WHY ARE BONE MASS MEASUREMENTS PERFORMED?
There are three clinical applications for bone mass measurement. Each has a distinct value in clinical decision making. The three applications are
Diagnosis of osteopenia or osteoporosis (see Chap. 64).
Fracture risk prediction.
Serial monitoring to measure response to interventions, diseases, or medications that affect bone.
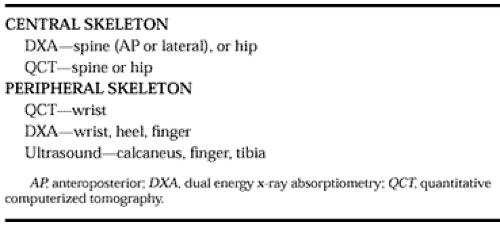
Clinicians have at their disposal various devices that measure bone mineral density. These devices are characterized as central or peripheral. Central devices measure the spine or the hip and peripheral devices measure the wrist, heel, finger, or tibia. These devices are listed in Table 57-3.
For each of the three applications of bone density measurements previously listed, the central and peripheral devices have advantages and disadvantages.35,36
THE DIAGNOSIS OF OSTEOPENIA AND OSTEOPOROSIS
The diagnosis of osteopenia (T score of <-1.0 but >-2.5) is clinically important, independent of fracture-risk assessment, for
the initiation of early postmenopausal prevention strategies. This diagnostic category represents the range of bone density for which prevention strategies were designed. It has been shown that the recognition of low bone mass in early post-menopausal women facilitates the acceptance of hormone-replacement therapy (HRT).37,38 This observation will most likely be the same for other preventive interventions in early postmenopausal women.
the initiation of early postmenopausal prevention strategies. This diagnostic category represents the range of bone density for which prevention strategies were designed. It has been shown that the recognition of low bone mass in early post-menopausal women facilitates the acceptance of hormone-replacement therapy (HRT).37,38 This observation will most likely be the same for other preventive interventions in early postmenopausal women.
The utility of central or peripheral devices for the detection of osteopenia is dependent on the age of the patient and the particular skeletal site measured. In early menopausal patients, it is more likely that a diagnosis of osteopenia or osteoporosis will be missed if only one skeletal site is measured. In the elderly, bone mass may be more concordant at various skeletal sites. This reduces, but does not abolish, the likelihood of missing a diagnosis of osteopenia or osteoporosis if only one skeletal site is measured. The exception to the ability to use a single measurement in the elderly is the anteroposterior (AP) spine study by DXA. The AP spine measurement by DXA is frequently falsely elevated by osteophytes and/or facet sclerosis of the posterior elements; this may lead to underdiagnosis in this population.39 In the elderly, all peripheral and central measurements, with the exception of the AP spine measurement by DXA, have nearly equivalent value for diagnosing osteopenia or osteoporosis.27,40,41 There are fewer prospective fracture data for lateral spine DXA measurements. However, there is a strong correlation between lateral spine DXA BMD and spine quantitative computerized tomography (QCT) BMD, the latter of which has adequate fracture data. This suggests that low lateral spine DXA values should predict increased fracture risk in the elderly.42,43
BMD is more discordant throughout the skeleton in the early menopausal population than in the elderly (older than 65 years) population.27,40,44 There are at least four potential explanations for this discordance:
Differences in development of PABM at various sites.45
Differences in rates of age-dependent bone loss between cancellous bone and cortical bone after the menopause.
Differences in the accuracy of measuring BMD using various techniques.
T scores being derived from different young normal databases.
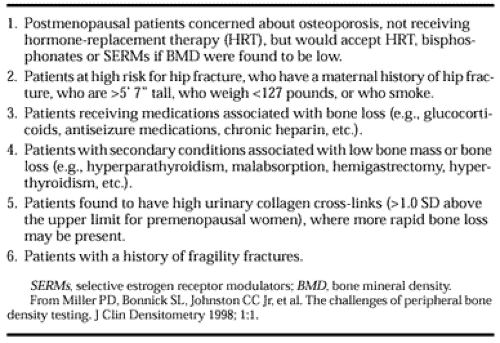
Data suggest that in early menopausal women, if one skeletal site is osteoporotic (T score <-2.5 SD), there is a <10% chance that another skeletal site will be normal (T score >-1.0 SD).27,46 Studies have not yet clarified how many early postmenopausal women have normal BMD at one site and osteopenia at another. These numbers may not be insignificant. Bone mass measurements can be used to “rule in” a diagnosis of low bone mass, but cannot be used to “rule out” a diagnosis (i.e., if they are normal). Hence, many early menopausal women will need additional BMD testing if a single skeletal site is normal to avoid missing an abnormal measurement at another skeletal site. This is particularly true in women with additional risk factors for low BMD or when a diagnosis of osteopenia would change the pharmacologic intervention. Patients with a normal single skeletal site BMD who may need additional testing are described in Table 57-4. These guidelines will minimize the potential for misdiagnosis.47
There are other patient populations in which a diagnosis of osteopenia may change intervention strategies. The prevention of bone loss associated with glucocorticoid therapy is recommended in patients with T scores <-1.0.48 It may also be appropriate to intervene in other medical conditions associated with bone loss (i.e., hyperthyroidism [see Chap. 42], hyperparathy-roidism [see Chap. 58], posttransplantation, etc.) based on a finding of osteopenia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree