html xmlns=”http://www.w3.org/1999/xhtml”>
Chapter 17
The role of assistive technology in the care of people with dementia
Introduction
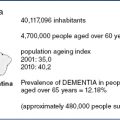
Our rapidly ageing population has led to considerable concern as to whether existing health and social care provision will cope with such an increased future demand and established an urgent need to explore alternative, innovative solutions to this challenge [1]. This chapter will use examples of research and innovation in the provision of assistive technology in dementia care from the UK, but we hope that these will be helpful to our international readers. In the UK, national policy has over the last two decades continued to emphasise the need for the care of older people, including those living with dementia, to be based in the community and for them to remain in their own homes for as long as possible [2–6]. Assistive (or enabling) technologies provide one possible solution to promote autonomy and independence for older people [7], but in the UK they are still underutilised in routine care [8,9]. A series of current UK research studies is exploring the effectiveness of assistive technologies in the care of older people and those with long-term illness and how they can become better integrated into usual care. In England, the Department of Health Whole System Demonstrator (WSD) programme was set up in 2009 as a randomised controlled trial of telecare and telehealth in chronic illness management on three sites [10]. In Scotland the Joint Improvement Team ran a National Telecare Development Programme from 2006 to 2011. The aim was to consider the range of devices and services that harness developing technology to enable people to live with greater independence and safety in their own homes, and to support the implementation of the use of those devices [11].
The words that are used to describe the use of assistive technology include
- Telecare: to facilitate independence and enhance personal safety. Devices include community alarms, sensors and movement detectors, and the use of video conferencing or ‘Skype’ to allow visual and auditory communication with carers. This has been described by the WSD programme as a ‘service aimed at vulnerable people who need the support of Social Care or Health Services to keep living on their own. For example, those with physical disabilities, the frail and elderly or those suffering from dementia or epilepsy’ [10].
- Telehealth, which facilitates the monitoring of long-term health conditions and bodily functions for clinicians at a distance to offer support and is described by the WSD as a ‘service aimed at helping people manage their long term conditions in their own home’ [10]. Dementia is not listed as an example of a long-term condition at this point.
- Environmental controls, which are often used to give a disabled person the capacity to control many aspects of the home environment from a single unit. For a person with dementia the environmental controls may eventually be operated by someone else or automated.
- Leisure equipment such as touch screen monitors which can be an easy way to access reminiscence materials or entertainment such as music, films or photographs, or games specifically designed considering the impairments that are associated with dementia. They are also used for communication.
- Dementia-friendly design, where the whole environment is considered as a way of helping the person with dementia to live independently or to reduce the burden of care on the family, or others who provide care and support. Environmental design equipment can also include innovations such as the controlled emission of odours to signal the time of day and to encourage appetite [12].
The term ‘assistive technology’ is often assumed to refer only to sophisticated equipment that uses electronic information and communication technology. In reality the term can refer to quite simple devices such as a modified sink plug, which can prevent flooding when someone is forgetful in the kitchen and bathroom and leaves an unattended bath or sink. The plug is activated by the pressure of the water or the sink and will open and release the excess water down the plughole to avoid flooding (http://www.magiplug.com). It is a small, inexpensive, easily available, mechanical device requiring no maintenance and no new skills to use. It presents no ethical dilemmas. By the definition assumed in this chapter, that plug is both ‘assistive’ and ‘technology’.
Another assumption in this chapter is that the ‘kit’ or equipment that is brought into use should never be introduced in isolation, but only as part of a strategy of care that includes the provision of information and support, health advice and advice on design of the environment:
‘We’ve put in a movement sensor in my mother’s bed room which means that when she gets out of bed during the night, the toilet light switches on automatically. We know her really well and that is usually where she is planning to go when she gets up at those times. In an attempt to reduce the number of times she gets up at night, I have started to take her for a walk in the daylight every morning, which helps to set her body clock. We’ve also changed the light bulbs. They are still energy saving, but her old ones had lost their luminosity over time, and were a bit dull, so these new ones light up faster and provide stronger light to help her orientate herself. And we’ve put a sign on the toilet door. We’re not sure how significant any of these things are individually, but the situation is better now at night.’
In this example, the sensor that switches on the light is the only electronic part of the assistive technology solution, but works with the advice on exercise, design and lighting to alleviate a nocturnal problem which is very common for people with dementia and their carers (although telecare can of course help all older people).
The quality of life of people with dementia and those who care for them can be enhanced significantly by the thoughtful use of assistive technology. It is an important part of normal dementia care to provide access to aids, particularly when the technology is low cost and accessible. It is important for people with dementia, their families and professionals who support them to be aware of the sort of technological equipment that is available and to develop the skills needed to use the equipment well, including the capacity to undertake simple maintenance tasks. As well as knowing what is already on the market, health and social care professionals and other workers including service managers should be aware of emerging useful devices and have a strategic approach to keeping up to date with what is being developed in this dynamic field. It is also their responsibility to communicate with designers, inventors and entrepreneurs to make sure that increasing energy is put into the creation of new technologies [13] which, because it is useful and taken up by care organisations and individual people, will be of commercial value to the industry, which in turn will stimulate greater inventiveness and ultimately benefits for patients and clients.
Why is assistive technology in use in dementia care?
There is considerable variation in how assistive technology is used in dementia care. In some countries a wide range of technology is readily available, with assessment of individual need and implementation integrated into a routine social care assessment. For example, in 2009, a programme of provision of telecare was implemented in Scotland for anyone living at home over the age of 60 who wanted it, thus ‘mainstreaming’ a strategy of capacity building and encouraging people to grow old where they are. The evaluation noted positive effects on
- staff working in a new culture of care, emphasising support and capacity building
- client satisfaction
- quality of life for both older people and unpaid family caregivers
- the ability of a local (municipal) authority to deliver on performance indicators and the supply of good-quality services at low cost [14].
There was clear learning from the programme. Early intervention appears to be important in housing solutions for people with dementia. People with dementia can build capacity in this way. The role of committed and skilled staff is crucial because of the need to focus on what people with dementia can do, rather than focusing on their disabilities. The researchers were keen to point out that ‘mainstreaming’ (a term which indicates that everyone is being given some basic assistance) carries the danger that those with particular needs such as those with dementia wind up being marginalised. Their greatest emphasis was on the fact that it was not the assistive technology in isolation that enabled the success of the programme, but the whole system. However, it is clear that using assistive technology improved cost and quality of care.
The role of assistive technology in supporting family carers
In the UK (as in many countries) most people with dementia live independently in the community, with one-third residing in care homes; around half a million family carers provide the mainstay of community support to the former [15]. Carers of people with dementia are more likely to experience worse physical and mental health and to report a higher care burden compared with carers of people with other long-term conditions [16]. A systematic review of the effectiveness of networked technology in supporting family carers of people with dementia revealed that the technologies had moderate effects on carer stress and depression [17].
Assistive technologies have the potential to help reduce the burden of care for family carers. Describing care as a ‘burden’ shapes our frame of reference in a negative way. In order to get improved services and to raise money for third-sector organisations, the negative aspects of caring are often emphasised in public. The perception of many health and social care workers is further shaped by the fact that they are more often involved when the situation is in crisis. Looking after your family is actually still an important part of our society across many cultures (see the chapters in Section IV) and people do it willingly in general. Many families are glad to care for a person with dementia for as long as possible. Having a carer living with you at home has been said to reduce the likelihood of institutionalisation by up to seven times [18]. Carers mostly do not undertake this work under duress, but out of loyalty and long-standing commitment, and a sense that this is what life is about – caring for each other. But for many of them care is more burdensome than it needs to be. Without some basic information and advice the carer spends more time, has more adverse incidents and opportunity costs and may spend more money than is absolutely necessary. Carers need access to assistive technology so that the energy they are devoting to the person with dementia can be focused on other aspects of their own, and their family’s needs, such as getting a decent night’s sleep.
For staff working in hospitals and care homes or other residential settings, a concern is often expressed that technology ‘replaces caring’. Of course this is theoretically possible. The invention of a robot nurse might give rise to concern that dependent people might one day never see a human again [19]. As it happens, the robot nurse, if the face was not painted on it, and it did not have a voice generator in it, is really a rather splendid hoist, for moving and handling physically dependent people in a way that is superior to the mechanical cranes that have been commonly used in hospital and other settings. When in production this may turn out to be safer for staff as well as being comfortable for patients.
Other concerns are expressed about movement sensors and methods of electronic observation, which are seen to replace the watchful eye of the friendly nurse. Again, the framing of the dichotomy is misleading. The question is not whether we would prefer a person to be watching over us or a machine. The real question is whether we would like to be protected at all, and in what way? In reality a nurse or carer cannot be watching all the time, unless the patient or resident is in an open plan area like an old Nightingale hospital ward and the staff have nothing else that they have to do. If you want privacy in an individual room, but you are vulnerable, the compromise may be that you agree to unobtrusive electronic monitoring. Any staff time and energy can then be focused on those things for which there is no satisfactory assistive technology application, like dancing with or sharing a meal with the person with dementia.
The ethics of the use of assistive technology
In practice, there are mental capacity issues and decision-making responsibilities that arise at some point along the journey of the person with dementia. However, not all are raised with everyone and in some cases some issues arise quite late on, or not at all, if sufficient preparation has been made and advanced directives and proxy forms of decision-making have been put in place in good time. Giving maximum control to the person for as long as possible is crucial. The person with dementia may be reluctant or refuse to accept assistive technology and even if staff or families wish to overrule them because the decision being made seems unwise, the person may want to retain their right to control their environment. If the decision is taken to overrule the person with dementia, this should be done cautiously and with a proper understanding of how serious this is. In particular, a difficulty in communicating with a person with dementia must never be interpreted as making them incompetent to make a decision. There are mechanisms that can be used to find out what people with dementia think and want which are easily available and simple to use, for example, talking mats (http://www.talkingmats.com). In addition, some skilled communicators have a highly developed capacity to hear the voices of people with dementia who others think are beyond contact.
A recent literature search on the use of assistive technology in the care for community-dwelling elderly people suggested that the necessary ethical debate appears not to be a priority [20], with the exception of care homes [21]. Issues in the public domain which give greatest rise to debate are often centred on tracking devices, seen as problematic because of the association of their use in the criminal justice system for tagging offenders on parole. The families showed higher support for tracking devices both for the independence and safety of the relative in their care and for their own peace of mind, particularly if the device is user-friendly, whereas professional staff are particularly concerned about the autonomy of the person with dementia and minimising their risk of harm [22]. This balance between a person with dementia’s right to independence and a professional carers’ duty to minimise harm is a core issue in decision-making about the use of assistive technology [23]. This short chapter is too brief to cover ethical issues in depth, but it is important to highlight that for many people with dementia the views of family or professional carers are taken as a proxy for their own views, even when they are still competent to express a view [24]. This is clearly not acceptable unless the person with dementia has delegated this responsibility and is no substitute for consulting that person.
Because it is important to remember that the person’s individual choices and beliefs are an important consideration, health and social care staff need to be conscious and aware of their own beliefs and prejudices. Because these situations are complex, it is difficult to produce a checklist or guide that will make clear what is right or wrong in every situation. Cox et al. describe a set of core values when making decisions concerning people with dementia: people should make sure that
- the person using the service should have the maximum control
- real and informed choice should be a key part of any service
- people who use the service should be valued and respected as unique individuals
- continuity of care is built into service delivery in a way that keeps the person in touch with their past and present
- the person is not discriminated against because they have dementia or because of any other differences and they receive their fair share of good quality and appropriate services [25].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree