Vaccines in Theory and Practice
Learning Objectives
• Compare and contrast exotoxins, endotoxins, and enterotoxins
• Identify mucosal-associated lymphoid tissue (MALT) inductive and effector sites
• List the seven different types of vaccines
• Identify the five live attenuated viral vaccines
• Recognize the three live attenuated bacterial vaccines
• Compare and contrast the advantages and disadvantages of live attenuated vaccines
• List the advantages and disadvantages of inactivated vaccines
• Compare and contrast toxins and toxoids
• Identify the usefulness of a conjugate vaccine
• Recognize reassortment vaccines
• Compare and contrast the advantages and disadvantages of bacterial or fungal expression vectors
• Identify the two viral vectors used in recombinant vaccines
• Understand the method used to create plant vaccines
• Compare and contrast systemic and mucosal adjuvants
• Identify the mechanisms by which aluminum salts stimulate the immune system
• Compare and contrast Freund’s complete adjuvant (FCA) and Freund’s incomplete adjuvant (FIA)
• Identify the impediments to using FCA in humans
• Discuss the relationship between muramyl dipeptide and mycobacterial cell walls
• Compare and contrast monophosphoryl lipid (MPL) and muramyl dipeptide (MDP)
• Recognize the three different oligodeoxynucleotide (ODN) classes and their functions
• Relate the structural and biologic functions of liposomes
Key Terms
Adjuvant
Attenuation
Endotoxin
Enterotoxin
Exotoxin
Fimbriae
Freund’s adjuvant
Liposomes
Oligonucleotide
Pili
Squalene
Toxoids
Vaccine
Introduction
Vaccination began with Lady Mary Wortley Montagu, the wife of the English Ambassador to Turkey. In 1723, she popularized the Turkish practice of variolation, in which small amounts of dried smallpox were scratched into the skin of healthy people. In fact, the term variola comes from the Latin word varus, meaning “mark on the skin.” Variolation proved to be protective against smallpox infection. In 1796, Edward Jenner heard stories that dairymaids were immune to smallpox if they had previously been infected with cowpox. Jenner showed that infections with cowpox provided protection from smallpox and that cowpox could be transmitted from dairymaid to dairymaid as a deliberate protection mechanism. Using the Latin word vacca, meaning “cow,” Jenner coined the name for the new procedure vaccination.
Louis Pasteur recognized the value of Jenner’s work and believed that vaccines could prevent many infectious diseases. During his lifetime, Pasteur developed vaccines for chicken cholera, rabies, and anthrax by using weakened organisms. In the twentieth century, microbiologists came to understand the differences between innocuous and infectious microbes. Highly infectious bacteria were termed virulent organisms and infectivity was determined by the presence of virulence factors.
Virulence Factors
Virulence factors include molecules that allow bacterial attachment to mammalian cells such as bacterial pili and fimbriae; polysaccharide capsules that surround pneumococcus and Pseudomonas and prevent phagocytosis; and toxins produced or released from gram-positive and gram-negative bacteria, respectively.
Three types of toxins are produced by bacteria: (1) Exotoxins are proteins synthesized and secreted by gram-positive bacteria. Exotoxins destroy mammalian cells or disrupt cellular function. For example, diphtheria toxin inhibits ribosome function and protein translation in mammalian cells, which ultimately kills the cells. Tetanus toxin accelerates the production of neurotransmitters that promote muscle contraction in the face (lockjaw) or in the long muscles in the back (opistothenosis). (2) Endotoxins are lipopolysaccharide components of the gram-negative cell wall. They consist of a long antigenic polysaccharide and a lipid A fragment that interacts with mammalian cells and contributes to septic or endotoxic shock. Unlike exotoxins, endotoxins are only released on the death of the bacteria. (3) Enterotoxins are secreted molecules that cause food poisoning and diarrhea. Staphylococcal, cholera, and clostridia enterotoxins produce transient effects in humans. Escherichia coli O157:H7 produces a potent enterotoxin that causes severe diarrhea, dehydration, and death.
Types of Vaccines
Vaccines are administered by subcutaneous, intramuscular, or mucosal routes. Administration by the intramuscular or subcutaneous route stimulates systemic immunity in the spleen, lymph nodes, and peripheral blood. The vaccines interrupt person-to-person transmission and prevent the spread of infectious agents to the critical organs in the body. Mucosal vaccines stimulate local immune responses to microbes at the point of entry into the body. Moreover, antigen-stimulated lymphocytes from the initial site travel to other mucosal surfaces conferring immunity at multiple mucosal sites (see Chapter 1). Mucosal vaccines are advantageous because they prevent both infection and dissemination to critical organs and are easy to administer.
Route of Administration and Mucosal Immunity
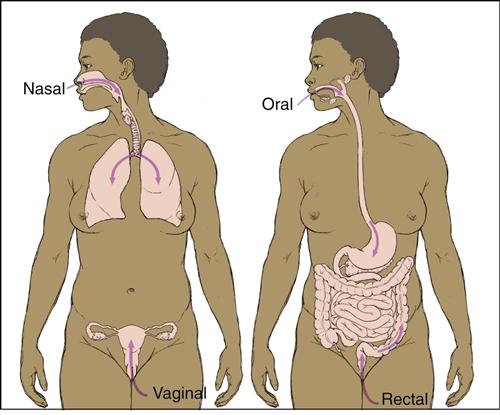
The route of administration determines which mucosal surface is stimulated by microbial agents. Oral administration induces antibody responses in the small intestine, ascending colon, and mammary and salivary glands. In contrast, nasal administration protects the upper airways and the lungs but has no effect on the lymphoid tissue in the gut (Figure 24-1).
Mucosal-Associated Lymphoid Tissue
Mucosal-associated lymphoid tissue (MALT) is a generic name for collections of lymphoid cells, small lymphoid nodes, and organs found in the gastrointestinal, urogenital, and respiratory tracts (see Chapter 1). MALT has both inductive and effector sites in the mucosa. Inductive sites include mucosal lymphoid nodules as well as M cells that transport foreign material to the lymphocytes in the submucosa. In the lymphoid nodes, T and B cells interact to produce immunoglobulin A (sIgA). Following antigen stimulation, T and B cells migrate to multiple effector sites throughout the submucosa. MALT is divided into segments on the basis of anatomic location: nasal-associated lymphoid tissue (NALT), bronchial-associated lymphoid tissue (BALT), and gut-associated lymphoid tissue (GALT).
Nasal-Associated Lymphoid Tissue
NALT is found in the salivary glands and the Waldeyer’s ring, including the palatine, tubal, pharyngeal, and lingual tonsils. Tonsillar anatomy is similar to that of lymph nodes in that it contains T and B cells in follicular germinal centers and mantle zones. B cells in tonsillar germinal centers produce a predominance of IgG antibodies rather than sIgA antibodies.
Bronchial-Associated Lymphoid Tissue
BALT comprises lymphocyte aggregations located randomly along the bronchial tree. More defined aggregations are found around the bifurcations of the bronchi and bronchioli. Both T and B cells are found in the aggregates. B cells are heavily skewed toward the production of sIgA.
Gut-Associated Lymphoid Tissue
Lymphocytes are scattered beneath the epithelium along the entire gastrointestinal tract. Organized lymphocyte clusters in Peyer’s patches contain CD4+ T helper cells, mature B cells, macrophages, and dendritic cells (see Chapter 1). GALT functions to protect mucous membranes from colonization and infections by pathogenic organisms.
Types of Vaccines
Live Attenuated Vaccines
Before a live organism can be used in a vaccine, it must undergo a process known as attenuation, which reduces virulence while maintaining immunogenicity. In the classic attenuation process, microbes are passed through unnatural hosts, grown on unusual media, or exposed to harsh chemicals for extended periods. As a consequence, microbes usually lose the critical genes necessary to produce virulence factors.
A new approach known as rationale attenuation inactivates or removes virulence genes by targeted mutation or gene deletion. Because of their small genome, viruses are relatively easy to attenuate. The Sabin polio, measles–mumps–rubella (MMR), chickenpox, herpes zoster, and hepatitis A vaccines contain live attenuated viruses. Bacteria, which have a larger genome, are more difficult to attenuate. Only three bacteria have been attenuated and used in vaccines. Live attenuated vaccines for typhoid fever and cholera are used in some parts of the world. Attenuated Mycobacterium bovis, known as Bacille Calmette-Guérin (BCG), is used as a vaccine in Europe and other countries. In veterinary medicine, a live attenuated Bacillus anthracis Sterne strain is used to vaccinate cows and horses against anthrax.
The use of live attenuated vaccines has advantages as well as disadvantages. A major advantage is that the body does not differentiate between an attenuated microbe and a wild-type microbe, and both elicit a vigorous, long-lasting immune response. Moreover, only one immunization is required for lasting protection.
However, attenuated viral and bacterial vaccines have some disadvantages. Viruses used in vaccines can mutate and revert to being virulent organisms. For example, it is estimated that 1 case per 2.5 million doses of the attenuated, oral Sabin vaccine results in vaccine-associated poliomyelitis. Live attenuated viruses are also shed by the respiratory route and pose a health risk to immunosuppressed individuals. Conversely, live attenuated bacterial vaccines often fail to stimulate MALT. For example, attenuated cholera bacteria fail to express a molecule necessary for M cell attachment and transport the bacteria to MALT located in the submucosa. Attenuated Salmonella bacteria are better immunogens, but three to four immunizations are necessary to stimulate MALT, and protection is achieved in only 66% of vaccinated individuals.
Unlike other live attenuated vaccines, the BCG vaccine is highly successful in preventing person-to-person transmission of tuberculosis and has few side effects. When children are vaccinated, the vaccine elicits a cell-mediated response that is highly protective in 80% to 90% of children. The BCG vaccine is used in countries that have a high incidence of tuberculosis, tuberculomeningitis, and blood-borne tuberculosis. More than one billion individuals have been vaccinated since 1921 with few side effects. The vaccine is not used in the United States because of the low incidence of tuberculosis and the vaccine’s interference with tuberculosis skin tests. Individuals vaccinated with BCG will have false-positive skin tests, and this often complicates or delays decisions concerning treatment.
Inactivated Vaccines
Inactivated vaccines consist of organisms killed by physical or chemical means. Killed bacteria are advantageous because they do not revert to the virulent state and pose little health risk to immunosuppressed subjects. However, they have several disadvantages. When administered intramuscularly, subcutaneously, or by both routes, inactivated vaccines are only weakly immunogenic and often require booster immunizations to achieve lasting protection. The Salk polio and some seasonal influenza vaccines contain inactivated viruses.
Subunit Vaccines
Whole-cell vaccines often contain nonantigenic molecules that can cause rare systemic and frequent local adverse health effects. Toxicity is reduced by eliminating all nonantigenic molecules while retaining the antigenic molecules or critical epitopes that are necessary for protection against infection. For example, the pertussis component of the diphtheria–pertussis–tetanus (DPT) vaccine comprises inactivated pertussis toxin, purified filamentous hemagglutinin, fimbriae, and pertactin. Subunit vaccines are advantageous because they do not cause infections and pose little risk to immunosuppressed individuals.
Toxoid Vaccines
Modified bacterial exotoxins known as toxoids
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree