The Czech Republic
The Czech Republic has a long history of dementia research. It is the homeland of Oskar Fischer (1876–1942) who first described the presence of plaques and tangles in 12 cases of presenile dementia, compared to one case described by Alois Alzheimer (1864–1915) [1]. Arnold Pick (1854–1924), working in Prague, found swollen brain cells known as Pick cells, together with abnormal staining within cells (Pick bodies) in a patient with fronto-temporal atrophy.
The Czech Republic has approximately 10.5 million inhabitants. According to the latest prevalence rates we estimate that there are about 125,000 people with dementia. The diagnosis is mostly established by neurologists in the earlier stages, while psychiatrists and geriatricians deal mainly with people in the moderate and severe stages [2]. There are approximately 11,400 people per 1 neurologist, 10,800 people per 1 psychiatrist and 51,500 people per 1 geriatrician. These numbers are comparable to other central and eastern European countries [3].
Prescribing of cholinesterase inhibitors (ChEI) and memantine is limited to these three specialties. Insurance companies require Mini-Mental State Examinations (MMSE) every 3 months for the reimbursement of cognitive drug therapy. ChEI therapy is covered within the 13–25 range of MMSE score and memantine in the range of 6–17, allowing for dual therapy reimbursement in the range of 13–17, which is quite regularly prescribed [2]. In case of ChEI intolerance, memantine can be prescribed free of charge up to a MMSE score of 19.
With average catchment areas of 1500–1800 people per GP, it is estimated that one GP should have 15–20 patients with dementia (while only approximately 2–4 patients are actually referred to specialists who can prescribe ChEI) [4]. About half of dementia patients seek specialist help directly. There is still a relatively high use of nootropics, vasoactive substances and other non-evidence-based therapy. This might be partially due to insurance companies constraining the use of ChEIs to patients with MMSE scores below 25, yet are deemed clinically to have AD. It may also be the result of underdiagnosis by GPs, who aren’t allowed to prescribe anti-dementia medication. Reimbursement of non-evidence-based medications is likely to be revoked during 2012 while insurance companies expect a gradual increase in usage – and therefore cost – of ChEIs. However, patents of ChEIs have expired, lowering the cost.
National recommendations for diagnosis and treatment are comparable to European guidelines [5], which were translated and adapted for the Czech Republic and its specific environment [6,7].
There are over 10 specialist sites dealing with AD, some involved in research and most attached to universities. There are four laboratories measuring cerebrospinal fluid tau, phosphorylated tau and beta-amyloid levels. The main obstacle for such tests to be freely available is the lack of reimbursement by health insurance providers and uncertainty about cut-off and normative values, yielding different results across laboratories. They are therefore used primarily for research rather than clinical diagnostic purposes [8].
The Czech Republic is participating in many European Union (EU) projects, such as the EU Joint Program on neurodegenerative diseases. One other key example of Euro-Atlantic cooperation is an EU-funded collaborative project in cardiology and neurology, that is, the International Clinical Research Centre Brno, which in part focuses on AD epidemiology and collaborates with the Mayo clinic, Rochester, USA. Czech researchers participate in the INTERDEM international research group on psychosocial interventions in dementia and are active in the field of palliative care, collaborating on recommendations for end-of-life care [9].
The Czech Alzheimer Society (CALS, established in 1997) is an active member of Alzheimer’s Disease International and Alzheimer Europe (current vice-president of Alzheimer Europe is the delegate of CALS) and is involved in many national activities. Memory Days is a project focusing on early diagnosis and case finding of dementia, funded by different sponsors and supported by independent experts. Project GOS (Gerontological and Organisational Supervision) aims to improve care in residential facilities in Southern Moravia. Improvement of long-term care provision is one of the goals of CALS, and there is since 2011 an international collaboration: ELTECA (Exchange of Experiences in Long-term Care).
In 2011, leading experts established the Alzheimer Foundation with the objective of supporting young scientists and research in the field of AD and related disorders.
Although the Czech Republic is internationally very active in AD research, there is still no national Alzheimer or Dementia plan. In early 2011, a task force was approved by the Czech government to design concept solutions for AD and similar diseases (‘Alzheimer Plan’), the aim being to analyse the current situation of people with dementia and their carers and to create health care, social, educational and research measures to improving their care. The various government departments involved pledged to finalise this plan by June 2011, but further steps were not taken until early 2012.
Acknowledgement
Supported by Grant Agency of the Czech Republic Grants 309/09/1053; European Regional Development Fund – Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123)
References
1. Goedert M (2008) Oskar Fischer and the study of dementia. Brain 132(4):1102–1111.
2. Sheardova K, Hort J, Rektorova I, Rusina R, Linek V, Bartos A (2012) Dementia diagnosis and treatment in Czech neurological and psychiatric practices. Cesk Slov Neurol N 75/108(2):208–211. in print.
3. Bartos A, Kalvach P, Trošt M, Ertsey C, Rejdak K, Popov L, et al. (2001) Postgraduate education in neurology in Central and Eastern Europe. Eur J Neurol 8:551–558.
4. Hort J (2011) Nová guidelines pro diagnostiku a léčbu Alzheimerlovy choroby. Neurol Prax 12(4):277–281.
5. Hort J, O’Brien JT, Gainotti G, Pirttila T, Popescu BO, Rektorova I, et al. (2010) EFNS Scientist Panel on Dementia. EFNS guidelines for the diagnosis and management of Alzheimer’s disease. Eur J Neurol 17(10):1236–1248.
6. Sheardova K, Hort J, Rusina R, Bartos A, Linek V, Ressner P, et al., za Sekci kognitivní neurologie České neurologické společnosti ČLS JEP (2007) Doporučené postupy pro léčbu Alzheimerovy nemoci a dalších onemocnění spojených s demencí. Cesk Slov Neurol N 70/103(5):253–258.
7. Ressner P, Hort J, Rektorová I, Bartos A, Rusina R, Linek V, et al., za Sekci kognitivní neurologie České neurologické společnosti J. E. P. (2008) Doporučené postupy pro diagnostiku Alzheimerovy nemoci a dalších onemocnění spojených s demencí. Cesk Slov Neurol N 71/104(4):494–501.
8. Hort J, Bartos A, Pirttilä T, Scheltens P (2010) Use of cerebrospinal fluid biomarkers in diagnosis of dementia across Europe. Eur J Neurol 17(1):90–96.
9. Gove D, Sparr S, Dos Santos Bernardo AM, Cosgrave MP, Jansen S, Martensson B, et al. (2008) End-of-Life Care for People with Dementia. Luxembourg: Alzheimer Europe.
Hungary
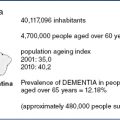
Epidemiology
To date no systematic survey has explored the prevalence of dementia in Hungary, but estimates can be extrapolated from two surveys conducted in general practice:
Rates in both surveys are higher than internationally published data, probably because they were conducted in general practice rather than in general population cohorts [3]. Besides this selection bias, significant alcohol consumption in the Hungarian population may be contributing to the higher prevalence of dementia [4]. Based on the above, it was estimated that between 150,000 and 300,000 Hungarians suffer from dementia [5].
An important finding is the high prevalence of vascular dementia as a result of high overall vascular morbidity [6,7]. In a recent study, neurodegenerative pathology was found in 81% of the brains of patients with clinical dementia, with 43% showing vascular pathology and the rate of mixed cases being 25% [8].
In spite of the somewhat lower life expectancy in Hungary (70 for men, 78 for women [9]) the proportion of elders (≥65) has grown from 15.1% in 2001 to 16.3% by 2009, as a result of decreasing number of childbirths. Hungary is fast becoming one of the oldest countries in Europe, a significant burden on the economy [10].
Empirical evidence shows that health or social issues related to milder dementia are less important in Hungary compared to more developed countries. For instance, elderly Hungarians can manage their daily life without driving while their American counterparts cannot. Many old people live close to relatives in Hungary, which is less typical in, for example, the USA. A diagnosis of dementia is highly stigmatising and as such it discourages patients and their families to seek help early.
In 2002, there were 78,000 outpatient visits for dementia [11]. Based on these data, the estimated number of newly diagnosed cases was <5000. Of these, only about one-fifth were seen in specialist psychogeriatric services. Similarly low was the number of guardianship orders because of inability to manage affairs [12].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree