| Stage/phase | Time after onset of penetration | Clinical findings: parasite | Clinical findings: host |
|---|---|---|---|
| Stage 1 Penetration | 30 min–7 h (average 3 h) | Penetration of the gravid flea; the abdominal segments 1–3 separate toward the cephalic direction | Penetration at an angle of 45–90º; slight erythema; mild stink; tiny reddish spot |
| Stage 2 Hypertrophy | 1–2 days | The abdominal segment enlarges and the parasite is visible | Itching and painful nodule with a central black dot; erythematous inflammatory area |
| Stage 3 White halo | 4 days | Correspond to the maximum growth of the parasite; the lesion resembles a white pearl with a central opening from which the enlarged flea eliminates feces and eggs | Painful foreign-body reaction |
| Stage 4 Involution | 3–4 weeks | Dark crust containing the parasite remains | The lesions may be numerous and close-set like a honeycomb; secondary infection is frequent |
| Stage 5 Residual scar | Days after the involution phase | Reorganization of the epidermis continued; the site occupied by the parasite is flattened and becomes indistinguishable from normal skin |
a Fortaleza Classification, based on: Eisele M, Heukelbach J, Marck EV, Mehlhorn H, Menckes O, Franck S, Feldmeier H. Investigations on the biology, epidemiology, pathology and control of Tunga penetrans in Brazil: I. Natural history of tungiasis in man. Parasitol Res. 2003;90:87–99.
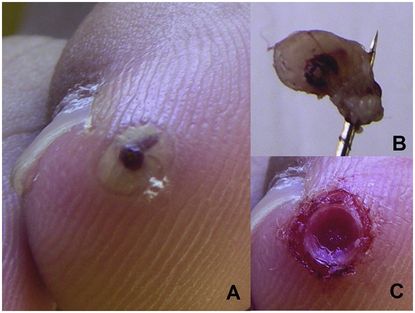
Figure 25.1 Tungiasis. (A) Isolated lesion on the first toe, corresponding to the parasite in its maximum growing stage, and presented as a white nodule with central opening. (B) Parasite removed with a needle, after gentle debridment, showing the intact abdomen full of eggs. (C) Circular ulceration, with clean walls, after removing the female Tunga.
Dermoscopy has been shown to be helpful in confirming the clinical diagnosis of Tunga infestation. The exam in vivo shows an annular brown ring with a central black pore. After extraction of the intact parasite, ex vivo, the diagnosis is confirmed by the visualization of the flea head on a distended “jelly sac” that corresponds to the abdomen full of eggs.
The histopathology of a typical lesion shows hyperkeratosis, parakeratosis, and acanthosis. The body of the flea locates in the upper dermis, and it is surrounded by a pseudocystic cavity. Inside the cavity, annular-shaped digestive and respiratory organs as well as ovaries rich in eggs may be observed. Eggs are oval or, less frequently, round, with a thickened wall and pale center. A perilesional, inflammatory infiltrate, mainly consisting of lymphocytes, neutrophils, and numerous eosinophils, is also present.
The differential diagnoses of tungiasis include talon noir, plantar or subungual warts, subungual exostoses, myiasis, abscesses, verrucae, ecthyma, tick bite, and melanocytic and nonmelanocytic skin tumors, especially melanoma.
Tungiasis is usually a self-limited condition, resolving in 4 to 6 weeks, with few complications consequent to the infestation. Colonial documents and travel reports from the early twentieth century indicate that the disease used to cause severe morbidity among the indigenous populations, such as grave inflammation in the feet, deep ulcers, gangrene, lymphangitis, and septicemia. Nowadays, the degree of morbidity depends on the intensity of infestation, hygiene conditions, and associated clinical disorders.
In economically depressed urban neighborhoods, however, poor housing conditions and inadequate health care lead to a high transmission potential, resulting in high parasite loads and secondary complications. The most common problems associated with tungiasis infestation are: acute painful inflammation and edema, abscess formation, lymphangitis, sepsis, tissue necrosis or gangrene, erysipelas, or even contamination by other infectious agents such as fungi, causing atrophy or loss of nails, toe deformations, and difficulty in walking and gripping. As an additional risk, clinical and epidemiologic evidence suggests that, in populations with low vaccination coverage, untreated tungiasis is a risk factor for tetanus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





