There are strengths and weaknesses to formulating an action plan in this way. It is simple, so tasks can be chunked into manageable bits, but it may miss sub-steps. Mapping the data from the reports and enquiries summarised by Andrew Chidgey for England onto this framework results in an outline with which to draft an effective narrative (see Box 9.2).
1Improving Services and Support for People with Dementia. London, National Audit Office, 2007.
2Public Accounts Committee. Improving Services and Support for People with Dementia. London, TSO, 2008.
In this, in England, we had the bones of our clear story. The next step was to articulate it as a whole and ensure that everybody comes to be telling it the same way. In terms of the Heath brother’s formulation of message types, this is one that moves from common sense (‘dementia is bad’) to uncommon sense (‘we should spend to save’) [9]. It has elements that correspond to the SUCCESs framework they suggest can help an idea or message to become ‘sticky’. In this the narrative below (see Box 9.3) is
- Simple – finding the core of the idea – it’s bad, it’s big, we can do something
- Unexpected – grabbing attention by surprising them – more than stroke, heart disease and cancer put together
- Concrete – an idea that can be grasped and remembered later – 700,000 people, £17 billion
- Credible – believability – evidence based, referenced
- Emotional – so people see the importance – use of adjectives to describe impacts
- Stories – empower people to use an idea through narrative – a single through line
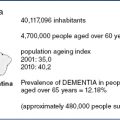
In the UK we have 700,000 people with dementia and 200,000 new cases a year. It is a devastating disorder for those affected causing irreversible decline in global intellectual, social and physical functioning. The cost of caring for people with dementia is immense, £17 billion per year, greater than stroke, heart disease, and cancer put together. There are major problems with the health and social care system for dementia. Only a third of people with dementia ever receive a diagnosis and then often late in the illness when it is too late to prevent harm. There are misconceptions that nothing can be done for dementia. This is not true. There is a vast amount that can be done to enable people to live well with dementia. Finally, better dementia care is cheaper than the poor quality care we now provide (including £8 billion pa on care home places). We need to change the system to improve diagnosis and care; this will improve the quality of life of people with dementia and their carers and save money by reducing unnecessary institutionalisation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree