is an Academician of Chinese Academy of Sciences, International Cooperation Laboratory on Signal Transduction, Eastern Hepatobiliary Surgery Hospital, Second Military Medical University, National Center for Liver Cancer, Shanghai, China.
In recent years, the global economy and society have been developing in fluctuations and oscillations. Despite the significant progress achieved in medicine, science, and technology, the ongoing globalization and urbanization are challenging the nation’s ability to protect public health. The threat to human health posed by complex diseases such as malignant tumor, diabetes, hypertension, and coronary heart disease has not been weakened with the socioeconomic development; on the contrary, it even showed an increasing trend. As far as cancer is concerned, February 4 is the World Cancer Day. On February 3, 2014, the World Cancer Report was published by the International Agency for Research on Cancer (IARC), the official cancer organization under WHO. The report pointed out that cancer is one of the main causes for death globally, causing 8.2 million deaths in 2012. Throughout the world, cancers with the highest fatality rate include lung cancer (1.5 million), liver cancer (745,000), gastric cancer (723,000), colorectal cancer (694,000), etc. The report predicted that in the future 20 years, the annual number of new cancer cases in the world would increase to 22 million; meanwhile, the annual number of cancer deaths will increase from 8.2 million to 13 million [1]. The situation for global cancer prevention and control is very severe.
Even though the cancer incidence rate in China is not the highest, because of its tremendous population base, in 2012, 3.07 million cancer cases were newly diagnosed in China, accounting for 21.8% of the world’s total, and 2.2 million people died from cancer, accounting for 26.9% of the total number of cancer deaths worldwide. As far as liver cancer is concerned, over 50% of the world’s newly diagnosed liver cancer cases are in China, whose liver cancer deaths account for about 51% of the world’s total. The reason is that China is one of the regions of high viral hepatitis B prevalence. Over a hundred million hepatitis B virus carriers are important susceptible populations, and over 85% of liver cancer patients in China have evidence of hepatitis B viral infection.
Usually the incidence of liver cancer is accompanied by the typical “hepatitis-liver cirrhosis-liver cancer” process, but the pathogenesis from hepatitis to liver cancer is yet to be clarified. At present, screening and follow-up for high-risk populations is one of the important strategies for liver cancer control. In reality, China is lacking in convenient and effective means of liver cancer warning and surveillance for susceptible populations and does not have a scientific and reasonable molecular typing system. In the clinical diagnosis and treatment of liver cancer, difficult problems exist, such as nonspecific treatment method, high recurrence and metastasis rate, lack of basis for personalized treatment, few innovative efficient drugs, etc. Many hepatitis patients would turn pale at the mentioning of liver cancer because of the all-time high fatality rate of liver cancer, and the difficulty to cure hepatitis and treat liver cancer is also consuming an excessive amount of the already insufficient health resources.
The completion of the Human Genome Project and the progress of integrative biology and systems biology made it possible for early tumor prevention and early intervention of higher efficiency. With the development of medicine, a “4P” medical model has been proposed, i.e., preventive, predictive, personalized, and participatory. This model has initiated a new approach of medical research on tumor transformation. Once the breakthrough happens, it may bring about revolutionary changes to tumor prevention and control. Translational medicine is dedicated to filling the gap between basic experimental R&D and clinical application and shortening the time needed for a new diagnosis and treatment method to go from the laboratory to clinical stage. As a “B2B (bench to bedside)” continuous research and application development process, transitional medicine is now more commonly used in researches on malignant tumor including liver cancer. The key links of transitional medicine research are identification of biomarkers (the new parameter for the diagnosis and surveillance of tumor genesis and progression) through screening and R&D of new diagnosis technology, new treatment strategy, and new method. In recent years, China has gradually increased its investment in liver cancer research; initiated a batch of national scientific research programs, targeted at the key scientific problems of liver cancer; gathered teams with advantages in liver cancer research; established a technological innovation system combining production, study, research, and application; tackled key problems through collaboration; promoted the basic and clinical research on liver cancer; obtained a batch of important molecular markers through screening; actively explored new strategies of biotherapy for liver cancer; and implemented standardized combined therapy with enthusiasm and achieved initial success. Once the new products, new technologies, and new plans resulting from relevant researches are approved, they will be put into clinical use and application in high-risk areas. These practices will become valuable exploration of the innovative liver cancer research and clinical translation. Apparently, China is welcoming new leaps forward facing the challenges of liver cancer prevention and treatment.
2.1 Early Warning and Early Diagnosis Are the Breakthrough Points for Innovative Research on Liver Cancer
Based on the change of medical model and research idea, right now throughout the world, the key point for liver cancer prevention and control is screening for new markers, accelerating the transformation into clinical application, and improving the ability of risk prediction and early diagnosis of liver cancer. At present, the early diagnosis rate of liver cancer is extremely low in China, which greatly impacted the effect of liver cancer treatment. Considering China’s huge population base of chronic hepatitis B virus carriers and chronic hepatitis B patients, a systemic analysis targeted at these high-risk groups and liver cancer patients can help to achieve breakthrough in the prevention and early diagnosis and treatment of liver cancer and improve the level of liver cancer prevention and control faster.
A hot area of liver cancer research is screening for liver cancer-related markers or determining spectral pattern with various high-throughput “omics” technologies. Through large-scale screening for warning and diagnosis markers, China’s liver cancer researchers have already found out a batch of markers with proprietary intellectual property right and good prospect in clinical application, especially the important serological warning, early diagnosis, and pathological diagnostic markers such as MXR7 (GPC3), DKK1, and miRNA. Through multicenter and large-sample clinical cases, it has been confirmed that the combined use of these molecular markers and AFP can improve the accuracy rate of liver cancer diagnosis significantly [2]. Recently, many technical plans of hepatoma-specific early diagnostic reagent with proprietary intellectual property rights have been formed, some of which have been used in industrialization R&D through collaboration with enterprises, and will be applied and popularized in China’s hepatopathy diagnosis and treatment units and high-risk areas after obtaining CFDA approval. They will play a key role in increasing the early diagnosis rate of liver cancer, improving the treatment effect, and lowering the fatality rate.
2.2 Research on Molecular Regulation Network Will Provide New Drug Target for Biotherapy of Liver Cancer
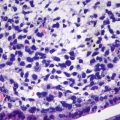
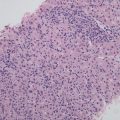
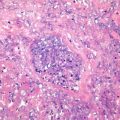
The genesis and progression of liver cancer result from the combination of genetic and environmental factors. It is a multilevel multistage dynamic development process, and the recurrence and metastasis caused by invasive growth is also a process of the steric effect of liver cancer cells and microenvironment, which involves the complex regulation network [3]. At present, we still lack specific prevention and treatment measures, the crucial reasons being the pathogenesis of highly heterogeneous liver cancer is not clarified and the panoramic analysis of the dynamic regulation mechanism of liver cancer is not completed.
The systematic understanding of the genesis and progression of liver cancer and the network regulation mechanism of inflammation-cancer transformation is of vital importance to obtaining specific drug target and also an important scientific problem in the research on liver cancer prevention and treatment, especially the research on the systematic regulation of signal transduction network of liver cancer cells and microenvironment and the research on interaction of host nervous system, hormone endocrine system, immune system, etc. and their role in the genesis and progression of liver cancer; they update and enrich concepts about the prevention, diagnosis, and treatment of liver cancer; provide new targets applicable to the research and development of new drugs for liver cancer; and ultimately realize effective and specific multi-target therapy.
2.3 Metabolic Abnormality Is Closely Linked with the Genesis and Progression of Liver Cancer
During the genesis and progression of malignant tumor, cellular metabolic features have experienced fundamental changes, promoting the malignant proliferation of tumor cells. The relationship between metabolic abnormality and tumor has never been neglected since the 1920s when Otto Warburg first reported about the Warburg effect, i.e., under well-oxygenated conditions, the glycolysis of tumor cells will also be greatly reinforced. In recent years, the content of the Warburg effect has been further expended: the metabolic features of tumor cells are significantly different from those of normal tissues in terms of nucleic acid, protein, enzymatic system, and glycometabolism [4]. Research shows that many metabolic pathways such as fatty acid, glutamine, serine, and choline metabolism have changed in tumor cells, all of which are collectively referred to as metabolic reprogramming [5].
The liver is the main metabolic organ of the human body with extensive participation in metabolic processes such as the absorption, synthesis, decomposition, storage, and transport of substances like sugar, protein, lipoid, and vitamins. If liver cells become cancerous, the original powerful metabolic capability of liver cells may very likely be “kidnapped” to create conditions for tumor growth. Evidence-based medical researches indicate a close relationship between metabolic diseases such as obesity, diabetes, and cardiovascular diseases and the genesis and progression of malignant tumors including liver cancer. The latest research shows that DMBG, the drug originally used for diabetes treatment, can reduce the risk of liver cancer and improve the prognosis of liver cancer patients [6].
Research on the interaction between the metabolic reprogramming of liver cancer cells and the body’s metabolic state and further clarification of the internal regulation network of metabolic phenotypes of liver cancer through interdisciplinary collaboration of cancer systems biology, metabonomics, bioinformatics, molecular imaging, epidemiology, etc. can not only help to understand the pathogenesis of liver cancer but also target at critical node points of the energy metabolism of liver cancer, interfere with cellular metabolic abnormality, and provide new ideas and strategies for the diagnosis, prevention, and treatment of liver cancer [7].
2.4 Liver Cancer Stem Cells Promote the Genesis and Progression and Recurrence and Metastasis of Liver Cancer
Recent researches indicate that tumor does not consist of homogeneous tumor cells. A small part of cells are equipped with the ability of self-renewal and continuous proliferation to form new tumor colony, and these tumor cells are referred to as cancer stem cell (CSC) or tumor-initiating cell (TIC) [8]. The traditional method of chemotherapy can inhibit the growth of tumor, but may lead to the accumulation of cancer stem cells, the existence of which may be the reason for tumor recurrence and metastasis and tolerance to chemotherapy [9, 10]. In-depth research on the signal regulation network of cancer stem cells in search for suitable therapeutic target is an international frontier scientific issue of liver cancer research. Clinical trials targeted at cancer stem cell therapy for rectal cancer and breast cancer have already begun in foreign countries, and the research results are worth expecting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree