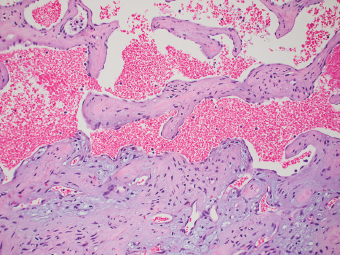
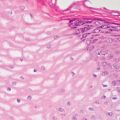
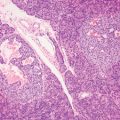
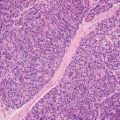
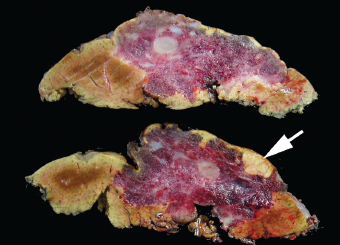
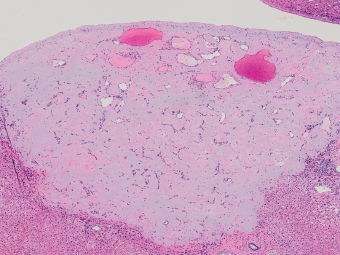
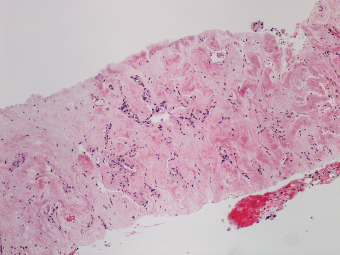
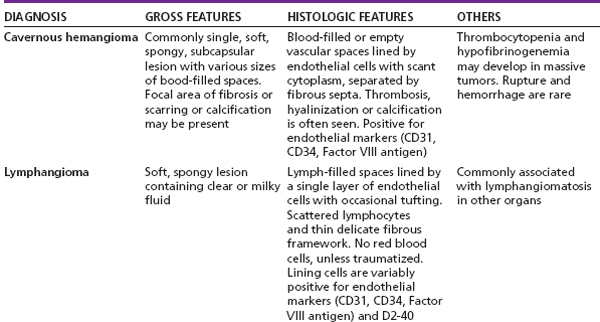
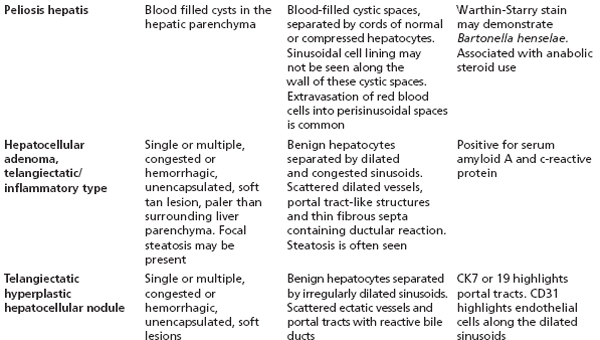
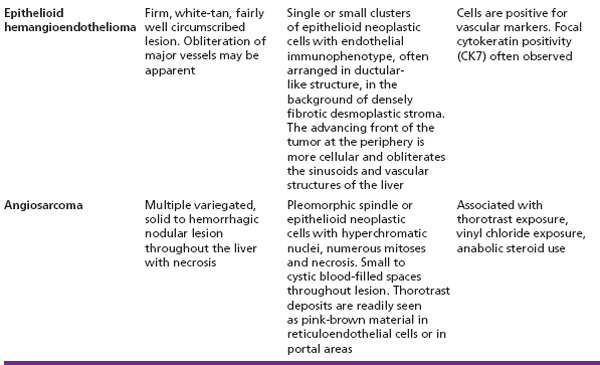
11 Biologic Evolution and Treatment Biologic Evolution and Treatment Hemangioma, often referred to as cavernous hemangioma, is a benign vascular lesion composed of communicating and dilated vascular spaces of variable size, lined by a single layer of flat, benign, endothelial cells. Cavernous hemangioma, hyalinized hemangioma, sclerosed or sclerosing hemangioma, solitary necrotic nodule, and various other synonyms have been used to describe different stages of development and regression of hemangioma. The term “sclerosed” is reserved for hemangiomas that are predominantly fibrotic with near complete obliteration of the vascular spaces. Cavernous hemangioma is the most common primary tumor of the liver (515). It is usually asymptomatic and an incidental finding at the time of surgery, metastatic disease workup, or autopsy. Patients with large cavernous hemangioma may experience abdominal pain, which may be the result of recurrent or intermittent intratumoral thromboses, infarction, stretching of the Glisson capsule or pressure to adjacent organs. Vascular hum can rarely be heard over the lesion. Hemangiomas may be single or multiple, well demarcated, ranging in size from a few millimeters to more than 20 cm in greatest diameter. Giant hemangioma refers to hemangioma larger than 15 cm. Hemangiomas are located either deep within the liver parenchyma or in the periphery of the liver, which often project or are visible from the surface. Pedunculated lesion is an infrequent finding (516). The diagnosis of hemangioma is based on imaging studies, in particular contrast-enhanced computed tomography (CT), which show immediate homogeneous filling of the lesion during arterial phase. Tumor is isodense to large blood vessels on CT, often with peripheral enhancement. Magnetic resonance imaging of hemangiomas usually shows a heterogeneous appearance due to thrombi and scarring of the lesion. Fine needle aspiration is unnecessary in most instances due to the risk of intraperitoneal hemorrhage, particularly in peripheral or subcapsular lesion. Hemangiomas are a round or wedge-shaped, sharply demarcated, blood-filled area with a spongy and cystic or honeycomb pattern (Figure 11.1). Firm, white-tan areas of thrombosis, scarring, and occasionally calcification suggest regression in large or older hemangiomas to an extent that the entire lesion is sclerosed, resulting in the so-called “sclerosed hemangioma.” The role of mast cells in the regression and the development of fibrosis of sclerosed hemangioma have been suggested by Makhlouf and Ishak (517). Microscopically, hemangiomas are composed of various sizes of cavernous vascular channels lined by flattened benign endothelial cells with scant cytoplasm. The nuclei are small, often hyperchromatic and without mitotic activity. Variable amounts of mature fibrous tissue separate the vascular channels; many are thin and delicate fibrous strands, while others are thick as the result of organized thrombi and scarring (Figures 11.2–11.4). Scattered lymphocytes are often seen in the fibrous framework. Fresh and organizing fibrin thrombi may be found in some vascular channels. FIGURE 11.1 Multiple tan-white areas represent areas of thrombosis and scarring in cavernous hemangioma. A focal nodular hyperplasia is sometimes associated with cavernous hemangioma (arrow). FIGURE 11.2 Cavernous hemangioma is composed of blood-filled cavernous spaces, lined by flat endothelial cells. The lower field represents the thrombosed part of the lesion. FIGURE 11.3 Remaining slit-like vascular channels can be found in sclerosed hemangioma. FIGURE 11.4 A needle biopsy of sclerosed hemangioma showing hypocellular, dense, collagenized stroma without dilated vascular channels. While most of smaller hemangiomas are well demarcated from the surrounding liver with their distinct fibrous interface, some may show entrapment of bile duct or foci of hepatic parenchyma. In large hemangiomas, dilated lesional vascular channels occasionally extend into the adjacent parenchyma as far as 2 cm, beyond the confines of the main tumor, which is referred to as “hemangioma-like vessels” (518). This finding is of little to no consequence, as none of the patients studied had recurrences of hemangioma or developed clinical complications following excision, and there was no evidence that these lesions represent a low-grade malignancy. Incidental focal nodular hyperplasia may be found in or adjacent to hemangioma (Figure 11.1), which underscores the vascular pathogenesis of focal nodular hyperplasia. This finding in a small needle biopsy may mimic concurrent cirrhosis. The clinical differential diagnosis of hemangioma is mainly metastatic tumor, because hemangiomas are usually found incidentally during evaluation for metastatic disease of other organs. In many cases, imaging studies are sufficient to differentiate hemangioma from solid metastatic tumor. The pathological differential diagnoses of hemangiomas include other benign or low-grade vascular lesions, such as peliosis hepatis, hereditary hemorrhagic telangiectasia, epithelioid hemangioendothelioma, well-differentiated angiosarcoma, telangiectatic or inflammatory hepatocellular adenoma, and telangiectatic hyperplastic nodule. See Table 11.1 for differential diagnoses of vascular neoplasm and neoplastic mimics. TABLE 11.1 Differential Diagnoses of Vascular Neoplasm and Neoplastic Mimics of the Liver
Vascular Neoplastic Mimics of the Liver
 TELANGIECTATIC HYPERPLASTIC HEPATOCELLULAR NODULE
TELANGIECTATIC HYPERPLASTIC HEPATOCELLULAR NODULE
HEMANGIOMA
 CLINICAL AND IMAGING FEATURES
CLINICAL AND IMAGING FEATURES
 PATHOLOGIC FEATURES
PATHOLOGIC FEATURES
 DIFFERENTIAL DIAGNOSES
DIFFERENTIAL DIAGNOSES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree