Fig. 9.1
Papillary adenoma: the tumor is lobulated, with slender papillae on the surface
Microscopic Features
According to histological morphology, gallbladder adenoma can be divided into tubular, papillary, and tubulopapillary types, while based on the cellular morphology, it can be divided into pyloric gland type, intestinal type, biliary type, and foveolar type (Fig. 9.2a–d). Each type has relatively specific immunohistochemistry markers, such as pyloric gland type (92% MUC6+), intestinal type (100% CK20+; 75% CDX2+; 50% MUC2+), biliary type (66% MUC1+), and foveolar type (100% MUC5AC+).
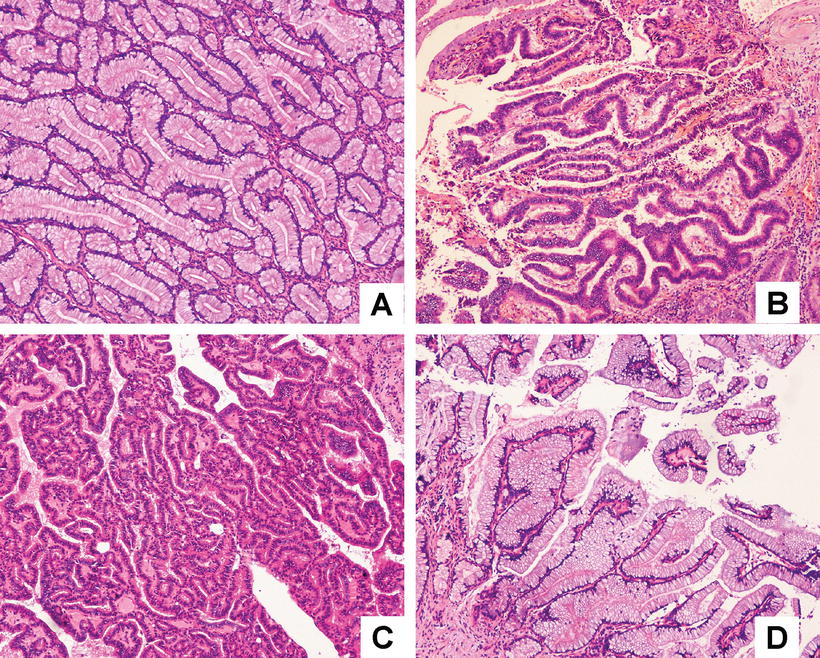
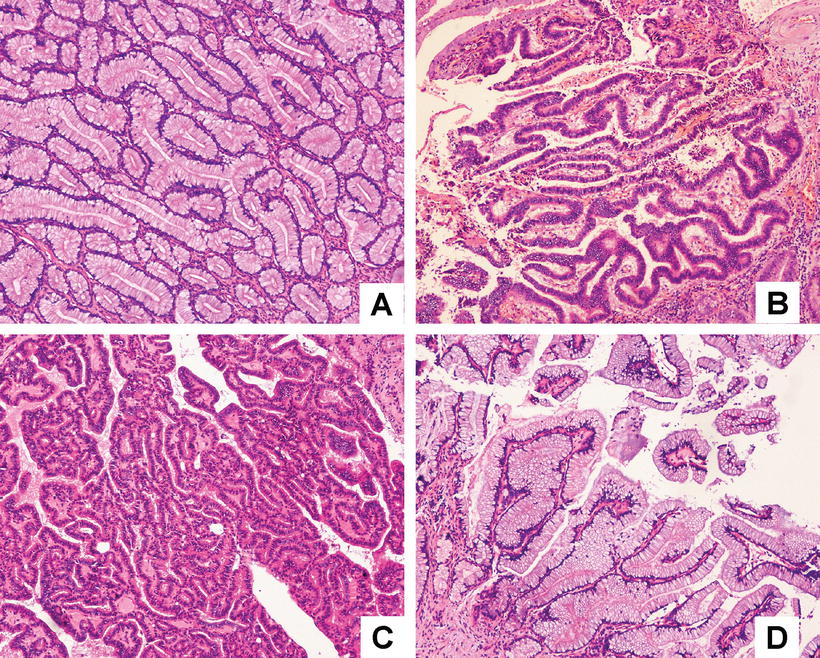
Fig. 9.2
Gallbladder adenoma: (a) pyloric gland type, (b) intestinal type, (c) biliary type, (d) foveolar type
- 1.
Tubular adenoma : The tumor consists of tubular glands which are lined by cubic or columnar epithelium and often located in the lamina propria, with clear boundary and a covering of normal gallbladder epithelium (Fig. 9.3a, b). Pyloric gland type accounts for 90% and intestinal type accounts for 10%. Pyloric gland type tubular adenoma consists of densely arranged pyloric glands, some of which are dilated into microcysts, and the glands are lined with mucus-secreting cubic or columnar epithelium. The cells contain lightly stained or vacuolar nuclei, and goblet cells and Paneth cells can be found between columnar epithelial cells, while squamous metaplasia can be visible in rare cases. 5-serotonin, somatostatin, pancreas polypeptides, or gastrin staining in immunohistochemistry can show the endocrine cells in small clusters. Large or intestinal-type tubular adenoma contains atypical hyperplasia in the epithelium, and 63% of the cases exhibit pseudopyloric gland proliferation in the nearby gallbladder epithelium, while Rokitansky-Aschoff sinuses (hyperplasia, subsidence and extension of normal gallbladder mucosa into the muscle layer) can be found in the adenoma tissues (Fig. 9.4a–b), which should be differentiated from adenocarcinoma .
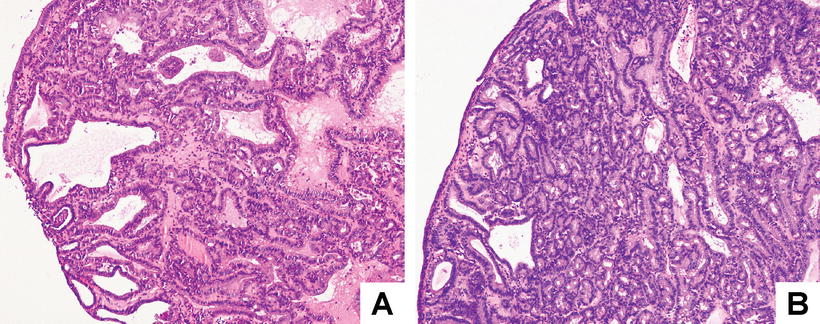
Fig. 9.3
Tubular adenoma : the tubular glands are lined with well-differentiated columnar epithelium (a & b)
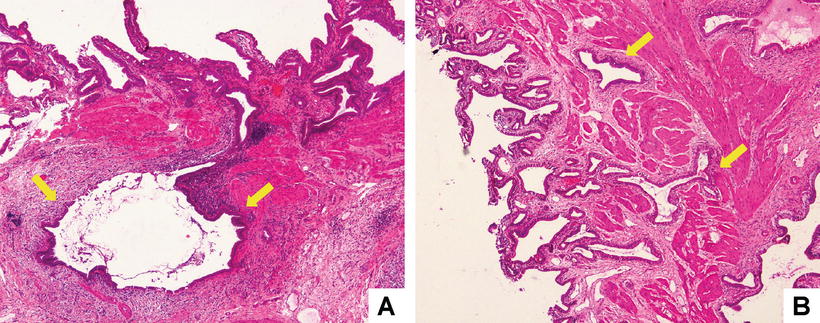
Fig. 9.4
Rokitansky-Aschoff sinuses: (a) Rokitansky-Aschoff sinuses refer to the hyperplasia, subsidence, and extension of normal gallbladder mucosa into the muscle layer (arrows); (b) arrows show the dilated Rokitansky-Aschoff sinuses among smooth muscle bundles
- 2.
Papillary adenoma: The tumor is divided into intestinal type and bile duct type. The former is composed of papillary glands lined with cubic or columnar epithelium, and there are more goblet cells, Paneth cells, and endocrine cells mixed between the epithelial cells. The pseudostratified epithelial cells contain little or rare cytoplasmic mucus secretion. The nuclei are round or long spindle and darkly stained, with a few mitotic figures (Fig. 9.5a–b). Sometimes it shows villous protrusions on the cell surface which can be diagnosed as villous adenoma, similar to the same kind of colon lesions. Tubular and villous structures can be found in a few cases named as villioustublar adenoma with varying degrees of epithelial dysplasia. Bile duct type is rare, which is coated with bile duct cuboidal epithelium on the papilla, and rare malignant transformation can be found [5].
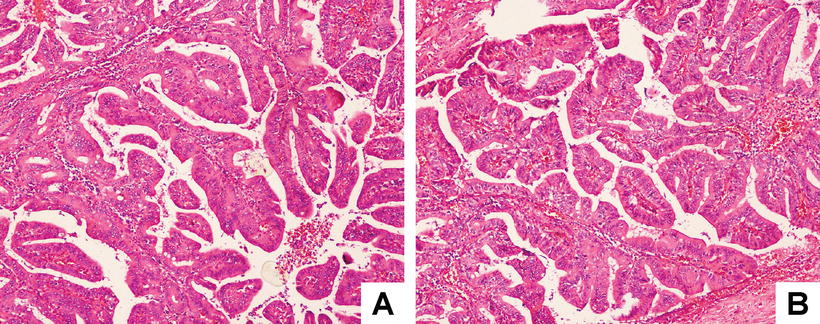
Fig. 9.5
Papillary adenoma: (a) papillary glands lined with cubic or columnar epithelium; (b) fibrovascular cores of the papilla
- 3.
Tubulopapillary adenoma: The tumor is composed of tubular glands and papillary structures, and each component at least accounts for more than 20% (Fig. 9.6a–b). The tubular glands can be pyloric gland type or intestinal type, with papillary structures lined with columnar epithelial cells containing mucous. Paneth cells and endocrine cells can be found in a few cases or with hyperplasia of pseudopyloric gland.
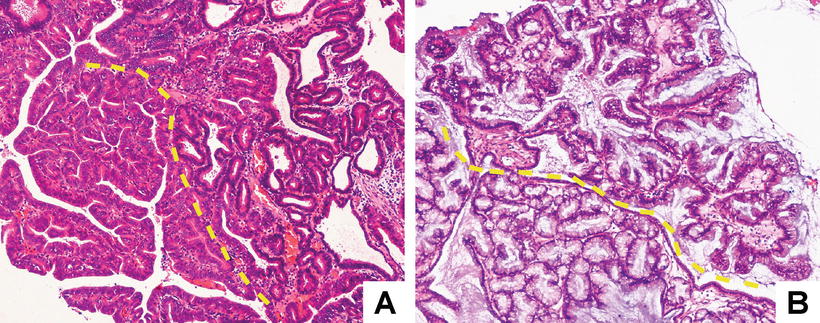
Fig. 9.6
Tubulopapillary adenoma: the tumor is composed of tubular glands and papillary structures (a & b) (the dotted line shows the boundary)
9.1.1.2 Cystadenoma
Cystadenoma is often found in extrahepatic biliary system, while gallbladder cystadenoma is rare and more common in middle-aged females. Grossly, the tumor can be lobulated, polycystic, or monocystic, containing mucus, serum, or hemorrhage, with calcification in the cystic wall. Cases with huge lesions may be accompanied by symptoms due to obstructive jaundice or cholecystitis. Under the microscope, the inner layer of the cyst wall is composed of columnar or cubic mucus-secreting epithelium, and the stroma is abundant and similar to ovarian stroma, with expression of estrogen and progesterone receptors. The interstitial tissues often contain varying degrees of fibrosis, and its outer layer is hyalinized fibrous tissue. It should be differentiated from gallbladder echinococcosis, abscess, adenomyomatosis , and septum gallbladder, and around 13% of the gallbladder adenoma may undergo malignant transforming into cystadenocarcinoma [6, 7].
According to the statistics in foreign literature, the canceration rate of gallbladder adenoma is 6–36%, while a group of domestic data shows the rate is 1.7%. In general, the gallbladder adenoma is not an important precancerous lesion for gallbladder carcinoma, because the incidence rate of gallbladder adenoma is very low and only 3% of early gallbladder carcinoma contain adenoma in the paracancerous adjacent mucosa [8]. In addition, gallbladder adenoma often has a β-catenin mutation which is rare in gallbladder carcinoma, and those genetic changes, often found in gallbladder carcinoma such as TP53, P16, and KRAS, cannot be found in gallbladder adenoma [9–11]. It is worth noticing that gallbladder adenoma or hyperplastic polyps with the following conditions should be closely followed up or treated by surgical resection as soon as possible: ① diameter of the lesions >1 cm,② diameter of the lesions <1 cm with rapid increase in volume (it has been reported that adenoma which was only 0.4 cm in diameter had already undergone malignancy), ③ multiple adenoma, ④complication with gallbladder stones, ⑤ wide base of the lesions with locally thickened gallbladder mucosa, and ⑥ older than 50 years old.
9.1.1.3 Biliary Intraductal Neoplasia (BilIN ) and Carcinoma In Situ (CIS ) of the Gallbladder
Biliary intraductal neoplasia in the gallbladder is often difficult to be identified due to complication with chronic cholecystitis, and the mucosal surface may be flat, papillary, granular, or nodular, with flat mucosa as the most common type. The main evaluation index includes ① cellular and nuclear atypia (cellular and nuclear pleomorphism, increased karyoplasmic ratio, thickened or irregular nuclear membrane, darkly stained chromatin), ② cellular and nuclear polarity, and ③ structural atypia (multilayered cellular and nuclear arrangement, micro-papillar or pseudo-papilla structure). And WHO classified gallbladder BilIN into the following three grades [12]:
BilIN -1 (low grade): The epithelium shows flat or low/micro-papillary structure, and the nuclei are almost in situ, with focal pseudostratified nuclei in rare cases which are still located in the lower two thirds of the epithelium. Cytology shows mildly abnormal nuclei, which have slight irregular nuclear membrane, increased karyoplasmic ratio, and elongated nuclei consistent in size and shape (Fig. 9.7a, b).
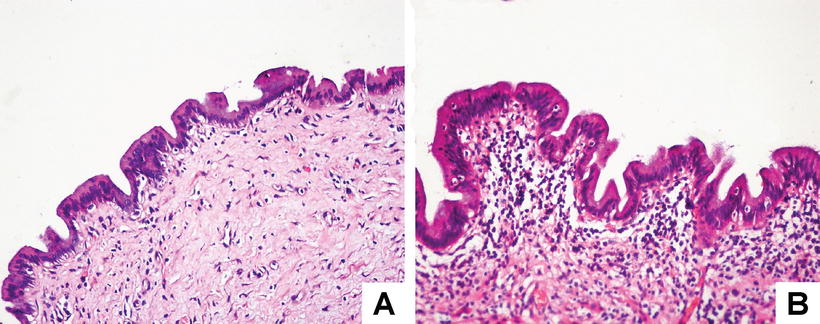
Fig. 9.7
BilIN -1 (a & b)
BilIN -2 (moderate grade): It can be flat or pseudo- or micro-papillary, often with absence of non-diffused cellular polarity, pseudostratified nuclei reaching the luminal surface, which are still located in the lower two thirds of the epithelium. Cytology shows obvious nuclear dysplasia and enlargement, darkly stained chromatin, irregular nuclear membrane, varying degrees of inconsistency in the size and shape of the nuclei, and rare mitotic figures (Fig. 9.8a, b).
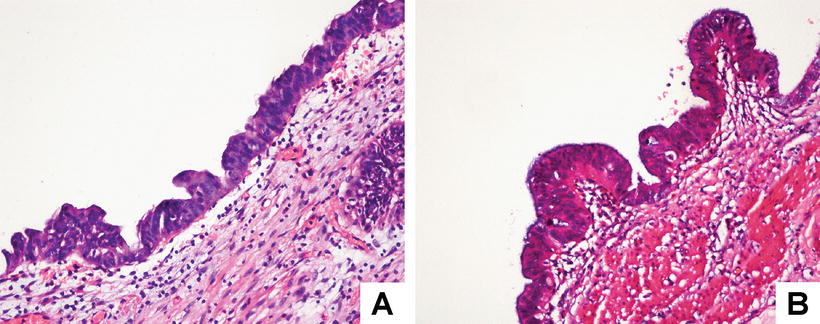
Fig. 9.8
BilIN -2 (a & b)
BilIN -3 (high grade): It often contains visible pseudo-papilla or micro-papilla, and cytology shows that it is similar to carcinoma without invasion throughout the base membrane. Diffuse and severe disappearance of cellular polarity can be found with nuclei located on the luminal surface. The epithelial cells protrude into the luminal surface in small bud clusters, forming cribriform structures. Malignant features can be observed in cytological examination, including markedly irregular nuclear membrane, darkly stained chromatin, and abnormally increased nuclei with visible mitotic figures (Fig. 9.9a, b).
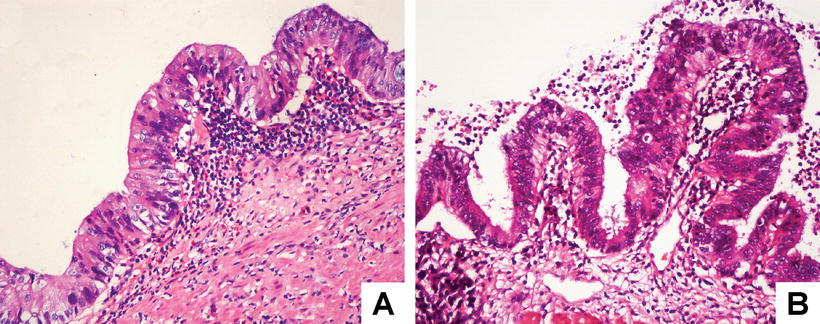
Fig. 9.9
BilIN -3 (a & b)
BilIN -3 has a incidence of 0.5–3% in patients with gallbladder stones, which is often accompanied by pyloric gland and intestinal metaplasia, and shares similar clinical features with gallbladder carcinoma, such as onset age, high-prevalence areas, predilection sites and molecular biological changes, etc. BilIN -3 is often a complication of gallbladder carcinoma and considered to be a precancerous lesion for gallbladder carcinoma, induced by cholelithiasis, familial adenomatous polyposis, sclerosing cholangitis and pancreatic-biliary reflux, and so forth [13]. The area of dysplasia is clearly separated from the surrounding normal epithelium. However, high-grade intraepithelial neoplasia in Rokitansky-Aschoff sinus should be identified from interstitial infiltration in gallbladder carcinoma [12]. And if the microscopic examination shows a lesion as BilIN -3, more samples should be examined to exclude gallbladder carcinoma. The morphological type of BilIN -3 can be the same with or different from the concomitant invasive cholangiocarcinoma in cases with both tumors. Immunohistochemistry demonstrates that the cells in intraepithelial neoplasia are positive for CEA, CA19-9, p53, and S100 A4 [14]. Different from dysplasia, reactive hyperplasia often contains flat epithelium, with no papillary structure or metaplasia and little changes in cellular polarity, slightly enlarged cell, round or oval and slightly enlarged nuclei, smooth nuclear membrane, and fine and uniformly distributed chromatin. Unlike dysplasia which contains monotype of cells, its cellular components are diverse, including columnar mucus-secreting cells, low cuboidal cells, and atrophic epithelioid and pencil-like cells, and the transition between it and normal epithelium is also gradual without clear boundaries.
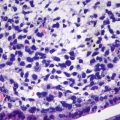
Carcinoma in situ (CIS ) shares the morphological characteristics with BilIN -3, but the lesions are confined to the mucosa and can be divided into micro-papillary type and flat type grossly. Dysplastic cells with obvious features of malignant tumors can be identified as CIS , such as frequent mitotic figures (2–10/HPF), crowded nuclei, enlarged glands, lessened stroma, close or back-to-back arrangement of the glands, lining of pseudostratified epithelium, and disappearance of cellular polarity, with intestinal metaplasia (Fig. 9.10). Albores-Saavedra et al. (2004) suggested that Rokitansky-Aschoff sinus with CIS is different from invasive glands in tubular tumors in that the former contain superficial epithelium connected to the invaginated epithelium with mixture of recognizable normal and tumorous epithelium, condensed bile content in the elongated and extended glandular cavities, and no invasion of smooth muscles. In addition, CIS extends along the Rokitansky-Aschoff sinus showing long glandular cavities through intramuscular connective tissues, while tumorous glands are often small- and medium-sized glands invading smooth muscle bundles or intramuscular connective tissues [15]. Furthermore, gallbladder stones can also result in multiple forms of mucosal changes of the gallbladder. Martinez-Guzman et al. (1998) analyzed 1096 cases of gallbladder stones, finding that mucosal epithelium with pseudopyloric gland metaplasia accounted for 50%, intestinal metaplasia 16%, low-grade atypical hyperplasia 40%, high-grade atypical hyperplasia 16%, carcinoma in situ 1.5%, and infiltrative carcinoma 2.6%, and the average age of patients with the latter four types of lesions was 42, 48, 53, and 61 years old separately. Segovia Lohse HA et al. (2013) conducted an analysis on the statistics of 1514 cases of cholecystitis, showing that pseudopyloric gland metaplasia accounted for 22.6%, intestinal metaplasia 2.1%, atypical hyperplasia 0.2%, and gallbladder carcinoma 0.6%, and the average age of the patients was 47, 46, 54, and 63 years old [16]. Both aforementioned data suggest that carcinogenesis is a gradually developmental process. As to the treatment for cases with BilIN -3 and invasive carcinoma confined to the lamina propria, surgical resection is the mainstream.
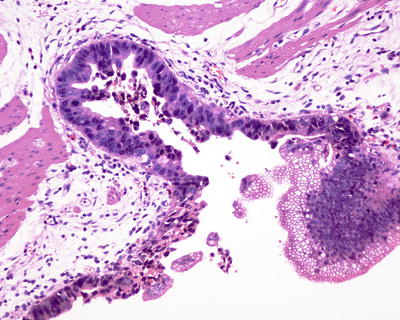
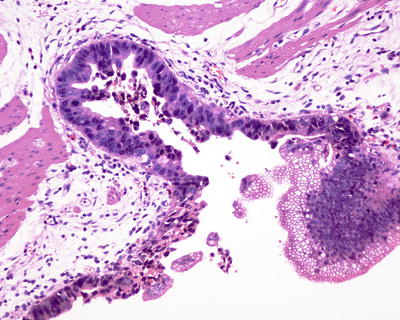
Fig. 9.10
CIS : the lesion involves the whole mucous layer but confined to the lamina propria
9.1.2 Benign Mesenchymal Tumors of the Gallbladder
Benign mesenchymal tumors of the gallbladder are rare, with a total incidence of less than 0.1% of all the specimens obtained in cholecystectomy. And the gross and microscopic morphology of these tumors are similar to the same kind of lesions at other sites.
9.1.2.1 Fibroma
Fibroma is often located in the bottom of the gallbladder, and the diameter of the lesions is often 0.8–1.2 cm, consisting of fibrous tumor cells or ganglion cells in rare cases [17].
9.1.2.2 Leiomyoma
Leiomyoma can be nodules in the gallbladder wall protruding into the cystic cavities, and leiomyoma of the gallbladder duct may cause obstruction. The lesions are often about 1 cm or even 4 cm in diameter. The microscopic observation shows the tumor consists of interdigitated bundles of leiomyomatous cells [18].
9.1.2.3 Hemangioma
Hemangioma is often cavernous angioma, and eight cases have been reported in the English literature [19], while three domestic cases have also been reported. Macroscopically, it is often lobulated, purple, and spongy, with a diameter of up to 6–8 cm, and can be connected to other intrahepatic blood vessels causing corresponding symptoms due to rupture, hemorrhage, and compression on the surrounding tissues. The patients may sometimes manifest as heart failure. Preoperative diagnosis of hemangioma is difficult, and it should be differentiated from malignant tumors of the gallbladder and hepatic tumors. Microscopically, the tumor consists of vascular cavities lined with vascular endothelium.
9.1.2.4 Lipoma
Lipoma consists of mature adipose tumor cells, and one domestic case of primary huge lipoma was reported by Nian-xin Xia et al. (2008), which was located in the subserosa of the gallbladder and 8 cm × 7 cm in size, and the patient manifested it as discomfort in the right shoulder, who was treated by surgical resection with a good prognosis [20].
9.1.2.5 Neurofibroma
Similar incidences are found in male and female patients, and the average onset age is 57.9 (32–77) years old. Approximately 50% of the patients are complicated by gallbladder stones. The tumors are small and located frequently in the neck of the gallbladder in a diameter of 0.4–1.5 cm. A case with the diameter up to 8.6 cm has also been reported. Under the microscope, they are composed of wavy slender spindle cells (Schwann cells), and their morphology and histogenesis are the same as those in other organs. Furthermore, they are related to NF-1 gene [21].
9.1.2.6 Paraganglioma
The tumors are located in the subserosa, usually well circumscribed as small round nodules, which can be up to 4.5 cm in diameter, protruding to the serosa. There have been eight cases reported in the foreign literature [22]. Microscopically principal cells are arranged in typical nest or acinar structures. Endocrine markers, e.g., CgA, Syn, etc., are positive, which needs to be identified from clear cell carcinoma .
9.1.2.7 Granular Cell Tumor (GCT)
GCT is rare, often found in young or middle-aged female patients. Clinically, cases with involvement of bile duct show cholecystalgia or abdominal pain or occasional obstructive jaundice, while those with involvement of the gallbladder may be asymptomatic. Involvement of cystic duct can result in complications, such as cholecystitis or gallbladder mucous cyst or hydrocholecystis, and gallbladder stones occasionally. Grossly, the tumors are light yellow, solid, and nodular, with unclear boundaries, and often protrude into the cavity of the gallbladder. The microscopic morphology of GCT in the gallbladder is similar to the same kind of lesions in skin and other organs [23].
9.1.2.8 Cystic Lymphangioma
So far, only 11 cases of cystic lymphangioma have been reported in the foreign literature, with a male to female ratio of 5:6, and the average onset age is 36 (17–66) years old. The maximum diameter can be up to 20 cm, and clinical symptoms due to compression by the lesions can be found in half patients, possibly complicated by acute Inflammation, rupture of the cyst, and intracystic hemorrhage. Symptomatic or huge lesions should be surgically resected. Microscopic examination shows the tumor consists of lymphatic tissues, lined with monolayer of endothelial cells, and the walls of varying thicknesses contain discontinuous smooth muscle inside. The morphology of the tumor is the same to the kind of lesions in other parts [24] (Fig. 9.12).
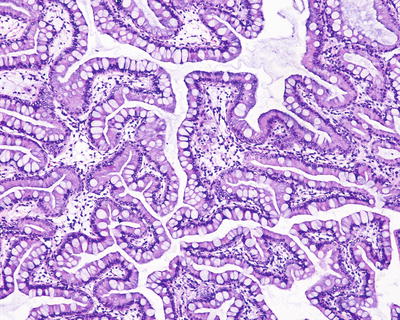
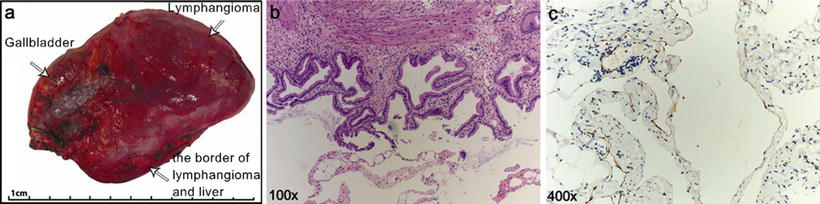
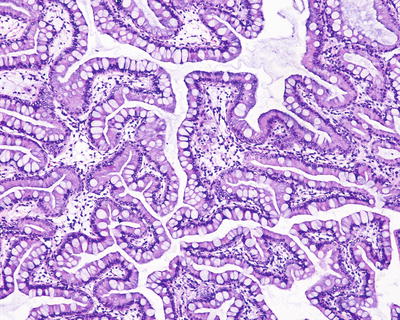
Fig. 9.11
Intestinal metaplasia: columnar epitheliums of the gallbladder adenoma mixed with many metaplastic goblet cells
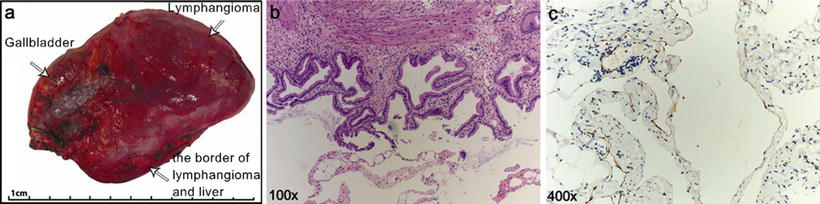
Fig. 9.12
Lymphangioma of the gallbladder: (a) gross specimen; (b) the tumor consists of lymphatic tissues, lined with monolayer of endothelial cells; (c) positive staining of endothelial cells with lymphatic marker D2–40
9.2 Malignant Tumors of the Gallbladder
9.2.1 Carcinoma of the Gallbladder
9.2.1.1 Pathogenesis and Mechanism
The incidence of carcinoma of the gallbladder ranks the sixth in gastrointestinal carcinomas and the first in malignant biliary tumors accounting for 85–90%, with <two cases per 100,000 people in low incidence area of the world. The incidence of gallbladder carcinoma in China is reported to be 2–5%. However, the pathogenesis of gallbladder carcinoma is still unclear, and 60–90% of the patients are complicated by gallbladder stones, suggesting the close relationship between cholelithiasis and gallbladder carcinoma. In addition, infection such as chronic cholecystitis and carcinogenic derivatives of cholic acid in the bile may also play a role in the pathogenesis of gallbladder carcinoma. Other risk factors include genetic susceptibility, geographical region, race and gender, obesity, smoking, Salmonella or Helicobacter pylori and other infectious factors, abnormal junction of pancreaticobillary duct, ulcerative colitis, familial polyposis, porcelain gallbladder, primary sclerosing cholangitis, etc. [25]. Recent studies found that the pathogenesis of gallbladder carcinoma involves accumulated mutations of multiple genes, such as activation of oncogene K-ras and telomerase; mutation and inactivation of anti-oncogene p53, p16, and FHIT; loss of heterozygosity of 3p and 8p alleles; and microsatellite instability of Rb gene [26], and its carcinogenic mechanism follows the sequential pattern of hyperplasia/metaplasia→dysplasia→carcinoma, which takes 5–15 years [27].
9.2.1.2 Clinical Features
It is mainly found in the elderly, and 90% of the patients are older than 50 years old with an average age of 67 years old. More female patients are involved with a male to female ratio of 1:(3, 4). Recent studies show that this gender difference may be related to estrogen and its receptors [28, 29] A total of 1089 cases of adenocarcinoma of the gallbladder have been diagnosed in the Department of Pathology, Eastern Hepatobiliary Surgery Hospital, Second Military Medical University from 2007 to August 2014, the average age of the patients was 59.9 (29–83) years old, including 433 males and 656 females, and the male to female ratio was 1:1.52. The clinical symptoms for gallbladder carcinoma include abdominal pain, jaundice, nausea and vomiting, etc., which are general gastrointestinal symptoms and difficult to identify from manifestations in patients with cholelithiasis; thus, it is difficult to make early diagnosis. Resectable lesions account for less than 20%. Some patients have enlarged gallbladder due to obstruction of cystic duct caused by the tumor. Serum CEA and CA19-9 levels are often increased, and hypercalcemia, leukocytosis, and elevation of serum HCG or AFP levels can be found in a few cases.
9.2.1.3 Gross Features
Carcinoma of the gallbladder can be grossly divided into three basic types, named massive type, nodular type, and invasive type, and the latter is the most common one, presenting diffuse thickening and hardening of the gallbladder wall, involving an area of up to 5 cm2 of the whole gallbladder. The sections are solid, firm, and hard in texture. The tumors can also be huge polypoid masses or nodules filling the whole cystic cavity. Occasionally, dumbbell-shaped gallbladder can also be observed due to cyclic infiltration. Generally, papillary adenoma has no pedicle and is polypoid or cauliflower shaped, while mucinous adenocarcinoma and signet ring cell carcinoma are superficially coated with myxoid jelly. Carcinoma of the gallbladder is most commonly found at the bottom of the gallbladder (60%), followed by the cystic body (30%), and rarely in the neck (10%); however, most cases involve the majority of the gallbladder when discovered, and it is difficult to identify the initiation site of the tumor. Direct invasion of the adjacent liver parenchyma is often found due to penetration throughout the gallbladder wall (Fig. 9.13).
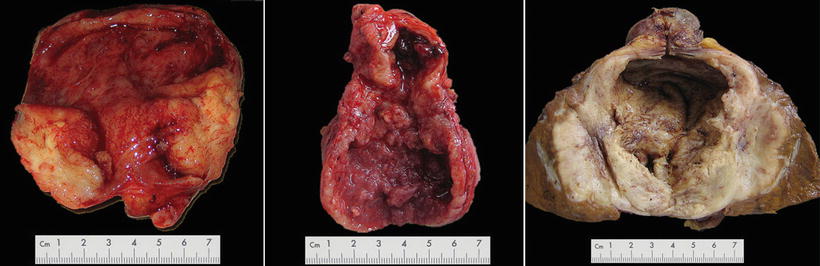
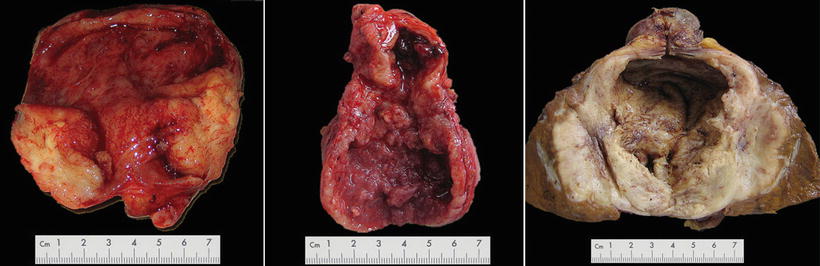
Fig. 9.13
Gross types: left massive type, middle nodular type, right invasive type
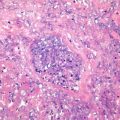
9.2.1.4 Microscopic Features
Adenocarcinoma
Adenocarcinoma is the most common histological type of gallbladder carcinoma, accounting for around 80% of all gallbladder carcinoma. According to the cellular morphology, gallbladder carcinoma can be divided into biliary type, intestinal type, and foveolar pattern. Biliary type is the most common type, in which the glands are lined with biliary epithelial cubic or columnar cells. Intestinal type contains tumor cells forming tubular or papillary structures, similar to colonic epithelium, containing a large number of goblet cells, and varying amounts of endocrine and Paneth cells. Foveolar type is the rarest and characterized by cells with basal location of the nuclei and large amounts of mucus contents in the cytoplasm.
Based on the degree of differentiation, gallbladder carcinoma can also be divided into well-differentiated, moderately differentiated, and poorly differentiated adenocarcinoma. Well-differentiated adenoma is mainly composed by well-differentiated tubular adenocarcinoma (Fig. 9.14), and the glands are lined with cubic or columnar epithelial cells, containing atypia nuclei with darkly stained chromatin and obvious nucleoli. These cells are multilayered or pseudostratified in arrangement, absent in polarity. About one third the tumors contain focal intestinal gland differentiation with varying number of endocrine cells, while Paneth cells are rare. The stroma of the carcinoma tissues contains marked fibrous hyperplasia. Poorly differentiated adenocarcinoma shows glandular differentiation to a certain degree, but most of the tumor cells are displayed in solid masses or cords (Fig. 9.15), with obvious fibrous hyperplasia. Some of the poorly differentiated adenocarcinoma cells are mainly small and round cells, distributed in patches, nodules, or cords, with vesicular nuclei, marked nucleoli, and little cytoplasm, and they should be differentiated from large cell lymphoma . Moderately differentiated adenocarcinoma is a tumor between well- and poorly differentiated adenocarcinomas (Fig. 9.16). Infiltration of the perineural tissues can always be observed in the adenocarcinoma of the gallbladder, with vascular tumor thrombus and invasion of the adjacent liver tissue (Fig. 9.17a–d). And the glands may contain varying amounts of mucus in the cavities, which is often salivary mucus, different from that in normal gallbladder and cholycystitis. The tumors can be cribriform or angiosarcomatoid, as well as osteoclast-like giant cells and trophoblast cells. Okada et al. classified the growth pattern of gallbladder carcinoma in the cystic wall into two groups, infiltrative growth type (IG type) and destructive growth type (DG type). Tumors in DG group have a poorer differentiation with lymphatic metastasis and vascular and perineural invasion, and their prognosis is poor [30] (Fig. 9.18).
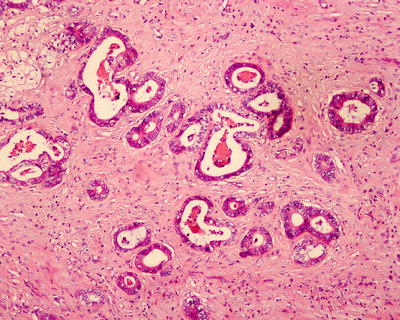
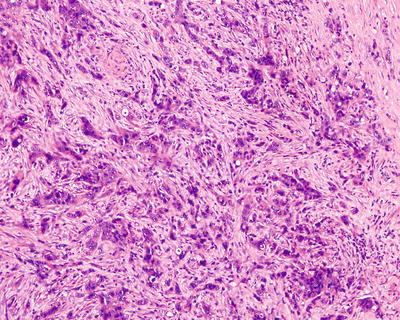
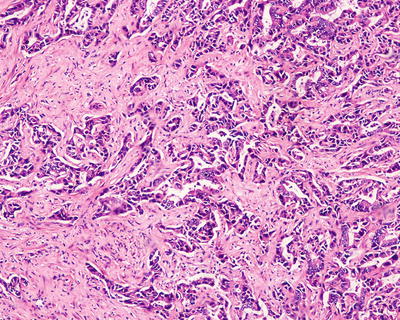
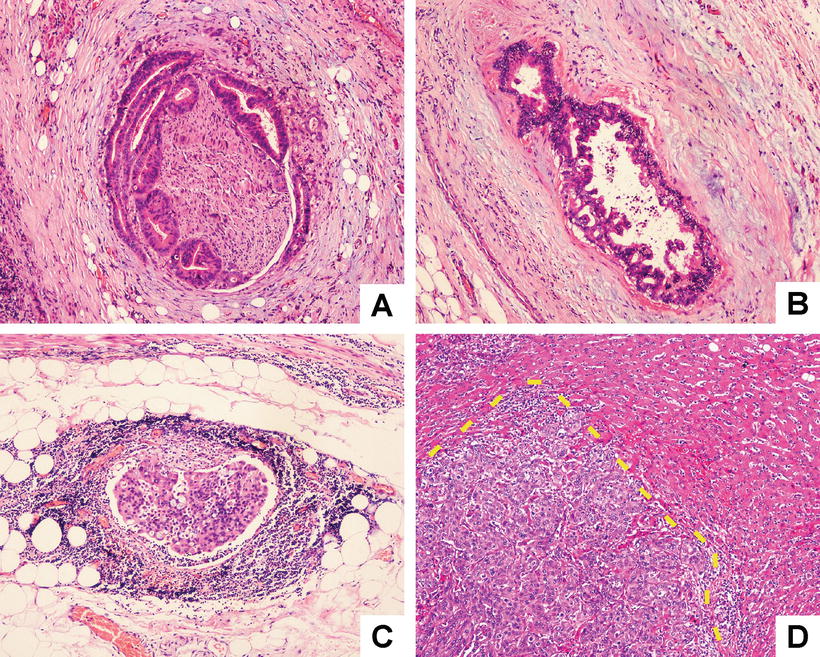
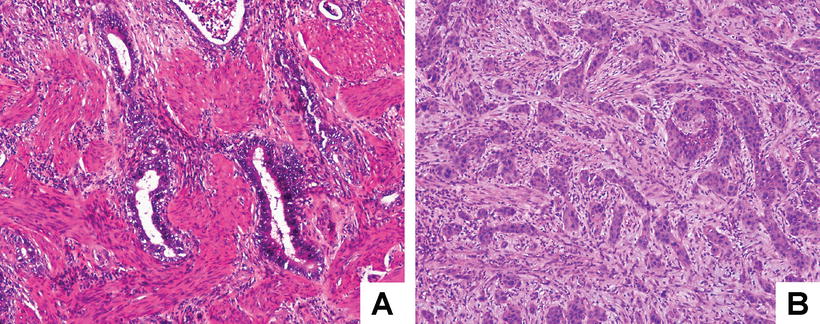
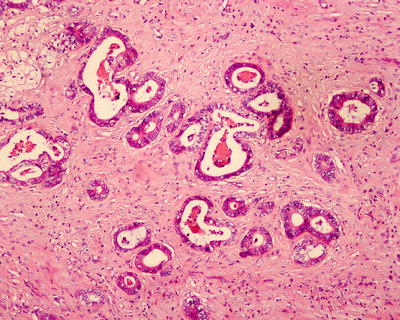
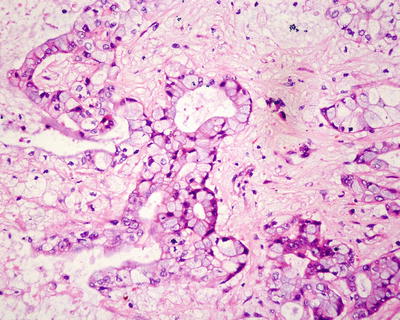
Fig. 9.14
Well-differentiated gallbladder adenocarcinoma: the glands are lined with cubic or columnar epithelial cells
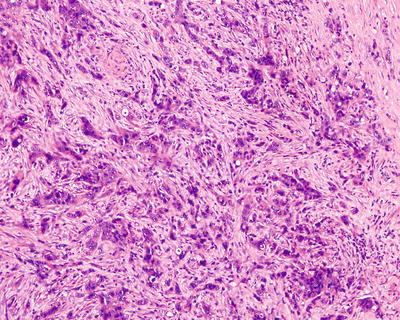
Fig. 9.15
Poorly differentiated gallbladder adenocarcinoma: the tumor cells are arranged in nest-like distribution or irregular glandular structures, with obvious atypia
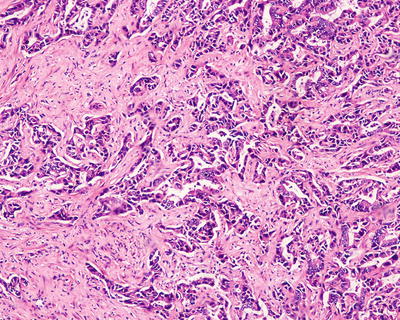
Fig. 9.16
Moderately differentiated gallbladder adenocarcinoma: moderately differentiated adenocarcinoma is a tumor between well- and poorly differentiated adenocarcinomas
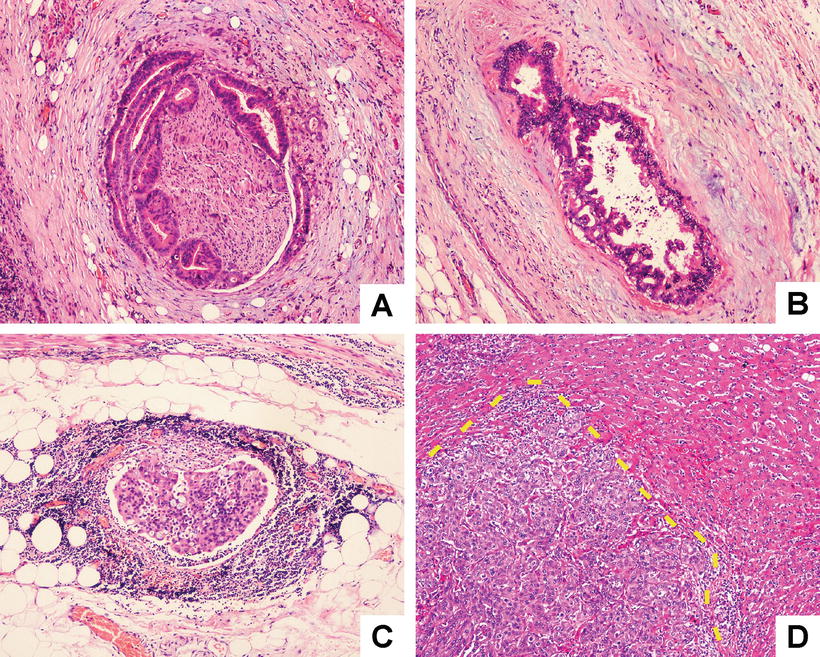
Fig. 9.17
Gallbladder adenocarcinoma: (a) perineural infiltration; (b) vascular tumor thrombus; (c) lymphatic tumor thrombus; (d) invasion of the adjacent liver tissue (the dotted line shows the boundary)
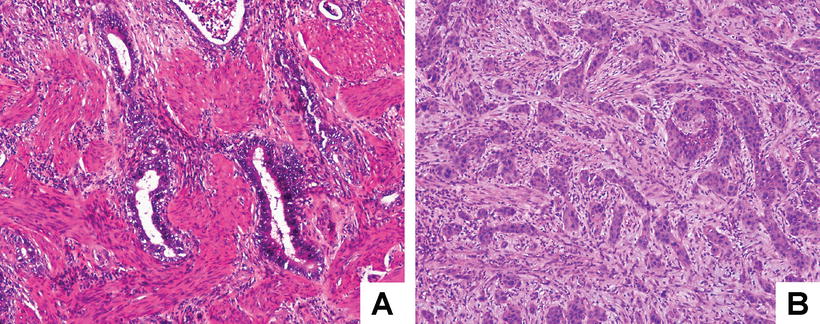
Fig. 9.18
Gallbladder adenocarcinoma: (a) cancer cells of IG type show infiltrative growth in the muscle layer (through the intermuscular space) without muscle layer destruction; (b) cancer cells of DG type invade the subserosal layer with destruction of the muscle layer. The DG type was accompanied by a stromal desmoplastic reaction which is active and irregular fibrosis due to the tumor invasion
9.2.1.5 Immunohistochemistry
Biliary type is often positive for CEA, MUC1, MUC2, p53, and CK7, intestinal type is often positive for CDX2, MUC2, CEA, and CK20, while foveolar type is positive for MUC5AC.
Cystadenocarcinoma
Cystadenocarcinoma of the gallbladder may derive from malignancy of cystadenoma , showing mono- or polycystic masses. The glands of the tumors are lined with epithelium which is similar to well-differentiated carcinoma, with or without varying number of endocrine cells [31]. Radical resection should be conducted with much caution via soft and gender operations to prevent rupture of the cysts and outflow of the cystic fluid, which can cause implantation and metastasis in the abdominal cavity [5].
Papillary Adenocarcinoma
The tumors are mainly papillary, lined with cubic or columnar epithelium, and they often contain varying amounts of mucus, while the degree of differentiation of the carcinoma cells is also inconsistent (Figs. 9.19 and 9.20). The tumors often show focal intestinal epithelial differentiation, with a large number of goblet cells, endocrine cells, and Paneth cells. Papillary adenocarcinoma grows primarily in the cavities and may fill the cystic cavity before the invasion of the cystic wall.
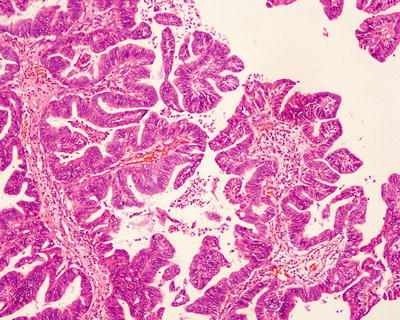
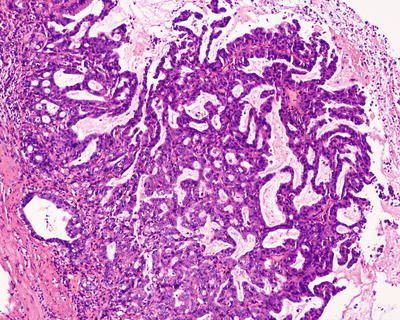
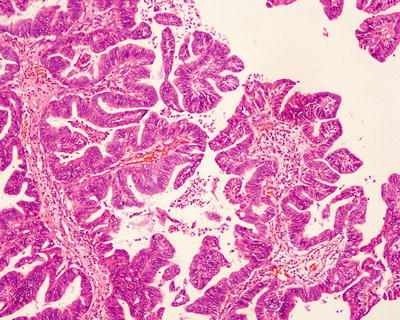
Fig. 9.19
Well-differentiated papillary adenocarcinoma
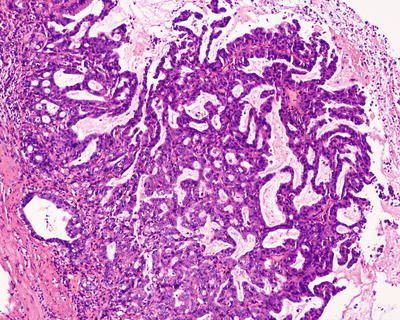
Fig. 9.20
Moderately differentiated papillary adenocarcinoma
Intestinal-Type Adenocarcinoma
Mucinous Adenocarcinoma
This type accounts for about 2.5% of gallbladder carcinoma, more common in middle-aged or elderly females. The lesions are large in size with an average diameter of 4.8 cm and are jelly on gross appearance which are similar to colloid carcinoma of the colon. The tumor contains extracellular mucus, which occupies more than 50% of the surface of the tumor. Microscopic observations show three growth patterns: tumorous glands lined with columnar cells, filled with mucus (Fig. 9.22); small clumps or long cords of carcinoma cells, containing abundant mucus, similar to signet ring cells; and mucus lake containing floating carcinoma cell masses. Well-differentiated cases should be differentiated from myxoid cysts or rupture of benign tubular or papillary R-A sinus which is filled with mucus. The prognosis is poor, since diffuse infiltration of cystic wall is often found, resulting in ulceration, perforation, and peritoneal metastasis, and the 3-year survival rate is only 1%. MUC2 can be used as a marker in the differential diagnosis from other gallbladder carcinomas [33].
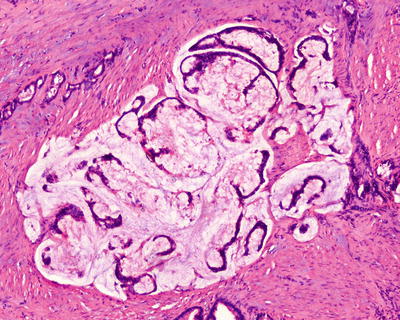
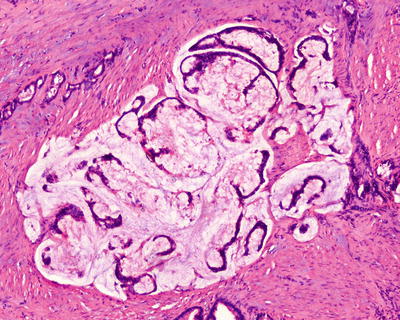
Fig. 9.22
The ruptured tumourous glands are full of mucus
Clear Cell Carcinoma
Clear cell carcinoma is rare, and the diagnosis could be made after the exclusion of metastasis of renal clear cell carcinoma . The tumors mainly consist of glycogen-containing clear cells, some of which have eosinophilic cytoplasm. The carcinoma cells have clear boundaries and darkly stained nuclei and are arranged in nests, sheets, cords, trabeculaes, tubules, or papilla (Fig. 9.23). Some of these carcinoma cells contain subnuclear vaculoes, similar to secretory phase endometrium, and careful observation helps to find the classic or mucinous adenocarcinoma region, with cells infiltrating the submucosa with partial invasion of adjacent liver tissue. The tumorous stroma contains abundant sinusoids, and obviously hyalinized fibrous septa can be found in deep infiltration area, as well as focal infiltration of lymphocytes. Most of the cases are positive for PAS, CK7, CK20, CEA, and EMA, and a few cases are positive for AFP [34].
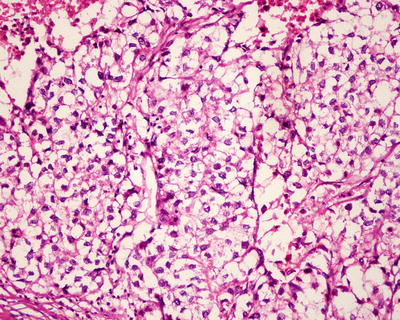
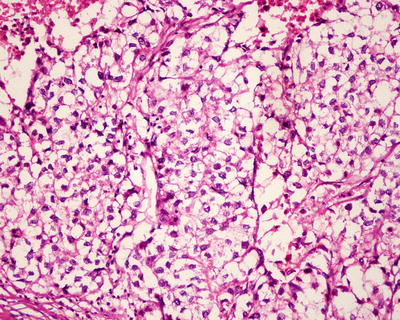
Fig. 9.23
Clear cell carcinoma is arranged in nests, with hyaline cytoplasmic inclusions
Signet Ring Cell Carcinoma
More than 90% of the tumors consist of mucus containing carcinoma cells, and the nuclei are deviated to one side of the cytoplasm forming a signet ring shape, due to the pushing of mucus (Fig. 9.24a–d). The carcinoma cells often arrange in diffuse sheets or nests [35]. A small amount of foam like histocytes may be observed in a few cases, which should be carefully differentiated from signet ring cells.
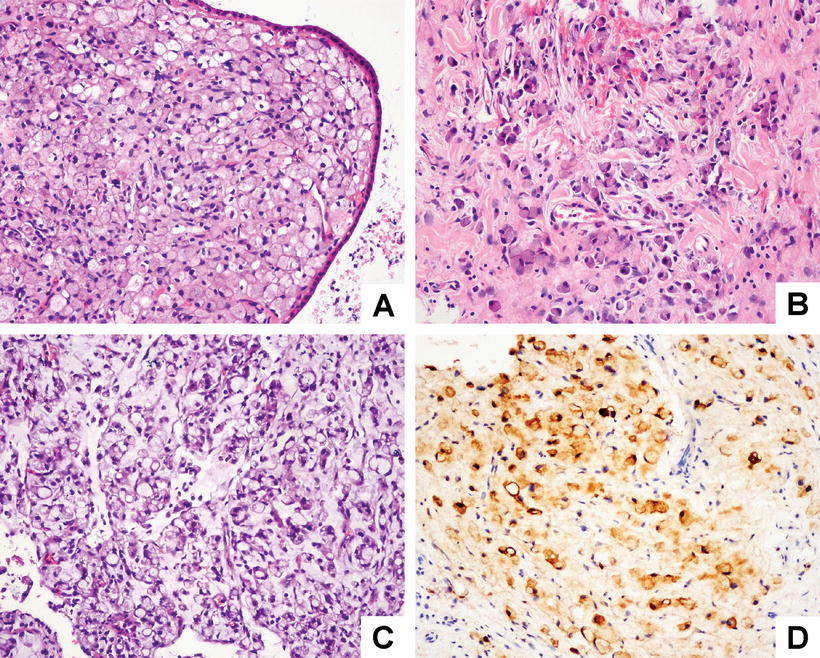
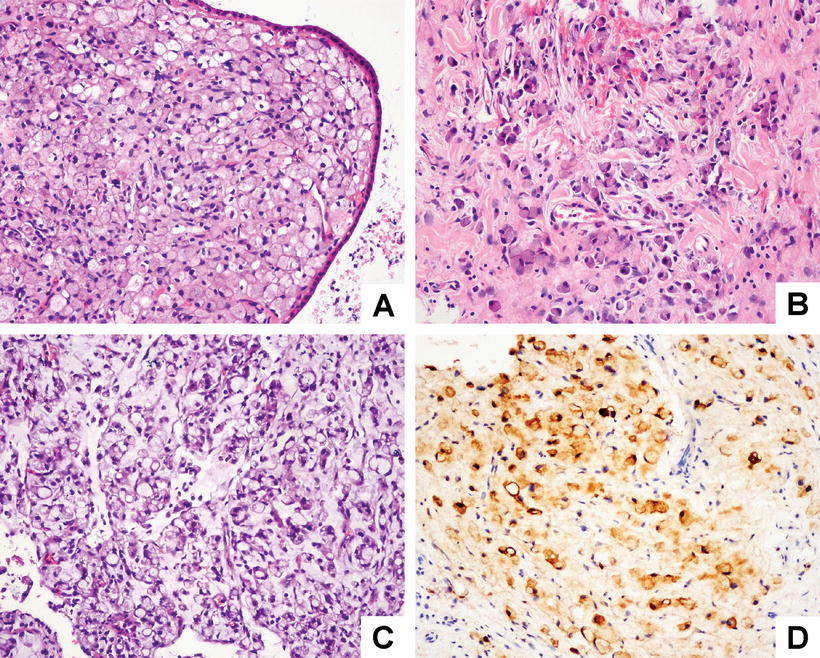
Fig. 9.24
(a) The tumor consists of mucus-containing carcinoma cells, arranged in nests under the mucosa; (b) muscular invasion; (c) the nuclei are deviated to one side of the cytoplasm forming a signet ring shape; (d) positive staining of signet-ring-like cells with epithelial marker CK
Adenosquamous Carcinoma
Adenosquamous carcinoma accounts for about 2% of gallbladder carcinomas, which consist of two components, adenocarcinoma and squamous carcinoma, in a varying proportion of different degrees of differentiation. It is generally believed that these two components occupy identical proportion; however, more than 30% of each component should be confirmed based on the consideration of deviation in distribution of tumor cells and sample drawing. Tumors with a certain component accounting for 15–30% can be described as adenosquamous carcinoma , with adenocarcinoma or squamaous carcinoma as predominant component; while those with components accounting for less than 15% should be defined as adenocarcinoma or squamaous carcinoma with other tumorous components. There is a transition between the two components. Squamous carcinoma is nest-like, containing cells of varying sizes with obvious atypia, rich cytoplasm, clear boundaries, marked nucleoli, and visible mitotic figures, with or without keratin pearl, keratinization in a single cell and intercellular bridges. Adenocarcinoma component contains tumor cells distributed in irregular glands containing mucus, and the cells are obviously atypic [36] (Fig. 9.25a–b). A few adenosquamous carcinoma may contain endocrine cells. And immunohistochemistry shows that squamous carcinoma component is positive for CK5/6 and CK34βE12, while adenocarcinoma component is positive for CK7 and CEA. Generally, the malignant degree of adenosquamous carcinoma of the gallbladder is much higher than that of common adenocarcinoma, and the prognosis is poor .
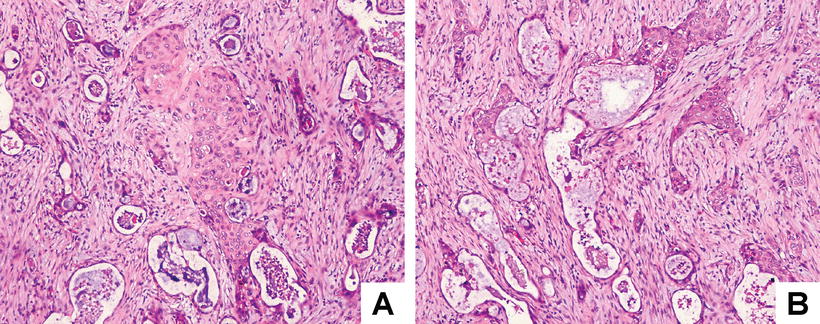
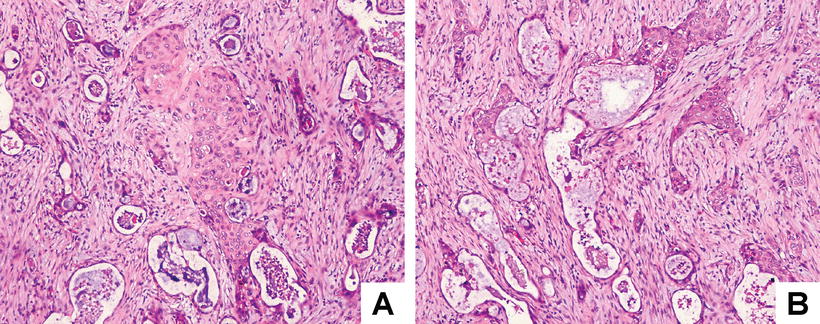
Fig. 9.25
Adenosquamous carcinoma of the gallbladder : (a) the tumor consists of two components, well-differentiated glands containing mucus and squamous differentiation regions with keratin pearls and intercellular bridges, and (b) there are transitional parts between these two components
Squamous Cell Carcinoma
Squamous cell carcinoma accounts for about 4% of gallbladder carcinomas and is grossly a grayish white, widely invasive mass, often deriving from squamous metaplasia of gallbladder mucosal epithelium. The tumors consist of squamous carcinoma cells [36] (Figs. 9.26 and 9.27) and can be divided into keratinizing and nonkeratinizing type. Generally, the tumor cells are positive for keratin and p63, while some poorly differentiated squamous cell carcinomas are mainly composed of spindle cells, which should be differentiated from some sarcomas, such as malignant fibrous histiocytoma or fibrosarcoma . Pure squamous cell carcinoma should be diagnosed based on careful examination of the specimens and multiple wide sampling, in order to exclude focal and small adenocarcinoma component. Its prognosis is poorer than common adenocarcinoma; however, lymphatic metastasis is rare .
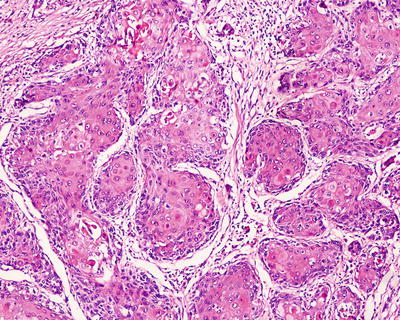
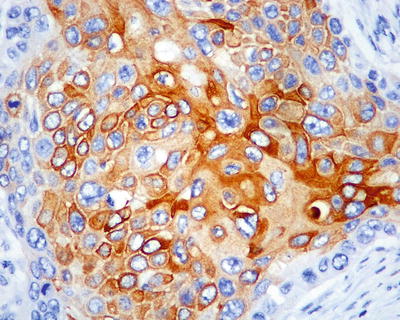
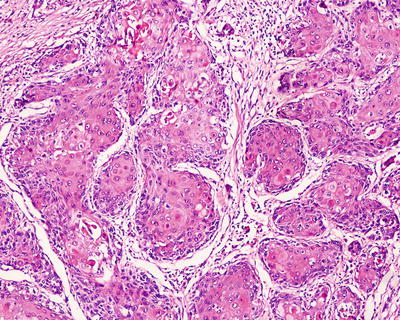
Fig. 9.26
The keratinized squamous carcinoma cells are arranged in nests, in an invasive growth pattern
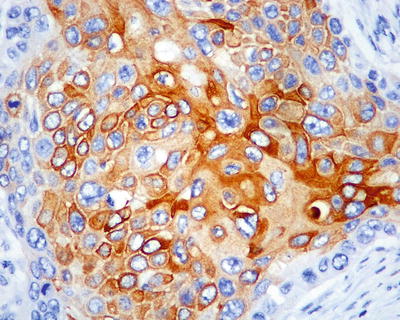
Fig. 9.27
The carcinoma cells are positive for CK19, with intercellular bridges
Neuroendocrine Neoplasms (NEN)
The 2010 edition of WHO classification of neuroendocrine tumors of the gallbladder includes neuroendocrine tumor (NET) , neuroendocrine carcinoma (NEC) , and mixed adenoneuroendocrine carcinoma (MANEC). Synonyms for NET include carcinoid tumor and well-differentiated endocrine tumors/carcinoma. And NET can also be divided into NET G1 (carcinoid) and NET G2. Synonyms for NEC include poorly differentiated endocrine carcinoma, high-grade neuroendocrine carcinoma , and small- and large cell endocrine carcinoma [12].
Carcinoid was first described by Joel (1929), and about 50 cases of gallbladder carcinoid have been reported in the current literature, considered to be rare tumors accounting for 0.2% of all carcinoids. Carcinoid is often solitary and 0.3–0.5 cm in size, often <2 cm in diameter, grayish white or grayish yellow, and polypoid or nodular in the submucosa. The microscopic images show that the tumor is solid and arranged in nests, cords, and glands. It occasionally grows penetrating the muscular layer. The cells are consistent in size, containing round or oval nuclei, nonobvious nucleoli, and red-stained cytoplasm. And immunohistochemistry shows that it is positive for neuroendocrine markers (Fig. 9.28). Cases of clear cell carcinoid of the gallbladder are rare, and only four cases have been reported in the literature, which were all found in middle-aged males, characterized by a large number of micro-lipid vacuoles in the cytoplasm. Ishida et al. (2012) reported one case of clear cell carcinoid of the gallbladder without VHL (Von Hippel-Lindau disease, an autosomal dominant inherited disease, characterized by clear cell tumors of multiple organs), and the Ki-67 index was only 0.8%. Immunohistochemistry showed that the tumor was positive for CgA and Syn, while it was negative for somatostatin and S-100. Furthermore, focal expression of CgA and Syn can be detected in the paratumorous regions with gastric gland metaplasia, while clear cell carcinoid with VHL is positive for somatostatin [37].
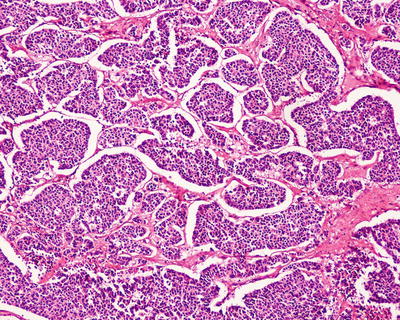
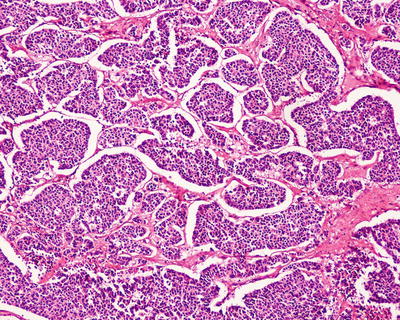
Fig. 9.28
Carcinoid of the gallbladder: the tumor cells are round or polygonal, arranged in nests, and they are consistent in size, with fine granular chromatin, pink cytoplasm, and fibrous stroma
Neuroendocrine Carcinoma (NEC )
Neuroendocrine carcinoma is a kind of tumor with strong invasiveness, high degree of malignancy, and poor clinical prognosis. The tumor can be found to invade the liver with lymphatic metastasis even when it is small; however, its clinical manifestations and imaging features show no specificity compared to adenocarcinoma of the gallbladder, and sometimes these two tumors are difficult to distinguish from each other even in histology. Immunohistochemistry shows specific neuroendocrine expression, which is the key point of diagnosis. Surgical resection or systemic chemotherapy is commonly used in the treatment .
- 1.
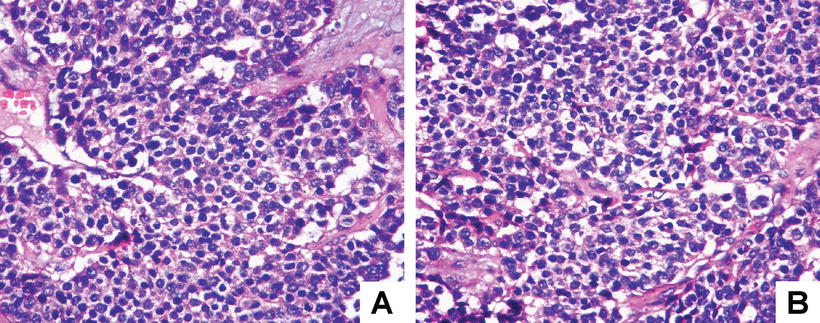
Small cell neuroendocrine carcinoma (SCNEC) accounts for 0.5–3.5% of malignant tumors of the gallbladder, and less than 100 cases have been reported in the literature, with the onset age of 25–86 years old which is averaged at 67 years old and female patients accounting for 66% [38]. The histomorphology of SCNEC is similar to that of small cell carcinoma of the lung, with poorly differentiated carcinoma cells, which are small round or short spindle cells, arranged in nests, sheets, cords, or ribbons, occasionally with Homer Wright rosettes and tubular structures. Diffuse necrosis and subepithelial invasive growth are the main characteristics. The nuclei are round or oval and darkly stained, with nonobvious nucleoli and common mitotic figures (15–20/10HPF) (Fig. 9.29a, b). Immunohistochemistry shows diffusely positive results for NSE and Syn and scattered positive images for CgA. In addition, tumor cells can also express epithelial markers, such as CK, CEA, AE1/AE3, etc., often with overexpression of p53 gene and loss of expression of pRb. Under electron microscope, the tumor cells contain round and dense core particles surrounded by capsules. And about 22% of the cases contain focal carcinoma areas, with 10% containing squamous cell carcinoma or carcinosarcoma areas, while half the SCNEC of the gallbladder may be complicated by other tumors. SCNEC of the gallbladder is highly malignant, and about 75% of the patients are found to have tumors with invasion of the serosa or metastasis during the operation, of which 90% are with muscular involvement. The average postsurgical survival time for cases with simple surgical resection is 4 months, 1-year survival rate is 21%, and 5-year survival rate is 0 [39].