Introduction
Weight loss is common in older adults and is a harbinger of poor outcome. A loss of 10% or more of body weight between age 50 years and old age is associated with a 60% increase in mortality compared with persons with stable weight.1 Involuntary weight loss greater than 4% of body weight is an independent predictor of increased mortality in older community-dwelling male veterans. Over a two-year follow-up period, mortality rates were substantially higher in the 13% of the population with involuntary weight loss (28%) than in those who did not lose weight (11%), even after adjusting for baseline age, body mass index, tobacco use and other health status and laboratory measures.2
Weight loss is strongly associated with a 76% increase in mortality risk among home-bound older adults, along with male gender and age. This effect of weight loss persists after adjusting for initial body mass index (BMI) (the weight in kilograms divided by the height in metres squared), smoking, health status and functional status.3
In nursing home residents, a 10% loss of body weight over a six-month interval strongly predicted mortality in the ensuing six months.4 When compared with controls, the 16% of subjects who lost at least 5% of their body weight were 4.6 times more likely to die within 1 year.5 In another study of long-term care residents, a 10-fold increased risk for death was seen for persons who lost 5% of their body weight in any month compared with those who gained weight.6 For this reason, the United States Long-Term Care Minimum Data Set defines a loss of greater than 10% of body weight within 180 days or 5% within 30 days as an important clinical threshold for triggering resident assessment protocols.7
Weight loss is also associated with a decline in functional status. Weight loss of more than 5% in community-dwelling women 60–74 years old was associated with a twofold increase in risk of disability over time, compared with women who did not lose weight, after adjustments for age, smoking, education, study duration and health conditions.8 Weight loss and undernutrition are also related to functional decline in nursing home residents.9
Body weight and weight adjusted for height (BMI) are easily obtained clinical measurements that can predict adverse outcomes in older persons.
The Relationship of Weight Loss to Mortality
A body mass index of less than 22 kg m−2 has been associated with a higher one-year mortality rate and with poorer functional status among older community-dwelling persons.10 The risk for higher mortality in men older than 65 years begins at a BMI of less than 22 kg m−2 and increases to a 20% higher risk in men older than 75 years with a BMI of less than 20.5 kg m−2. Similarly, a higher mortality risk in women begins at a BMI of less than 22 kg m−2 in women older than 65 years and increases to a 40% higher risk in women older than 75 years with a BMI of less than 18.5 kg m−2.11 BMI less than the 15th percentile is an independent predictor of 180 day mortality following hospitalization.12
Although there is a strong association between BMI and mortality, the key factor in mortality risk appears to be recent weight loss. Recent weight loss, rather than current BMI, is the strongest predictor for mortality. After excluding subjects with weight loss of 10% or more of their body weight, there is little relationship between BMI and mortality.13 In persons over 50 years of age who reported an unintended loss of 10 lb (∼3.7 kg) or more in the year before evaluation, the age-adjusted death rate was much higher compared with persons who voluntarily lost weight through diet or exercise or who maintained or gained weight.14 Nearly all of the observational studies on body weight have found that any weight loss is associated with increased, rather than decreased, risk for death.
The data suggest that obesity in older adults may not be an important clinical target for reducing mortality and that a preferred public health emphasis for this age group would be to increase awareness that substantial weight loss after age 50 years is a potential indicator for poor prognosis.
Body weight in the general population is not stable. Some 29% of men and 44% of women in the USA report that they are attempting to lose weight, and 35% of men and 34% of women report that they are attempting to maintain weight. The most common strategy among those attempting to lose weight was to consume less fat, but not fewer calories (35% of men and 40% of women). Only 22% of men and 19% of women reported using a combination of eating fewer calories and engaging in at least 150 min of leisure-time physical activity per week.15
In an observational study, overweight and obese persons who were at least 35 years of age and who had a BMI greater than 25 kg m−2, self-reported their intention to lose weight and then reported actual weight change during the past year. Those persons reporting an intentional weight loss had a 24% lower mortality rate compared with persons not trying to lose weight and reporting no weight change. However, mortality rates were independent of actual weight change. The persons who reported trying to lose weight but who had no weight change also experienced a 20% reduction in mortality risk. An unexpected finding was that a decreased mortality rate was also found among those who reported gaining weight but who were not trying to lose weight. In this study, an attempt at weight loss was associated with lower all-cause mortality, but was independent of weight change. A higher mortality rate (31%) occurred only in those persons reporting unintentional weight loss.
Paradoxically, a higher two-year mortality was found in community-living subjects who lost weight by dieting (36%) compared with those who had involuntary weight loss (28%). These data suggest that even voluntary weight loss by dieting may place older persons at risk. The recommendation that older adults voluntarily reduce body weight cannot be supported by the literature and may be hazardous.
Effect of Weight Loss on Comorbid Conditions
Only limited data support the notion that intentional weight loss reduces total mortality. However, mortality is only a small part of the substantial burden of disease caused by obesity-related conditions such as hypertension, diabetes mellitus, coronary artery disease, degenerative arthritis and cancers of the breast, uterus and colon. Short-term reductions in caloric intake (dieting) have favourable effects on blood pressure, cholesterol and metabolic rate. These benefits require at least a 20% reduction in caloric intake.
Weight loss has been shown to reduce disease-specific risks such as hypertension and type 2 diabetes. However, it should be noted that overweight/obesity-related comorbidities, particularly those associated with the insulin resistance syndrome (e.g. hypertension, dyslipidaemias and hyperinsulinaemia) can be improved independently of weight loss.16, 17 Blood pressure can be lowered in the absence of weight loss by dietary changes.18 The effect on blood pressure by non-pharmacological interventions can be maintained for 3–5 years despite significant increases in body weight.19 Other trials of coronary artery disease have shown prevention effects to be independent of weight loss. The data suggest that improvements in comorbid conditions can be enhanced with lifestyle changes, but that the effect is independent of whether weight loss occurs.
Causes of Weight Loss
The regulation of body composition is dynamic over time. Minute-to-minute composition is regulated by a person’s metabolic state. Day-to-day regulation depends of insulin and glucagon. Month-to-month, hormones such as estrogens and androgens, growth hormone, prolactin, thyroid hormones, catecholamines and corticosteroids regulate body composition. Immune mediators, such as interleukin-1, tumour necrosis factor and interleukin-2, also can affect body composition through modulation of appetite and food intake and direct effects on skeletal muscle.20
Weight loss can be either voluntary (a conscious decision to reduce body weight by either restricting calories or increasing energy expenditure) or involuntary (absence of any intention to reduce weight). Involuntary weight loss can occur from a variety of causes, including ingestion of inadequate calories (starvation), disuse atrophy or hormonal deficiencies (sarcopenia), a decrease in appetite (anorexia) or the effects of disease (cachexia), and a combination of these factors21 (Table 17.1).
Table 17.1 Causes of weight loss.
| Type | Mechanism | Cause |
| Intentional | Decreased caloric intake | Voluntary restriction |
| Increased energy expenditure | Exercise | |
| Unintended | Anorexia | Impaired appetite |
| Starvation | Inadequate access to food | |
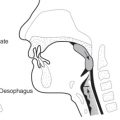
| Inability to swallow food | ||
| Inability to absorb food | ||
| Cachexia | Cytokine-mediated disease | |
| Sarcopenia | Age-related loss of muscle mass |
Starvation
Simple starvation is caused by pure protein–energy deficiency. Starvation can be short-term (fasting) or long-term (chronic protein–energy undernutrition). Worldwide, starvation is most often caused by lack of food. In developed countries, starvation is usually associated with disease. Starvation occurring in the presence of adequate food results from inability to swallow, a non-functioning gastrointestinal tract or failure of appetite (anorexia).
Older persons ingest fewer calories than younger adults. On average, persons over the age of 70 years consume one-third less calories compared with younger persons.22 About 16–18% of community-dwelling elderly persons consume less than 1000 kcal daily.23 This reduction in intake places older adults at risk for protein–energy, vitamin and mineral undernutrition.
The decline in energy intakes that accompanies ageing has been the subject of intensive investigation. Total energy expenditure (TEE) declines with ageing, chiefly due to changes in resting energy expenditure (REE). REE decreases by 10–20% with age, primarily due to a decrease in muscle mass.24, 25 REE is higher in active older adults than sedentary older adults,26 but a decline in muscle mass occurs in both sedentary and active ageing adults.27 A decrease in physical activity largely explains the decline in TEE with age.28 Surprisingly, there is little correlation between physical activity and fat mass in older persons. Higher physical activity is not associated with a lower body fat mass in subjects older than 60 years.
Sarcopenia
Unintended weight loss in older persons may result from a decrease in fat-free mass. Sarcopenia is operationally defined as an appendicular skeletal muscle mass divided by height in metres of more than two standard deviations below the young normal mean. Using this definition, Baumgartner et al. found that 14, 20, 27 and 53% of men aged less than 70, 70–74, 75–80 and over 80 years, respectively, met this definition. In women, 25, 33, 36 and 43% in the same age groups had sarcopenia.29 Although a decrease in muscle mass is the hallmark of sarcopenia, not all sarcopenic persons have a low body mass. At a BMI cut point of ∼27 kg m−2, 14% of men less than 70 years old and 29% of men more than 80 years old were sarcopenic and obese and 5% of women less than 70 years old and 8% of women more than 80 years old were sarcopenic and obese. Although the decline in muscle mass should be reflected in body weight, an increase in fat mass may obscure the body weight loss. Therefore, a relatively small proportion of sarcopenic persons do not exhibit a decrease in body weight.
The fact that muscle mass decreases with age has been known for some time. Earlier work demonstrated that the excretion of urinary creatinine, a measure of muscle creatine content and total muscle mass, decreases by nearly 50% between the ages of 20 and 90 years. This age-related loss of muscle mass appears to be fairly consistent, at a rate of ∼1–2% per year after the age of 50 years, and occurs in both sedentary and active ageing adults. In contrast, in healthy young adults, no net change occurs in skeletal muscle mass under equilibrium conditions due to the balance in skeletal muscle protein synthesis and degradation. This age-related reduction in muscle mass and strength is also accompanied by a reduction in motor unit number30 and by atrophy of muscle fibres, especially the type IIa fibres.31 An associated decline in protein synthesis, particularly in the synthesis of myosin heavy chains, has been observed.32
The loss of muscle mass with ageing is clinically important because it leads to diminished strength and exercise capacity.33 Dynamic, static and isokinetic muscle strength decreases with age.34 Maximum oxygen consumption declines with age35 at a rate of 3–8% per decade beginning at age 30 years. However, after correction for muscle mass, there is no important decline in VO2max with ageing, indicating that a change in muscle mass is the significant factor.36 Up to 65% of older men and women report that they cannot lift 10 lb (∼3.7 kg) using their arms.37 Although sarcopenia is due to a reduction in skeletal muscle mass, not all subjects demonstrate a loss in body weight. An increase in fat mass accompanying ageing may mask the loss of non-fat mass, resulting in normal or even an obese body weight in sarcopenic persons.
Cachexia
Cachexia is the cytokine-associated wasting of protein and energy stores due to the effects of disease. Systemic inflammation mediated through cell injury or activation of the immune system triggers an acute inflammatory response. Persons with cachexia lose roughly equal amounts of fat and fat-free mass while maintaining extracellular water and intracellular potassium. The loss of fat-free mass is mainly from the skeletal muscle.
Cytokines are related to a number of disease conditions, including cancer, end-stage renal disease, chronic pulmonary disease, congestive heart failure, rheumatoid arthritis and AIDS38 (Table 17.2). In subjects with pneumonia, the admission concentrations of α1-antitrypsin and α1-acid glycoprotein are better predictors of hospital morbidity than albumin and C-reactive protein levels.39 In subjects with end-stage renal disease on haemodialysis followed for 3 years, increased IL-1, TNF-α, IL-6 and IL-13 levels were significantly associated with increased relative mortality risk, whereas higher levels of IL-2, IL-4, IL-5, IL-12, T-cell number and function and CH50 were associated with improved survival.40 Although the cancer anorexia–cachexia syndrome is present in 50% of advanced cancer patients and in 80% of terminally ill cancer patients, serum levels of cytokines are not always directly associated with the onset of cancer anorexia–cachexia syndrome.41
Table 17.2 Conditions associated with cachexia.
| Infections, e.g. tuberculosis, AIDS |
| Cancer |
| Rheumatoid arthritis |
| Congestive cardiomyopathy |
| End-stage renal disease |
| Chronic obstructive pulmonary disease |
| Cystic fibrosis |
| Crohn’s disease |
| Alcoholic liver disease |
| Elderly persons without obvious cause |
Cytokines have a direct negative effect on muscle mass and increased concentrations of inflammatory markers have been associated with a reduced lean mass.42–44 This direct effect also has been associated with a decline in muscle strength in older adults.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree