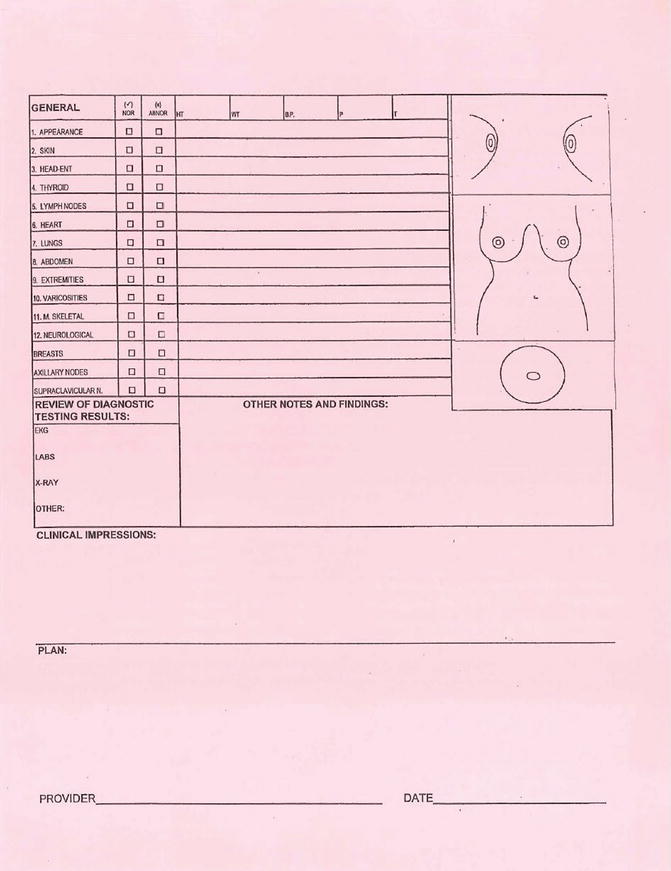
Fig. 7.1
(a, b) The Advocate Christ Medical Center’s multidisciplinary oncology breast clinic’s intake form
The history of present illness should note the means of how the cancer was initially identified, such as a palpable mass, an abnormality identified on a screening mammogram, nipple discharge, or the development of focal pain. Of course, it is important to obtain all outside imaging studies, with a personal review of such studies by both the treating surgeon and institutional breast radiologist. Tumor characterization, overall diameter, and clinical stage should be documented, with further evaluation of other imaging abnormalities that may not have been identified on the initial studies.
A thorough physical exam of the breasts and regional nodal basins should be performed [7]. If possible, evaluation of the regional nodal basin with ultrasound has been found to be helpful in the identification of suspicious-appearing lymph nodes that may require further evaluation and possible ultrasound-guided biopsy. Such information has clinical implications on the role, or lack thereof, for performing a sentinel node biopsy in the face of known nodal metastases [8, 9]. Accurate past medical and surgical histories are also important to obtain beforehand, as part of the general well-being of the patient and associated comorbidities that may potentially affect (alter) surgical, radiation, and medical oncology recommendations. A few such examples may be a previous history of mantle radiation for lymphoma or radiation for lung cancer, history of scleroderma, or connective tissue disorder that may prohibit or limit the use of radiation therapy.
A comprehensive history of current medications, including supplements and herbal medications, should be documented. Ideally, patients should bring their medication to the initial visit to avoid errors in the names of the drug or dosage. Allergies should also be identified, not only to medications, but also food, topicals, latex, and environmental substances. The review of systems is particularly important to identify possible coexisting conditions, second primary cancers, and findings suspicious for distant disease. A thorough menstrual and reproductive history should be obtained along with a history of hormone use such as oral contraceptives, impregnated intrauterine devices, depot contraception, hormone replacement therapy, and fertility drugs. It is also important to remember that cast menstrual period (CMP) is not an accurate reflection of menopausal state if a woman has had a hysterectomy without oophorectomy or has undergone a uterine ablation procedure. Ovarian function dictates endocrine therapy choices in hormone receptor-positive tumors and should be evaluated with FSH levels if any question exists [10].
A thorough family history of cancer is necessary to assess the risk of developing a genetically associated breast cancer. All types of cancer should be included, along with age at diagnosis, bilateral disease (where appropriate), and whether the family member experienced a recurrence of their cancer. A history of cigarette use, alcohol consumption, and recreational drug use should also be documented. All imaging studies should undergo a second opinion by your own department of breast radiology. Changes in interpretation of imaging studies and pathology findings can result in significant changes in the overall treatment plan [1, 4, 11, 12]. All outside pathology should also be obtained for second opinion by your institute’s breast pathologists in order to insure that the pathologic diagnosis is accurate and that the receptors, ER/PR and HER2-neu, are assessed at a minimum [13].
Evaluation of Local Disease Extent
It seems fairly intuitive that all patients who initially present with a diagnosis of breast cancer should undergo diagnostic mammography and ultrasound as indicated. As previously mentioned, ultrasound evaluation with biopsy of local nodal basins can be a valuable adjunct in establishing if there is any possibility of locoregional involvement. The decision to perform further imaging prior to the operation interventional is at the surgeon’s discretion, determined on need with each patient. The use of MRI or PEM technology should be critically applied, both in whom it should be used for and under what clinical circumstances. Mammographically, occult tumors, nodal metastases with an occult primary lesion, dense breast tissue, and unclear delineation of the primary tumor on mammography or ultrasound are all clinically reasonable situations where further evaluation of the breast with MRI or PEM may be appropriate. Breast MRI, in particular, is very useful for the surveillance of high-risk BRCA-positive patients and in the setting of neoadjuvant systemic therapy in order to evaluate the disease response [1, 13–18].
Evaluation of Distant Disease
The routine screening for distant disease in an asymptomatic patient with early-stage breast cancer is not indicated nor recommended [1, 19–21]. Overall, fewer than 6 % of patients will present with metastatic disease (stage 4) at their initial diagnosis [22, 23]. The NCCN treatment guidelines recommend additional studies for clinical stage I and IIB disease only if there are signs or symptoms that may raise the clinical suspicion of metastatic involvement, such as bone pain, or recent onset of headaches or vision changes. For patients with stage III breast cancer, the incidence of distant metastases at the time of diagnosis ranges from 8 % to 14 %, with the predominant site of metastatic disease found in the bone [20, 21, 23].
The presence of distant metastases in patients with locally advanced or symptomatic early-stage breast cancers may result in a significant change in the initial treatment strategy. An initial operative strategy may not be the best approach in the face of metastatic disease, with an initial systemic therapy approach with chemotherapy indicated. Systemic therapy considerations may also be altered, as endocrine therapy may be preferred over chemotherapy in hormone receptor-positive breast cancer. The most common, but not exclusive, sites of metastases for breast cancer are the bone, liver, lung, and brain. Early intervention in cases of potentially catastrophic and debilitating sequelae of distant metastases may improve quality of life in these patients. Table 7.1 outlines potential oncologic emergencies associated with metastatic breast cancer. There are many signs and symptoms that the patient may manifest, with pain the most common symptom identified (Table 7.2). The most common laboratory abnormalities are also listed in the face of metastatic disease (Table 7.3).
Table 7.1
Oncologic emergencies
Condition | Symptom | Morbidity |
|---|---|---|
Spinal cord compression | Back pain, leg weakness | Paralysis |
Bone metastases | Bone pain | Pathologic fracture |
Superior vena cava syndrome | Face/neck swelling | Dyspnea, trochlea compression |
Table 7.2
Potential symptoms of metastatic disease
Symptoms | Site |
|---|---|
Pain | Bone, visceral |
Leg weakness | Spinal cord |
Jaundice | Liver |
Dyspnea, cough | Lung, SVC syndrome, pleural effusion |
Headache | CNS involvement |
Seizure | |
Vision changes | |
Weakness | |
Confusion |
Table 7.3
Serum abnormalities associated with metastatic disease
Serum value | Site of concern |
|---|---|
Elevated alkaline phosphatase | Bone/liver |
Elevated liver function tests | Liver |
Hypercalcemia | Bone/paraneoplastic syndrome |
Anemia thrombocytopenia | Bone marrow |
Fertility
The incidence of breast cancer in women under the age of 40 is estimated to be about 1 in 200 [24], or 6–7 % of all breast cancers. For this group of young women, premature menopause, infertility, and the likely prolonged use of endocrine therapy and its affect upon fertility are all major concerns for those who wish to conceive in the face of breast cancer [25]. Fertility preservation should be addressed and, whenever possible, the patient referred to an oncofertility specialist [24]. Retrospective cohort studies have shown that there is no significant difference in cancer outcomes between cancer survivors who become pregnant after diagnosis and those who did not. Interestingly, many suggested a protective effect post-pregnancy [26].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree