; levels II–IV) + right tracheoesophageal groove dissection was carried out; all margins were free of cancer (> 2 mm). During the resection, a supracricoid access was made demonstrating the insufficiency of safe margins with this approach ( Fig. 20‑2); this is a clear example of the usefulness of OPHL type III in the modular surgical approach strategy using OPHLs.
Final staging based on biopsy specimen was glottic pT3N0 and there was no indication for adjuvant radiotherapy. The postoperative course was uncomplicated, swallowing recovery was conducted without cannula, and the patient was discharged 18 days after the operation, with the tracheostoma still open but occluded with a gauze dressing, which the patient removed during the night. The tracheostoma underwent a spontaneous closure within 30 days after the operation. Two years after surgery, the patient is free, manages to lead a normal life without tracheostomy, and his weight is stable. During this period, no episodes of aspiration pneumonia have been reported.
20.2 Clinical Case 2
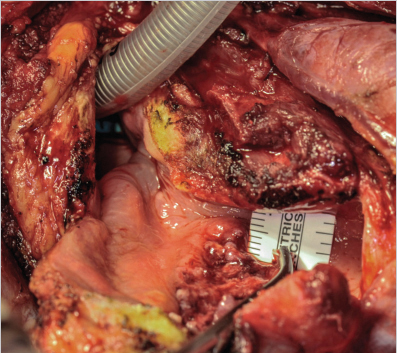
This was a 57-year-old male, in perfect general health, a current cigarette smoker, with a Karnofsky index of 100, and without any comorbidities. Because of persistent dysphonia, he underwent phoniatric examination during which an ulcerated glottic neoplasm with subglottic extension was discovered, involving the right hemilarynx, apparently extending from the anterior to the posterior commissure, and showing fixation of the TVC and arytenoid. No palpable lymph nodes were present. During the evaluation, MRI of the neck with surface coils ( Fig. 20‑3) was performed, demonstrating a glottic cancer with subglottic extension of about 15 mm from the free edge of the TVC at its midline, involvement of the superior and inferior paraglottic space, full-thickness involvement of the inferior aspect of the thyroid cartilage wing and possible involvement of the cricoid plate, apparent involvement of the anterior and posterior commissure, involvement of the cricoarytenoid joint, and absence of cervical and/or level VI pathologic lymph nodes. In the course of direct microlaryngoscopy, a subglottic extension of about 14 mm was noted; posteriorly, the margin between the lesion and the posterior commissure was approximately 3 mm. The pathological report on the biopsy sample revealed a squamous cell G2 carcinoma staged as glottic cT4aN0. During the tumor board meeting, a total laryngectomy + SND (levels II–IV + VI) + primary tracheoesophageal puncture (TEP) was proposed as the first therapeutic option, which the patient absolutely refused, expressly asking to be submitted to the therapeutic option allowing him the greatest guarantee of preservation of the larynx. Faced with the two options represented by concurrent chemoradiotherapy and OPHL type III, the patient chose the latter, considering also the potential better degree of freedom from total laryngectomy. After signing an informed consent that also included the option of an intraoperative conversion from partial to total laryngectomy based on the real extent of the tumor, an OPHL type IIIa + right CAU + SND (levels II–IV) + right tracheoesophageal groove dissection ( Fig. 20‑4) was carried out. The posterior margin of resection was close ( Fig. 20‑5) but free from tumor (2 mm). Final staging of the specimen was pT4aN0 due to minimal thyroid cartilage and cricoid arch and plate involvement, there was no indication for adjuvant radiotherapy.
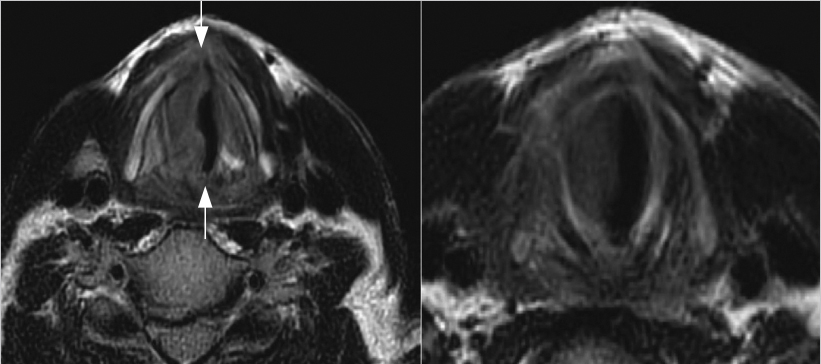
The postoperative course was uncomplicated, swallowing recovery was conducted without cannula, and the patient was discharged 14 days after the operation, with the tracheostoma still open but occluded with a gauze, which the patient removed during the night. The patient complained about the persistence of obstructive sleep apnea syndrome when he tried to keep the tracheostomy occluded during the night. This was studied by sleep endoscopy during which a double obstruction of the neoglottis was observed caused by a preexisting hypertrophy of the base of the tongue together with a mucosal flap of the hypopharyngeal mucosa on the side of the resected CAU. On two occasions, the patient was subjected to refinement of the base of the tongue and neoglottis by CO2 laser and was definitively decannulated within 3 months postoperatively. Three years after surgery, the patient is cancer free, leads normal life without a tracheostomy, practices sports, his weight is stable, and he occasionally makes use of C-pap ventilation during the night. During this period, no episodes of aspiration pneumonia were reported.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree