Phenotype
Exon
Codon
ATA risk
Sporadic MTC
13
768
A
–
16
918
D
–
–
–
–
FMTC
11
630
B
–
–
631
B
–
–
634
B or Ca
–
–
649
A
–
–
666
A
–
13
768
A
–
14
804
A
–
–
819
A
–
–
833
A
–
–
844
A
–
15
866
A
–
–
891
A
RAS mutations have also been identified in spontaneous MTC. The RAS proto-oncogenes code for three highly similar GTPases, H-RAS, on chromosome 11p15.5, K-RAS, on chromosome 12p12.1, and N-RAS on chromosome 1p13.2. These GTPases have been shown to play an important role in many human cancers through activation of the MAPK cascade. H-RAS and K-RAS mutations are found in over 50 % of RET-negative MTCs [12]. The fact that RAS and RET mutations in MTC are almost mutually exclusive of one another suggests that both RET and RAS can act as driver mutations in MTC [13].
Diagnosis of Medullary Thyroid Cancer
In patients with a known hereditary risk factor, MTC usually presents as an elevated screening calcitonin level or nodule(s) on screening thyroid and neck ultrasounds . These patients tend to have a lower incidence of lymph node involvement and higher cure rates as a result of the routine screening. Patients with sporadic MTC often present with a palpable thyroid nodule or neck mass. The presence of a thyroid nodule in the setting of elevated serum calcitonin is essentially diagnostic of MTC. MTC can also be confirmed with ultrasound-guided fine needle aspiration (FNA) demonstrating C cells on cytology, and more accurately, measuring calcitonin levels in the aspiration needle washout, a test known as FNA calcitonin [14, 15].
There are important gender differences in calcitonin levels, with males having more parafollicular C cells and higher calcitonin levels at baseline than women. Therefore, gender-specific thresholds have been determined, with a basal calcitonin level of 20 pg/mL in women and 100 pg/mL in men, and stimulated calcitonin level of 250 pg/mL in women and 500 pg/mL in men having a positive predictive value of 100 % in detecting an occult MTC [16] .
Clinical Features of Medullary Thyroid Cancer
MTCs account for 5 % of all thyroid cancers. The most common age range of presentation is 35–45 years of age. The incidence in men and women is more evenly matched than other thyroid cancer histologies, with only slightly more than half of the patients with MTC being women .
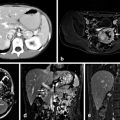
Sporadic MTCs are usually solitary lesions, while hereditary MTC presents with multicentric and bilateral disease in over 80 % of cases. Involvement of both central and lateral cervical lymph nodes is common in both sporadic and hereditary MTC. Early lymph node involvement is very common, with lymph node metastases occurring even with small primary tumors less than 1 cm in size (Fig. 1). The incidence of lymph node metastases increases with the size of the primary tumor [17]. In both sporadic and hereditary MTC, microscopic lymph node involvement in the central compartment level VI nodes was observed in 50–80 % of patients. High rates of micrometastases to the lateral neck level III and IV nodes were also appreciated, including the contralateral lateral neck nodes in patients with unilateral disease [17, 18]. Distant metastases are most frequently to the liver, lung, and bones. Rarely, brain and skin can also be sites of metastases .
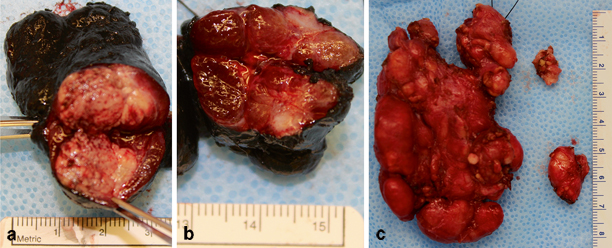
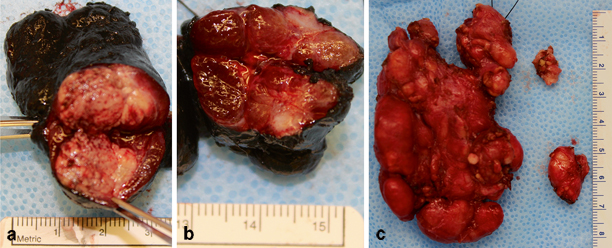
Fig. 1
Thyroid gland and right lateral lymph node compartments from a patient with bilateral synchronous lesions, lymph node metastases, and liver metastases: a left thyroid gland with primary tumor measuring 4 mm in greatest diameter, b right thyroid gland with primary tumor measuring 6 mm in greatest diameter, c right lateral neck compartments III, IV, and V had significant tumor burden involving the phrenic nerve, which was spared. Note that despite the primary tumors being small, lymph node involvement was extensive and the patient also had liver metastases. (Courtesy of Martha Quezado, M.D., Department of Pathology, National Institutes of Health)
Patients with MTC may experience anterior neck pain, which was found to be more common in MTC as compared to other differentiated thyroid cancers. In one series, the presence of neck pain translated to a more advanced stage of disease, with 82 % of patients with anterior neck pain being stage III or IV, and only 36 % of patients without pain being stage III or IV [19]. In addition to calcitonin and CEA, MTCs can also secrete vasoactive intestinal peptide (VIP), and infrequently, adrenocorticotropic hormone (ACTH) [20]. Therefore, in rare circumstances patients may have Cushing’s syndrome as part of their presentation. Patients presenting with systemic symptoms related to calcitonin or VIP burden, including bone pain, diarrhea, or flushing, almost universally have distant metastases [21] .
Meeting the criteria for FMTC necessitates two generations with MTC and no evidence of hyperparathyroidism or pheochromocytoma as first described by Dr John Farndon [22]. Other proposed definitions include MTC in four family members with no evidence of other MEN2 manifestations [23]. Overall, FMTC has a later age of presentation and is less aggressive biologically than MTCs in the sporadic or MEN2 setting [22]. Whether FMTC is a distinct entity or a specific phenotypic presentation of MEN2A is not concretely defined at this time, and some consider FMTC to be a variant of MEN2A.
Pathologic Features
MTCs are usually found in the upper third of the thyroid gland, due to the normal anatomic location of parafollicular cells . Grossly, the tumors appear well circumscribed, and nonencapsulated. Histologically, hyperchromatic spindle and polygonal tumor cells can be appreciated in sheets or nests separated by fibrovascular septa. The vast majority of MTCs have extracellular deposits of amyloid protein visible on microscopic examination. On immunohistochemistry, they stain positively for calcitonin and CEA (Fig. 2). In addition to the tumor, there are often areas of C cell hyperplasia (CCH) in patients with hereditary MTC. The diagnosis of CCH is made when three low power fields (area 1.93 mm2) contain over 50 calcitonin-positive cells which do not demonstrate any nuclear abnormalities, defects in the follicular basal lamina, or infiltration of the thyroid interstitium, as such qualities would be indicative of microscopic MTC [24] .
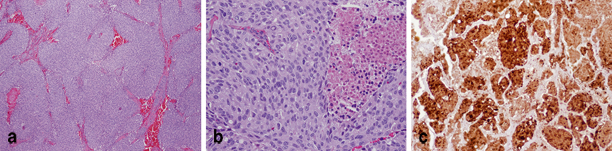
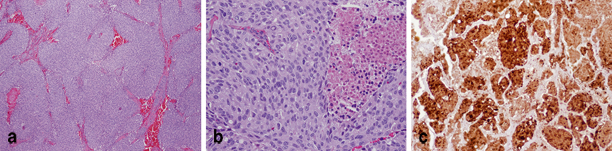
Fig. 2
Histopathology of medullary thyroid cancer: a hematoxylin and eosin stained MTC at 4× magnification view, demonstrating sheets and nests of tumor cells separated by fibrovascular septa, b at 20× magnification view, spindle and polygonal tumor cells with hyperchromatic nuclei can be appreciated, c MTCs are highly positive for calcitonin on immunohistochemistry, which stains brown. (Courtesy of Martha Quezado, M.D., Department of Pathology, National Institutes of Health)
Staging of Medullary Thyroid Carcinoma
Once a patient is diagnosed with MTC based on thyroid ultrasound and FNA, a basal serum calcitonin and detailed neck ultrasound should be obtained . The patient should undergo RET mutation testing, and pheochromocytoma should be ruled out using 24-h urine or plasma-free metanephrines and normetanephrines, and adrenal computed tomography (CT) or magnetic resonance imaging (MRI) if there is any uncertainty regarding biochemical screening results. Patients with no clinically appreciable lymph nodes on physical exam and neck ultrasound, and a basal calcitonin level under 400 pg/mL can proceed to surgical management for their MTC. If there are palpable nodes by physical exam, suspicious lymph nodes by ultrasound, or a basal calcitonin level over 400 pg/mL, a full metastatic workup should be initiated.
The metastatic workup for MTC should evaluate the liver using a sensitive imaging modality such as an MRI with contrast. Additionally, a neck and chest CT should be performed to further evaluate the neck compartments and determine whether lung metastases, which can frequently be bilateral, are present. (18 F)-fluorodeoxyglucose positron emission tomography can also be useful in detecting metastatic disease [25] .
Staging is then categorized by the American Joint Committee on Cancer (AJCC) tumor, node, metastases (TNM) classification system which has been adapted for all thyroid carcinomas, including differentiated thyroid carcinoma histologies ( see Chap. 15 on well-differentiated thyroid cancer).
Prognostic Factors in Medullary Thyroid Cancer
Age, gender, symptoms at presentation, extent of thyroidectomy, and TNM stage have been shown in univariate analysis to be significant prognostic factors in MTC . In a multivariate analysis, increasing age and advanced TNM stage were the only independent negative prognostic factors for survival [21, 26, 27]. Survival decreases dramatically with increasing stage (Table 2). Increased primary tumor size, positive lymph nodes, and distant metastases all decrease survival [28]. Early diagnosis and treatment have been shown to improve outcomes [29]. In patients with early MTC, treatment with total thyroidectomy and lymph node dissection results in a 95 % cure rate [21].
Table 2
Ten-year survival in MTC by stage
TNM stage | Overall survival (%) |
|---|---|
I | 100 |
II | 93 |
III | 71 |
IV | 21 |
A preoperative basal calcitonin level over 500 pg/mL is an excellent predictor of failure to achieve biochemical remission after surgery [30]. Biochemically persistent disease following total thyroidectomy is prognostic of decreased survival, likely because this indicates advanced stage and metastases [29]. Likewise, calcitonin doubling time (DT) is a strong and independent predictor of survival. In one series, a DT over 2 years corresponded to a survival of 100 % at 10 years, compared to a DT under 6 months, which had a survival of 8 % at 10 years [31] . In the same series, CEA levels did not always parallel calcitonin levels, and did not correlate with survival. Previous studies have shown CEA is less specific in predicting recurrence and survival, but may correspond to a less-differentiated cell population and worse prognosis when elevated [32–34]. Rapidly increasing tumor marker levels are highly suggestive of distant metastases, hence their ability to predict survival. Distant metastases are the cause of death in half of the patients with MTC. 1-, 5-, and 10-year survival after determining the presence of distant metastases is 51, 26, and 10–20 %, respectively [21].
Some studies of sporadic versus hereditary MTC suggested a difference in survival, while others have not [21, 27, 29]. What has been clearly demonstrated is the specific RET mutation, rather than if it is a somatic or germ-line mutation, has great prognostic significance in MTC because it predicts how aggressively a tumor will behave, which is the basis for the ATA risk stratification guidelines. Among sporadic cases of MTC, the presence of a somatic RET mutation correlates with larger tumors, nodal and distant metastases, advanced stage at diagnosis, worse outcome, and decreased survival [35] .
Surgical Management of Medullary Thyroid Carcinoma
The cornerstone of management for all patients with locally contained disease is a total thyroidectomy with central lymph node dissection (complete removal of all lymph nodes from the level VI compartment), and provides the best chance for cure in patients with MTC [25] . The complete central lymph node dissection does increase the risk of hypoparathyroidism postoperatively. Care must be taken to preserve the parathyroid glands and their blood supply, or to remove the glands and perform an autotransplantation. Permanent hypoparathyroidism occurs in 3–4 % of patients who undergo a central neck dissection [36]. The risk of transient or permanent injury to the recurrent laryngeal nerve is also slightly elevated with a lymph node dissection . However, the central compartment dissection is a vital component of appropriate treatment for MTC, and increases the cure rate [37]. Additionally, if any nodes in compartments II, III, IV, or V are suspicious on ultrasound or intraoperatively, or a patient has a calcitonin level over 400 pg/mL, these nodes should be removed [17, 38, 39]. Indeed, undertreated patients with only partial thyroidectomy or incomplete lymph node dissections have worse outcomes [40].
For patients with FMTC, prophylactic thyroidectomy can be considered based on the most recent ATA guidelines. Patients with level A and B germ-line mutations may delay prophylactic thyroidectomy, provided annual surveillance is in place and the family history suggests less aggressive tumor biology. Patients with level C germ-line mutations are recommended to undergo prophylactic thyroidectomy before the age of 5, and patients with level D germ-line mutations are recommended to undergo prophylactic thyroidectomy before the age of 1, although level D germ-line mutations are not generally observed in FMTC [25] .
Postoperative Surveillance
Calcitonin and CEA levels should be checked 2 months following a total thyroidectomy with lymph node dissection , and every 6 months afterward. If calcitonin levels are undetectable for 2 years, this interval may be increased to annual surveillance [25] .
Patients with detectable calcitonin levels postoperatively are not considered cured. These patients likely had an incomplete surgical resection, or have metastatic disease. In any patient with biochemical recurrence, a neck ultrasound and FNA or biopsy of any suspicious masses is recommended. In the event of biochemical persistence or recurrence, when basal serum calcitonin levels reach above 150 pg/mL, a full metastatic workup is recommended .
Management of Locally Recurrent Medullary Thyroid Carcinoma
For patients found during postoperative surveillance to have a local recurrence, surgical intervention should be considered . Subcentimeter indeterminate lymph nodes can be followed with serial ultrasounds. In one large retrospective study of patients presenting with persistent MTC and serum calcitonin under 1000 pg/mL who previously had no or incomplete neck dissection, reoperation and completion of lymph node dissection lead to biochemical cure in 44 % of patients with no prior lymph node dissection , and 18 % biochemical cure in patients with incomplete lymph node dissection [41]. While this has not yet been validated in a randomized control trial, this suggests complete lymph node dissections can significantly increase cure rates. External beam radiation therapy (EBRT) may also be used for locoregional control, to relieve pain, and avoid compressive complications [42]. Common toxicities are acute mucositis and dysphagia, and there is no current evidence that EBRT improves survival [43, 44] .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree