Introduction
The use of dietary supplements in general and nutrient supplements in particular is prevalent and growing in the United States. In 2007, dietary supplement sales grew to $23.7 billion. Sales of multivitamins, the most commonly purchased of supplements, grew by 3.9% in 2007 to $4.5 billion in sales for the year.1, 2 The ageing of the population and consumer desire to maintain good health and prevent disease have contributed to the increased growth of this industry. However, the current evidence on the use of dietary supplements rests on epidemiological association only.
The specific requirements for micronutrients in the elderly have not been studied until fairly recently. Vitamin and mineral requirements do not remain static over the adult life span. There are several micronutrients for which there is strong evidence that requirements are in fact increased in the elderly compared with younger people, such as vitamins D, B6 and B12.3, 4 It is clear that individuals change physiologically during ageing and that ageing is often associated with the development of chronic degenerative diseases. The roles that various supplements play in these changes appear to be less defined. There is an overall lack of evidence on the nutritional needs of the elderly, with a particular lack of data from clinical trials. Additionally, there is a critical need for the development of valid and reliable methods to detect undernutrition and for the generation of data to determine the dietary reference intakes (DRIs) of individuals 51–70 and >70 years old.5
Nutrition is an important determinant of health. As people age, activity levels and energy requirements tend to decrease. Concomitant decreases in food consumption may cause protein and micronutrient intake to fall below desirable levels. It is well documented that many older persons develop physiological anorexia associated with ageing. Additional factors that increase the risk of undernutrition include physiological changes that affect digestion, absorption and metabolism of nutrients, social isolation, chronic diseases, oral problems, sensory impairment, cognitive impairment, depression, multiple and chronic medication use, poverty and inappropriate food intake.6–9
Vitamin disorders in the elderly usually present atypically or are masked by coexisting diseases or a general failure to thrive.10 Vitamin preparations are consumed on a daily basis by 20–60% of elderly people. These supplements are consumed for various reasons, including the following: to increase energy, improve health, improve appetite and prevent and treat diseases. Older persons may consume potentially toxic amounts of vitamins and minerals by supplementation.11, 12 Drug–nutrient interactions are common in the elderly because of the high incidence of polypharmacy, many of which may occur unrecognized.13 Table 19.1 summarizes drugs with potential for interaction with various vitamins and minerals.
Table 19.1 Potential micronutrient–drug interactions.10, 14.
| Micronutrient | Drug |
| Calcium | Vitamin D, lysine |
| Chromium | Vitamin C |
| Copper | Zinc, iron |
| Folic acid | Methotrexate, cotrimazole, phenytoin, sulfasalazine, triamterene, zinc, alcohol |
| Magnesium | Vitamin B6, calcium |
| Manganese | Calcium, iron, zinc, copper |
| Selenium | Vitamin E |
| Vitamin A | Iron, vitamin E, tetracycline, cholestyramine |
| Vitamin B1 (thiamine) | Vitamin B2, vitamin B3 |
| Vitamin B2 (riboflavin) | Ouabain, theophylline, penicillin, boric acid, probenecid, chlorpromazine, phenothiazines, barbiturates, streptomycin, oral contraceptives, antidepressants, probenecid, tobacco, alcohol |
| Vitamin B3 (niacin) | Vitamin B1, vitamin B2, anticonvulsants, aspirin, clonidine, hydroxymethylglutaryl (HMG)-coenzyme A reductase inhibitors |
| Vitamin B6 (pyridoxine) | Magnesium, anticonvulsants |
| Vitamin C | Copper, iron |
| Vitamin D | Aluminium hydroxide, corticosteroids, diuretics, rifampin, phenytoin |
| Vitamin E | Antacids, cholestyramine, colestipol, mineral oil, sucralfate, iron, vitamin A, tobacco, alcohol, coumarins, anticoagulants, indandiones |
| Vitamin K | Calcium, anticoagulants |
| Zinc | Diuretics, copper, N-acetylcysteine, iron, calcium, magnesium |
Prevalence/Scope of the Problem
There continues to be a lack of evidence on prevalence of vitamin and mineral deficiencies, most studies have concentrated on protein energy malnutrition.15 The prevalence of vitamin deficiency in usual western diets is higher than generally believed, especially in the elderly.16 Various studies have revealed that up to 20% of community-dwelling ambulatory adults, 37% of home-bound elderly, 30–60% of hospitalized patients and 17–85% of institutionalized patients are malnourished.17–22
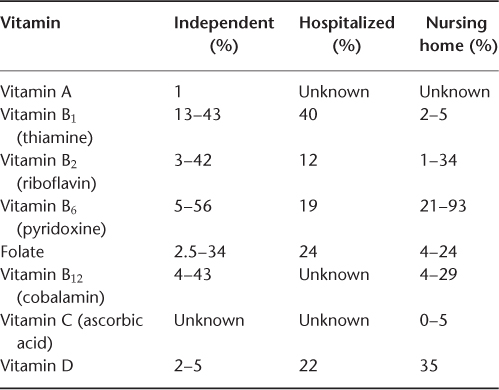
According to the National Health and Nutrition Examination Survey (NHANES), up to 16% of Americans over the age of 65 years consume less than 1000 calories per day. The reduced caloric intake is incompatible with maintaining adequate vitamin and mineral intakes. Studies on vitamin deficiencies in older individuals have revealed that vitamin deficiencies vary from 2.6 to 6.8% for vitamin D in the general population to 35% in the institutionalized patients, while vitamin A deficiency is seen in 1% or less of the older adults. The prevalence for vitamin B deficiency shows marked heterogeneity. The prevalence for vitamin B1 varies from <5% in the nursing home patients to as high as 43% in independent older persons; vitamin B12 deficiency is seen in up to 43% of independent older adults and in up to 29% of nursing home patients.15, 23–26 Table 19.2 gives the prevalence of vitamin deficiencies. Information on prevalence of trace mineral deficiencies comes from the developing world; zinc deficiency is widely recognized to be a common association with malnutrition. Geographic surveys show trends for selenium deficiency in individuals living in areas with low soil content of selenium.27, 28
Table 19.2 Prevalence of vitamin deficiencies in the elderly.
Dietary Reference Intakes
The goal of the Recommended Dietary Allowances (RDAs) was to estimate nutritional requirements for preventing basic deficiency diseases. The recommendations were also meant to be applied as general guidelines for groups, not as a gold standard for individuals. Research, led by the American Heart Association in the 1960s, demonstrated the links between diet and disease. It was already known that deficiency in certain nutrients results in disease. Studies went on to show clearly that increased intake of certain nutrients actually helps to prevent some chronic illnesses. Because of this research and because the RDAs were being used for purposes other than those for which they were created, new recommendations were in order.
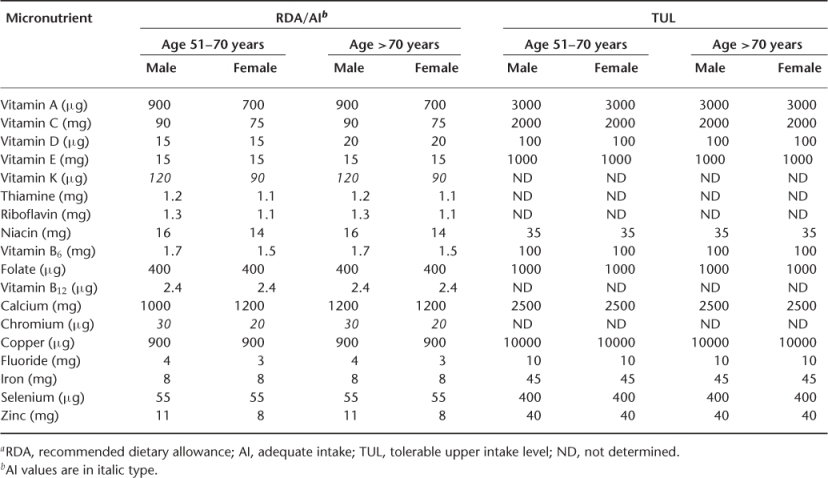
The new guidelines are called Dietary Reference Intakes or DRIs. They were developed by the Food and Nutrition Board of the Institute of Medicine, National Academy of Sciences, and published in 1998. These were designed to reflect the latest understanding of nutrient requirements based on optimizing health in individuals. For the first time, the group included data for individuals 70 years and older. They are being developed with individuals in mind. They are also concerned about the prevention of chronic degenerative diseases, such as macular degeneration, heart disease and osteoporosis. The DRIs are based on several factors. These include the level of a nutrient needed to meet the needs of a healthy individual and the level at which a nutrient will produce harmful side effects. The DRIs also consider the source of the nutrient, for example, the body is often better able to use nutrients supplied in food than by supplements. The new DRIs also take age and gender into consideration.15, 29–31
The Board described four categories of reference values:
Table 19.3 gives the DRIs for vitamins and minerals for individuals aged 51–70 and over 70 years.
Table 19.3 Dietary reference intake for micronutrients (Food and Nutrition Board, Institute of Medicine, National Academy of Sciences, 2010)a.
Factors Affecting Nutrient Intake in the Elderly
Total energy intake decreases substantially with age; this results in concomitant declines in most nutrient intakes, including vitamins and minerals. Despite the common occurrence of protein-energy undernutrition in older persons, its presence is rarely recognized. Factors implicated in the decreased nutrient intake in the elderly can be divided into the following categories:32, 33
- social
- psychological
- medical
- age-related.
Factors affecting the nutrient intake are summarized in Table 19.4.
Table 19.4 Factors affecting nutrient intake in the elderly.
| Social |
1. Poverty 2. Social isolation 3. Ignorance 4. Problems with meal preparation 5. Inability to shop 6. Lack of recognition of ethnic or other food preferences in institutional settings 7. Monotony of institutionalized food |
| Psychological |
1. Depression 2. Bereavement 3. Alcoholism 4. Dementia 5. Late-life paranoia 6. Late-life mania 7. Anorexia Tardive 8. Sociopathy 9. Overwhelming burden of life |
| Medical |
1. Increased metabolism
2. Anorexia
3. Swallowing problems
4. Malabsorption
5. Feeding problems
|
| Age related |
1. Anorexia of ageing 2. Decreased olfaction 3. Decreased taste |
The Antioxidants
One of the leading theories proposed for cellular and organism ageing is that damage to cellular mechanisms and tissues occurs because of chronic damage resulting from oxidative stress caused by oxygen free radicals. Endogenous oxidative damage to proteins, lipids and DNA is thought to be an important aetiological factor in ageing and development of chronic diseases such as cancer, atherosclerosis and cataract formation. The developing recognition that many disease states are caused by oxidative damage and that certain antioxidant compounds may scavenge these damaging oxygen free radicals has resulted in increased interest in vitamins and minerals as antioxidants. Vitamins A, C and E and β-carotene, referred to as antioxidant vitamins, have been suggested to limit oxidative damage in humans. Riboflavin (vitamin B2) and selenium, a trace metal, are also suggested to have antioxidant capabilities.10, 32, 34–36
A large body of epidemiological evidence suggests that eating a diet rich in sources of vitamins has a protective effect on development of disease. The strong association of dietary intake of vitamins and disease in epidemiological studies has not been borne out in clinical trials).10 Caution must be exercised in interpreting the results of observational studies, as the association of diets rich in fruits and vegetables with reduced risk of cancer and cardiovascular disease may be due to the vitamins themselves, other compounds in fruits and vegetables or the substitution of dietary meat and fat with fruits and vegetables.37
Vitamin A and β-Carotene
Vitamin A consists of preformed vitamin A (retinol) and the carotenoids such as β-carotene. The carotenoids are a diverse group of more than 600 naturally occurring pigments. Natural sources include yellow, orange and red plant compounds, such as carrots and green leafy vegetables. Humans cannot synthesize carotenoids and depend on dietary intake exclusively for these micronutrients. β-Carotene can act as an antioxidant by quenching the unpaired electrons of free radicals and divert free-radical damage towards itself. Vitamin A refers to preformed retinol and the carotenoids that are converted to retinol. Preformed vitamin A is found only in animal products, including organ meats, fish, egg yolks and fortified milk. More than 1500 synthetic retinoids, analogues of vitamin A, have been developed. Vitamin A intake decreases with age; however, hypovitaminosis A is uncommon even in the very old. The current RDI for vitamin A is 1500 μg l−1(5000 IU). Except at the extreme ranges, retinol levels correlate poorly with vitamin A status and are affected by many non-nutritional diseases. Hepatic levels of vitamin A appear unchanged in adults. About 50–85% of the total body retinol is stored in the liver. It is also found in many other tissues in much lower concentrations.10, 32, 38, 39
Dietary proteins undergo proteolysis to release retinyl esters in the stomach. They then join lipids and bile salts to form micelles for absorption through the intestinal mucosa. Preformed vitamin A is absorbed by the intestinal cell by a carrier-mediated mechanism, however; carotenoids are passively absorbed by the intestinal epithelium. Vitamin A is then transported to the liver via the lymphatics. By means of a receptor-mediated endocytosis on the surface of the hepatocytes, the retinol esters are released and stored as retinyl ester. These are further metabolized to combine eventually with retinol binding proteins (RBP) before storage in vitamin A-containing lipid globules within the hepatic stellate cells. In order for vitamin A to reach its target organs, it binds to RBP molecules for release into plasma as a retinol–RBP complex.10, 38–40
Vitamin A has a number of biological actions. In the eye, it is required for prevention of xerophthalmia and phototransduction. Vitamin A is crucial to cellular differentiation and integrity.40, 41
Vitamin A deficiency is rarely seen in the United States and other industrialized countries. However, it is still the third most common nutritional deficiency in the world. In the elderly, diminished physical activity reduces intake and concentrations may drop, but there is little evidence to support the need for supplementation and, indeed, toxicity is manifested more readily with age.38, 40, 42–44 Deficiency can result in the following:
- night blindness, complete blindness and xerophthalmia;
- Bitot’s spots (areas of abnormal squamous cell proliferation and keratinization of the conjunctiva), which can be seen in young children;
- corneal perforation, keratomalacia and punctate keratopathy, which have been observed in early childhood development;
- non-specific dermatological problems, such as hyperkeratosis, phrynoderma (follicular hyperkeratosis) and the destruction of hair follicles and their replacement with mucous-secreting glands;
- impairment of the humoral and cell-mediated immune system via direct and indirect effects on the phagocytes and T cells.
In a majority of cases, vitamin A toxicity occurs because of the ingestion of large amounts of synthetic vitamin A, about 10 times higher than the RDI, or about 50 000 IU. In the elderly, diminished physical activity reduces intake and concentrations may drop, but there is little evidence to support the need for supplementation and, indeed, toxicity is manifested more readily with age. Hypervitaminosis can occur both acutely and after chronic ingestion. Symptoms of toxicity include dry skin, nausea, headache, fatigue, irritability, ataxia, alopecia, hyperlipidaemia, hepatotoxicity, bone and muscle pain and visual impairments.10, 40, 41, 45
Epidemiological studies of dietary vitamin A on possible cancer chemoprevention appear to represent primarily the effect of α-carotene. Studies of relationships between cancer and vitamin A and carotenoids have provided mixed results. Observational data and clinical trial data have not been consistent.
Two large, randomized, placebo-controlled trials assessed the risk of lung cancer among male smokers or asbestos workers receiving α-carotene supplements. The risk of lung cancer was significantly increased among men receiving supplements. In the α-Tocopherol, α-Carotene (ATBC) Cancer Prevention Study, there was an increase in both prostate cancer incidence and mortality among subjects randomized to α-carotene. The excess risk appears to resolve over time once supplements are stopped.46–48
There have been no clinical trials of vitamin A intake and breast cancer. However, observational studies of vitamin A intake and breast cancer have yielded varying results. In a study by Kushi et al., no association between dietary vitamin A and breast cancer was observed.49 In contrast, recent data from the Nurses’ Health Study suggest that premenopausal women, particularly those with a positive family history, have significant reductions in breast cancer risk with increasing dietary α-carotene and β-carotene, lutein/zeaxanthin and total vitamin A.50, 51 Data from the Polyp Prevention Study Group did not show a reduction in adenoma risk in patients randomized to receive either α-carotene, vitamin C and E or both α-carotene and vitamins C and E.52
Vitamin A and α-carotene supplements have shown no benefit for primary or secondary prevention of coronary heart disease (CHD) in randomized trials and have been associated with potential harm.53 There is consistent evidence from observational studies that vitamin A intake within the range taken by many people in western societies, is a risk factor for osteopenia and fractures. The Physicians Health Study found that 12 years of α-carotene supplements had no effect overall on the risk of cataract formation, but appeared to decrease the risk significantly among current smokers.54–57
On the basis of current clinical data and the lack of clinical efficacy with respect to cancer prevention, along with its possible adverse effects, vitamin A and α-carotene supplement use should be discouraged.
Vitamin E
Vitamin E occurs in eight natural forms as tocopherols (α, β, γ and δ) and tocotrienols (α, β, γ and δ), all of which possess potent antioxidant properties. Vitamin E was originally found to affect reproduction in rats and was given the name tocopherol, derived from the Greek words toc (child) and phero (to bring forth) to describe its role as an essential dietary substance in normal fetal and childhood development.58, 59
Vitamin E absorption depends on the breakdown of fatty acids and their uptake via enterocytes to the enterohepatic circulation. The synthesis of chylomicrons is required for transport of vitamin E via the lymphatic system to the liver. Within hepatocytes, chylomicron remnants are broken down by lysosomes and R, R, R-α-tocopherol is preferentially secreted into the bloodstream, packaged within very low density lipoprotein (VLDL) molecules. The transport protein for α-tocopherol is named α-tocopherol transfer protein (α-TTP).60–62
Vitamin E works as a free-radical scavenger and antioxidant. α-Tocopherol is the biologically active form of vitamin E. It protects polyunsaturated fatty acids (PUFAs), a major structural component of the cell membranes, from peroxidation. Primary sources of vitamin E are vegetable oil, wheat germ, leafy vegetables, egg yolk, margarine and legumes.63, 64 Vitamin E deficiency can be measured by examining serum or tissue α-tocopherol levels.65
Deficiency of vitamin E is uncommon in humans except in unusual circumstances. In the elderly, conditions resulting in fat malabsorption can cause vitamin E deficiency. The effects of deficiency are widespread throughout the body and include the following:40, 66, 67
- Neuronal degeneration resulting in spinocerebellar ataxia, decreased deep tendon reflexes or areflexia, peripheral neuropathy and posterior column destruction with impairment of proprioception and vibratory sense. This can result in gait disturbance, which is a basic manifestation of vitamin E deficiency.
- Degenerative myopathy.
- Ocular impairment such as retinopathy and extraocular muscle paresis.
- Brown bowel syndrome, a result of lipofuscin deposition and oxidative damage.
- Red blood cell life span reduction.
The effects of long-term supplementation of vitamin E are unclear. Some studies caution against the use of vitamin E in patients with an increased propensity to bleeding or those taking oral anticoagulants. Impaired absorption of fat-soluble vitamins A and K with large vitamin E supplements have been seen in animal models. Necrotizing enterocolitis is seen in infants supplemented with high doses of vitamin E. It may impair the haematological response to iron in children with iron-deficiency anaemia.40, 68, 69
The protective role of vitamin E against cancers seen in observational studies49, 51, 70, 71 has not been supported by randomized trials. The ATBC Cancer Prevention Study observed a 32% decrease in prostate cancer incidence and a 41% decrease in prostate cancer mortality among men receiving α-tocopherol compared with placebo.72 A second report from the ATBC study showed a significant 19% reduction in lung cancer risk associated with higher serum vitamin E levels. The reduction in risk was greatest among men younger than 60 years and among patients with fewer years of cumulative smoking exposure.73 The SELECT trial followed 35 533 relatively healthy men for a median of 5.5 years. Vitamin E supplementation did not prevent prostate cancer in this population.74 The Physicians’ Health Study II did not reveal any benefit of vitamin E supplementation on the incidence of prostate cancer.75 The HOPE-TOO trial and the Women’s Antioxidant Cardiovascular Study found no effect of vitamin E supplementation on cancer incidence or cancer deaths.76a, 77
Vitamin E supplementation has shown no benefit in both primary and secondary prevention of CHD.53 In the ATBC study, daily supplementation with vitamin E had no overall effect on stroke risk. However, a subgroup analysis suggested that vitamin E may increase the risk for subarachnoid haemorrhage and decrease the risk for ischemic stroke, particularly in men with hypertension.78 In the Heart Outcomes Prevention Evaluation (HOPE) trial, daily supplementation with vitamin E had no effect on progression of carotid intimal medial thickness.76b The HOPE-TOO trial (ongoing outcomes) showed that vitamin E at 400 IU was associated with an increase in heart failure.76a The Health Professionals Follow-up Study showed no association between supplemental vitamin E and stroke risk.79
Data from observational studies have suggested that increased dietary intake of vitamin E may have a protective effect against the development of Alzheimer’s disease. A longitudinal cohort study found that both vitamin E and C supplementation protected against the development of vascular dementia and improved cognitive function late in life.80–82 A randomized trial of selegiline, vitamin E, both or placebo among patients with Alzheimer’s disease showed that both selegiline and vitamin E were independently associated with significant reductions in several outcomes, including functional decline.83 A randomized trial of vitamin E supplementation in healthy older women did not reveal any cognitive benefit.84
There have been several studies reporting that vitamin E supplementation improves the immune response. However, randomized, placebo-controlled studies have found no reduction in the incidence of respiratory infections in institutionalized or non-institutionalized elderly patients receiving daily vitamin E supplements.85–89
A meta-analysis of vitamin E supplementation that did not stratify trials by dose of vitamin E found no significant effect of supplementation on all-cause mortality.53 However, a recent meta-analysis that examined the dose–response relationship between vitamin E and overall mortality in a total of 19 randomized clinical trials found that vitamin E supplementation with a dose of ≥400 IU per day was associated with a significantly increased risk of all-cause mortality.90
Current evidence for vitamin E supplementation is inconclusive. Data at present suggest that high-dose vitamin E (≥400 IU per day) increases all-cause mortality. Also, individuals taking anticoagulants should be particularly advised against high doses of vitamin E because of the synergistic action of vitamin E with these drugs.
Selenium
Selenium, a trace element, is a component of several enzymes, including glutathione peroxidase and superoxide dismutase. Both of these enzymes are important in the prevention of oxidative and free-radical damage to various cell structures. Evidence suggests that the antioxidant protection conveyed by Se operates in conjunction with vitamin E because deficiency of one seems to enhance damage induced by a deficiency of the other.91 Se is incorporated as selenocysteine at the active sites of multiple selenoproteins. Selenoproteins are also important for thyroid function, muscle metabolism and sperm function, and also immune function.92
Dietary sources include vegetables, grains, Brazil nuts, seafoods and organ meats. The amount of Se in plant food is determined by the amount present in the soil. The mechanism of absorption of Se from the gut is unknown. Dietary Se has a high bioavailability and its absorption from the gut is unregulated.93, 94
The risk of Se deficiency seems to increase in proportion to age. Also, low levels have been documented in type II diabetes.92, 95 In China, Keshan disease is seen in areas where the soil is poor in Se. It is an endemic cardiomyopathy which improves with Se supplementation. Se deficiency has been reported in individuals on chronic total parenteral nutrition (TPN).96 Severe deficiency of Se manifests as cardiomyopathy and myopathy.
Toxicity can result from excessive intake. The most common manifestations are hair and nail loss. Other manifestations include nausea, emesis, tooth lesions, mental status changes and peripheral neuropathy.97, 98
The potential protective effect of Se status on the risk of developing cancer has been examined in animal and epidemiological studies. Low levels of dietary Se are associated with a greater risk of prostate, oesophageal, colon and antral gastric cancers.93, 99–101 There have been studies evaluating the effect of Se on cancer-related chemotherapy. A study assessing the in vitro effects of Se on chemotherapy revealed that the addition of Se enhanced drug-mediated cancer cell death. In another study, the addition of dietary Se at the beginning of chemotherapy prevented the development of resistance to cisplatin.102, 103
The antioxidant properties of Se have been linked to a lower incidence of cardiovascular disease in humans. However, the therapeutic benefit of Se administration in the prevention and treatment of cardiovascular diseases still remains controversial.104, 105
Se deficiency has been associated with impaired cell-mediated immunity and enhanced activity of natural killer cells.106, 107 Studies on the coxsackievirus and influenza virus by Beck and co-workers108, 109 have shown that Se prevented the genomic conversion of a non-virulent strain into a virulent strain that occurred in the presence of Se deficiency in mice. These effects of Se may have considerable implications on the elderly population, especially in the institutional setting.
Vitamin C
Vitamin C (ascorbic acid) is a water-soluble vitamin widely found in citrus fruits, raw leafy vegetables, strawberries, melons, tomatoes, broccoli and peppers. Humans cannot synthesize vitamin C and a deficiency results in scurvy. The amount present in food consumed, however, depends on the season of the year, the transportation time to the store, the shelf time before purchase, the form of storage and the method of cooking. Boiling can cause a 50–80% loss of vitamin C. Cooking with minimal water or microwaving food reduces losses.32, 67
Vitamin C is absorbed in the distal small intestine through an energy-dependent process. Blood concentrations of ascorbic acid are regulated by renal excretion. The greatest concentrations of ascorbic acid are found in the pituitary, adrenal, brain, leukocytes and the eye. Its absorption does not seem to be affected by age. The bioavailability of vitamin C is inversely related to the amount ingested and also the form. Sustained release tablets allow higher absorption than standard pills. It is a reversible biological reductant and provides reducing equivalents for a number of biochemical reactions involving iron and copper. It therefore functions as a cofactor, enzyme complement, cosubstrate or a strong antioxidant in a variety of reactions and metabolic processes.10, 110–113
Vitamin C has multiple functions. It is an antioxidant and reduces harmful free radicals. It is purported to be an immune enhancer and is known to be crucial to collagen synthesis and to norepinephrine synthesis. The conversion of iron from the ferric (+3) to the ferrous (+2) form requires vitamin C. Without this conversion, methaemoglobin could not be converted to haemoglobin and iron could not be absorbed in the duodenum. Vitamin C is also involved in the reduction of nitrates, a function that possibly is involved in stomach cancer. Vitamin C has a role in prostaglandin and prostacyclin metabolism. It may be capable of attenuating the inflammatory response or even sepsis syndrome.67, 114–116
Vitamin C deficiency is common in many frail elderly populations. Because vitamin C is supplied only by diet, deficiency is caused by insufficient dietary intake.10, 117–119 Deficiency primarily affects the musculoskeletal and haematopoietic systems. Deficiency results in the following:67
- Reduced collagen cross-linking and therefore decreased collagen tensile strength, leading to impaired wound healing and to weakened blood vessels.
- Haemostasis abnormalities occur, producing painful subperiosteal haemorrhages, haemarthrosis, haemorrhagic perifolliculitis, gingival bleeding, ecchymoses, petechiae and nail bed splinter haemorrhages. Some of these manifestations are common in elderly persons and are usually attributed to age-related physiological changes and not to vitamin deficiency.
- Structurally abnormal collagen that produces structurally abnormal osteoid, which produces structurally abnormal bone.
- Scurvy, which is the clinical syndrome produced by deficiency and develops after intake of less than 10 mg per day for 3–6 months. Scurvy includes the previously mentioned physical findings plus the development of corkscrew hairs, glossitis, gingival hyperplasia and bleeding and poor dentition caused by periodontitis and loss of teeth. Iron-deficiency anaemia can also occur. Terminal features include icteris, oedema, hypotension and convulsions.
There have been some reports of excessive use of vitamin C as a risk factor for calcium oxalate nephrolithiasis. However, a prospective epidemiological study demonstrated that consumption of high doses of vitamin C lowered the relative risk of calcium oxalate stones compared with 250 mg or less of vitamin C per day. Ingestion of large quantities of vitamin C has been rarely associated with fatal cardiac arrhythmias in patients with iron overload, presumably due to oxidative injury. Vitamin C toxicity has been associated with diarrhoea and abdominal bloating. High doses are also associated with false negative guaiac tests and they also alter the results of glucose measurements.116, 120–122
A large, randomized trial of vitamin C for secondary prevention of CHD found no benefit of supplementation with vitamin C. The Health Professionals Follow-up Study showed no association between supplemental vitamin C and stroke risk. Prospective data from the Nurses’ Health Study showed a 45% reduction in the risk of cataract requiring extraction in women using vitamin C supplements for at least 10 years. In contrast, a randomized, placebo-controlled study of high-dose supplementation with vitamins C and E and β-carotene found no reduction in the 7 year risk of development or progression of age-related lens opacities with vitamin C supplementation.53, 79, 123, 124
Riboflavin
Riboflavin or vitamin B2 is an important component of the coenzymes flavin mononucleotide (FMN) and flavin adenine dinucleotide (FAD). It is involved in an array of biochemical reactions. It is important for oxidative phosphorylation, ATP production and the production of reduced glutathione, which is an antioxidant. Vitamin B2 has been implicated in a signal transduction role for programmed cell death and regulation of a number of other important intracellular pathways. Dietary sources include dairy products, green leafy vegetables, whole and enriched grains, meats, liver, poultry and fish. It is not destroyed by heat, oxidation or acid but is susceptible to ultraviolet light and alkalis.67, 125
Riboflavin is released by proteolysis from the ingested food and undergoes passive absorption from the intestinal lumen. It then enters the hepatic cells and undergoes conversion to FAD and FMN. Like other B vitamins in this class, stores are minimal and regulated replacement is necessary through food or supplements.
Vitamin B2 deficiency is regarded as the most common vitamin deficiency in the United States; it is usually seen in conjunction with other B vitamin deficiencies. There is some evidence that the requirements for riboflavin may increase with ageing and that the glutathione reductase activity declines with ageing. Plasma riboflavin concentrations tend to reflect recent dietary intake. Erythrocyte glutathione reductase assay is a better test for riboflavin deficiency; it is not valid, however, in individuals with glucose 6-phosphate dehydrogenase deficiency.15, 91, 125
Deficiency may be secondary to inadequate dietary intake or a result of chronic diarrhoea, alcoholism or liver disease. Deficiency may manifest as the following:67, 91, 125
- cheilosis
- magenta-coloured glossitis
- inflammation of the oral mucosa
- seborrheic dermatitis
- normocytic normochromic anaemia
- corneal revascularization.
Vitamin B2 supplementation helps only in the prevention of deficiency. A small randomized controlled trial has shown some benefit of supplementation with a very large dose in the prevention of migraine.67, 126
Vitamin D
Vitamin D, or calciferol, is a generic term and refers to a group of lipid-soluble compounds with a four-ringed cholesterol backbone. Vitamin D is not a true vitamin, because humans are able to synthesize it with adequate sunlight exposure. By photoconversion, 7-dehydrocholesterol becomes previtamin D3, which is metabolized in the liver to 25-hydroxyvitamin D3, the major circulating form of vitamin D. In the kidneys, this is converted to two metabolites, the more active one being 1,25-dihydroxyvitamin D3. It is derived primarily via synthesis in the skin. Dietary sources include fortified milk, milk products, oily fish, egg yolks and fortified foods.32, 40, 67
Vitamin D is absorbed in the form of micelles by the intestinal epithelium to form chylomicrons. Chylomicrons enter the liver via the portal circulation where vitamin D undergoes a hydroxylation process by 25-vitamin D hydroxylase to form 25-hydroxyvitamin D (calcidiol). Further hydroxylation of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D [1,25(OH)2-vitamin D or calcitriol] occurs in the mitochondria of the proximal tubules of the kidney. Vitamin D from any source and in either form is absorbed into the circulation and bound to vitamin D-binding protein. Calcitriol, the biologically active form, has a short half-life of 4–6 h and therefore does not accurately reflect body stores, whereas calcidiol has a longer half-life of 3 weeks. Hence calcidiol is more widely used to measure vitamin D status. Laboratory measurements reflect both vitamin D2 and vitamin D3 status. Deficiency is defined as a calcidiol level below 15 mg dl−1.40, 67, 127–129
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








