Traumatic Brain Injury: Introduction
Traumatic brain injury (TBI) is common among the elderly mainly through the association with falls. TBI in the elderly presents special issues for the clinician to consider in the management of these patients, including a higher risk of poor recovery and physiatric and neuropsychiatric comorbidity. This chapter will review the epidemiology of TBI, mechanisms of injury, features on brain imaging, cognitive and psychosocial outcomes, and postacute management, with particular attention to research and practice with geriatric patients.
Epidemiology
TBI is craniocerebral trauma associated with decreased consciousness, cognitive or neurologic abnormalities, skull fracture, or intracranial injuries. More than 5.3 million Americans have disabilities related to TBI. With approximately 1.6 million incident cases per year, resulting in 1.2 million emergency department visits, 290 000 hospitalizations, and 51 000 deaths, TBI is a common cause of morbidity and mortality. Approximately 444 per 100 000 population are evaluated in the emergency department for TBI. In adults older than 85 years, the incidence of TBI-related emergency department evaluations is more than double the average (see Figures 68-1 and 68-2 for age breakdown). The annual incidence of hospitalized trauma or death is 101 per 100 000. The incidence of mild TBI across all ages (not resulting in hospitalization or death) is 392 TBI-related emergency department visits per 100 000 population.
Figure 68-1.
Incidence of emergency department (ER) visits with a TBI-related ICD-9 coding. Adults older than 85 yrs have high rates of TBI-related ER visits as do infants and toddlers. (This graph is derived from Jager TE, Weiss HB, Coben JH, Pepe PE. Traumatic brain injuries evaluated in U.S. emergency departments, 1992–1994. Acad Emerg Med. 2000;7(2):134–140.)
The economic consequences of TBI are alarming. The annual costs of TBI are approximately $60 billion. Estimates for the cost of lifetime care for a person with severe TBI range between $600 000 and $1.9 million. These estimates do not account for lost income of the patients, and time and lost earnings of family members who care for patients with TBI. Nor do these include the opportunities these victims have lost and their reduced quality of life.
Etiology
The older patient may have a number of age-related existing risk factors or conditions that increase vulnerability to both TBI and unfavorable outcome. These risks include, but are not limited to, cognitive slowing/impairment, orthopedic/mobility issues, visual acuity, balance difficulty, and neurologic and cardiac diseases. These issues increase risk for falls and motor vehicle accidents, the two major etiologies for TBI. These and other etiologies of injury are categorized in Figure 68-3. It is estimated that 28% to 36% of TBI are because of falls, followed by motor vehicle accidents (19%), being struck by or against an object (18%), assault (10%), others (11%), and unknown (10%). In the general population, men are twice as likely to sustain TBI as women, although this difference is negligible in the elderly.
Up to 60% of nursing home residents fall each year as do one-third of older adults in the community. It is significant to note that approximately half of all TBIs in the elderly are attributable to falls. In addition to being the most common mechanism of TBI, falls produce the highest rates of TBI hospital admissions. People aged 65 to 74 years are three times as likely to be hospitalized from a TBI-related fall as young adults. The risk ratio doubles for ages 75 to 84 years (7.6 relative risk) and doubles again for adults 85 years and older (16.4 relative risk). Similarly, the length of hospital stay is longer in the older adult, and the likelihood of being discharged to home is poorer. In adults older than 85 years, the rate of home discharge is 30%; for patients aged 75 to 84 years, the rate is 41%; at age 65 to 74 years, the rate is 54%; and in adults younger than 65 years the rate of home discharge is 86%.
Because falls account for the majority of injuries, an assessment of risk for falls is an important part of the geriatric evaluation. Risks such as the following should be considered: chronic neurological, sensorial, or musculoskeletal disease; alcohol use, acute illness and delirium, episodic hypotension, and potential medication effects; as well as activity and environmental risks. More on falls and their prevention are covered in another chapter.
Motor vehicle accident is the most common etiology of injury in the young adult. In the older adult, motor vehicle accident is the second most frequent etiology. Collisions are often at lower speeds but may still result in substantial injury. Key risks for motor vehicle accident include visual acuity and cognitive ability, particularly in the domain of attention—distractibility.
TBI-related death in the elderly is increasing. A CDC study found that for persons older than 75 years, the rate is 60 per 100 000 population. Falls, firearms, and motor vehicles were the most common causes. In hospitalized elderly patients with TBI, the rate of mortality is high for subdural hematoma (33%), followed by contusions (25%) and diffuse axonal injury (11%).
Types of Brain Injury
The circumstances, location, severity, and outcomes after brain injury are quite variable, although, some broad categorizations can be made regarding the mechanisms of injury (Table 68-1). Gennarelli indicates that there are two principal mechanisms of primary brain tissue damage in TBI: contact and acceleration/deceleration. Contact-related injury is the result of the head coming in forceful contact with an object (such as the floor or windshield), or contact between the brain and the inner surface of the skull. Contact injuries tend to result in cerebral contusions and hematoma at the point of contact. Not infrequently contra coup lesions occur opposite to the site of contact as the brain rebounds from the initial impact against the skull. Acceleration/deceleration injuries are the result of tensile shearing and straining forces acting on the tissue at the sudden moment of the impact. Such forces may tear blood vessels surrounding the brain, resulting in epidural or subdural hematoma or in widespread (diffuse) shearing of axons and microvasculature within the brain, which is termed diffuse axonal injury. The incidence of hematoma is very common in elderly patients with TBI, as a result of the fact that the proportion of brain volume to cranial volume is significantly smaller in the older adult, and the microvasculature is more brittle. These two factors may combine to yield more brain movement within the cranium at impact and higher incidence of hematoma owing to strain on the vessels, even with seemingly mild impact.
Primary injury |
Skull fracture |
Cortical contusions and arachnoid–pial layer lacerations |
Intracranial hematoma |
Diffuse axonal injury |
Diffuse microvascular injury |
Cranial nerve injury |
Secondary injury |
Hypoxia and ischemia |
Edema |
Increased intracranial pressure |
Infection |
Focal effects of trauma can be observed in variable locations throughout the brain, depending on the specifics of the injury. However, contusions are more frequently observed in the polar, inferior, and lateral frontal and temporal lobes. For example, the lesion in Figure 68-4 is large, but focal to the frontal lobe. Another mechanism for the increased rate of contusions in these areas is actual movement of the brain over the bony anterior and middle fossa and forward motion frontal impact sustained in motor vehicle accidents.
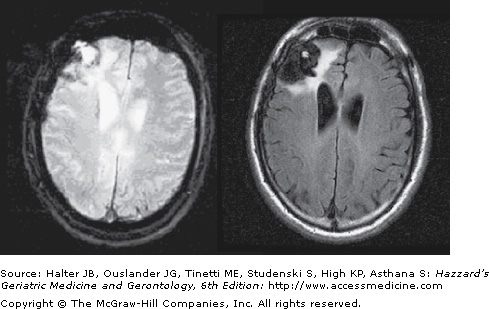
Figure 68-4.
A 52-yr-old male 14 months post injury. The patient was involved in a low-speed motor vehicle accident and sustained a skull fracture with right frontal epidural and subdural hematomas (that were subsequently evacuated surgically) and right frontal contusions. The T2*-weighted scan in the left panel is negative for diffuse axonal injury. The image on the right is FLAIR T2 and highlights the right frontal lesion with associated gliosis and encephalomalacia around the edges.
Extra-axial hemorrhages (epidural, subdural, and subarachnoid hematomas) are common in TBI, particularly in the elderly, and the presence of hemorrhage may impact the quality of outcome. A classic lucid period may be described in which the patient exhibits an impact-related alteration in consciousness, followed by a period where consciousness is regained, followed by secondary deterioration of consciousness as the hematoma evolves. Elderly have a higher rate of secondary hematoma even though the initial impact/injury may be mild. On computed tomography imaging, an epidural hematoma is an extra-axial biconvex ovoid mass of blood. Its biconvex shape is caused by blood accumulation in the epidural space, compressing the dura mater onto the brain, causing mass effect. Acute subdural hematoma involves blood accumulation between the dura and brain parenchyma. On computed tomography, subdural hematoma has a characteristic crescent shape. The inner boundary of subarachnoid hematoma is more irregular—characterized on imaging with blood accumulation that conforms to the sulcal and gyral pattern of the brain. Between 40% and 80% of patients with acute subdural hematoma have an initial Glasgow Coma Scale (GCS) in the severe range (8 or less). In severe cases of high-speed or penetrating injury, lacerations of the meninges may be present, owing to depressed skull fracture or rotational forces of the injury or from the penetrating object.
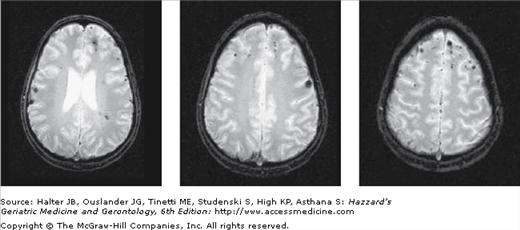
The diffuse effects of moderate-to-severe TBI can be seen throughout the white matter, indexed on gradient-echo MRI by small punctate hypointensities reflecting paramagnetic hemosiderin in the parenchyma, caused by microvascular shearing (Figure 68-5).
Figure 68-5.
Diffuse axonal injury. The patient was involved in a high-speed motor vehicle accident 3 months prior to this scan. The patient’s initial GCS at the scene was 5 and 3 following intubation. After 24 hours, the GCS was 7. At 3 weeks postinjury, the GCS was 11. By 4 weeks, the patient’s GCS was finally at 15. Day of injury imaging indicated a small left frontal epidural hematoma, left frontal contusions, and prominent diffuse axonal injury. This gradient-echo T2*-weighted axial series of images highlights areas of hemosiderin deposition, a blood byproduct containing iron, and therefore results in punctuate areas of signal loss (dephasing) on the image. The multifocal pattern of hemosiderin suggests microvascular shearing and diffuse axonal injury. The multifocal lesions mainly appear at gray–white matter junctions.
Secondary injury from diffuse axonal injury may involve a cascade of events, including defective axonal transport, swelling, and separation of proximal and distal segments of the axon for more than 12 to 24 hours. Further secondary injury may result from increased intracranial pressure, causing increased hypoxia and ischemia, and poorly regulated, excitotoxic release of glutamate and other excitatory neurotransmitters.
The GCS was developed by Jennett and Teasdale in 1974 and is still in wide use today to characterize the depth of coma, a major indicator of injury severity. The GCS is scaled from 3 to 15 (Table 68-2), with 3 being completely nonresponsive and 15 being completely alert, oriented, and following commands. Often the patient is necessarily intubated in the field, making an accurate assessment of GCS difficult.
Best eye response (E) | Spontaneous | 4 |
To speech | 3 | |
To pain | 2 | |
None | 1 | |
Best motor response (M) | Obeys commands | 6 |
Localizes to pain | 5 | |
Withdraws from pain | 4 | |
Flexion response to pain | 3 | |
Extensor response to pain | 2 | |
None | 1 | |
Best verbal response (V) | Oriented and coherent | 5 |
Confused conversation | 4 | |