Fig. 37.1
Preoperative clinical picture (a) of a severe diabetic foot infection including multiple anatomic compartments that required initial urgent surgical debridement followed by a revisional surgery with the use of negative-pressure wound therapy (b, c). The patient was followed closely in the postoperative period with frequent visits to a wound care clinic as well as further reconstruction with biologic dressings (d) and autogenous split thickness skin grafting (e)
Surgical off-loading with the utilization of external fixation can provide a stable construct that will protect any soft tissue reconstruction during the postoperative period. This method allows access to the surgical flap site for postoperative care and also aids in encouraging non-weight-bearing status for the recovery period if necessary. Careful patient selection with an appropriate rehabilitation regimen is paramount to avoid any inherent complications associated with reconstructive surgery in the diabetic population (Fig. 37.2).
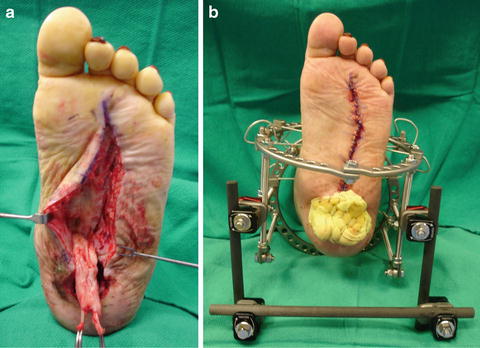
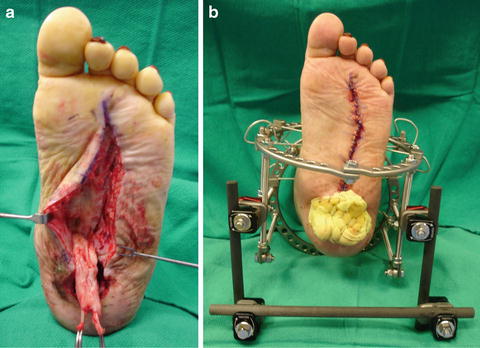
Fig. 37.2
Intraoperative clinical picture of a local flexor digitorum muscle flap (a) for coverage of a plantar central diabetic foot ulceration due to Charcot neuroarthropathy. Note the surgical off-loading by utilizing an external fixation device for postoperative care and non-weight-bearing status (b)
Diabetic Foot Infections and Amputations
Diabetic foot infections (DFIs) account for the largest number of diabetes-related hospital days and are the most common cause of non-traumatic lower extremity amputations [6, 7]. Many of the risk factors for DFUs also serve as the risk factors for DFIs, with diabetic neuropathy, PVD, and immunopathy having the most apparent influence. Hyperglycemia has a role in impairing the diabetic patient’s immune system through abnormalities in leukocyte function and changes in macrophage morphology. A pathologic cycle is created since elevated glucose levels inhibit the host’s defense to DFIs, while the presence of infection further affects glycemic control.
DFIs are diagnosed through a thorough history and physical examination, and confirmation can be made through laboratory testing and diagnostic imaging. The Infectious Diseases Society of America (IDSA) has defined the presence of infection as ≥ 2 classic findings of inflammation (purulence, erythema, warmth, pain, or induration) [8]. Local debridement and probing of the wound can help determine the severity and extent. Hospitalization and antibiotic therapy can be determined based on the IDSA category of clinical infection: mild (superficial and limited in size and depth), moderate (deeper or more extensive), or severe (accompanied by systemic signs of metabolic perturbations). As mentioned before, depending of the extent of the wound and infection, plain radiographs should be initially utilized to detect the presence of osteomyelitis and soft tissue emphysema. Magnetic resonance imaging (MRI) can provide information to help differentiate abscess, osteomyelitis, and neuropathic arthropathy.
Evidence of systemic toxicity (fever and leukocytosis), metabolic derangement, progressive deep soft tissue infection, gangrene, or the presence of critical ischemia warrants immediate hospitalization. Initial laboratory testing including complete blood count, metabolic profile, inflammatory markers, and hemoglobin A1C is important to establish a baseline and monitor response to treatment. Medical stabilization to correct electrolyte imbalance and control blood glucose levels is important prior to surgical intervention. Consultation with other services such as internal medicine, nephrology, endocrinology, infectious disease, and cardiology is determined based on the patient’s medical co-morbidities.
Empiric intravenous antibiotics may be started until reliable intraoperative deep cultures and bone biopsy when indicated are obtained to determine appropriate antibiotic therapy. Although most DFIs have been reported as polymicrobial, the most commonly isolated organisms are Staphylococcus and Streptococcus species [8]. Prior hospitalization and previous history of osteomyelitis increase the risk for infection by emerging multidrug-resistant organisms such as methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus. Surgical intervention should be initiated for early and aggressive debridement of the acutely infected diabetic foot with further recommendations for antibiotic treatment by the infectious disease team.
DFIs can have different manifestations such as local or extending cellulitis, abscess formation, gangrene, necrotizing fasciitis, and osteomyelitis. Isolated localized cellulitis can be treated via antibiotic therapy, whereas the other infectious pathologies necessitate adequate surgical debridement. Abscess formation can be addressed through incision and drainage with resection of adjacent nonviable tissues. Gangrenous tissue which results from local ischemia induced by acute bacterial toxicity should be sharply debrided and limb-threatening infections such as necrotizing fasciitis require emergent surgical debridement. Treatment options for osteomyelitis documented in the literature include antibiotics with or without surgical excision. Depending on the extent, such as in cases of joint sepsis or involvement of multiple anatomic foot compartments, a partial foot amputation may be required.
Surgical incision placement should take into account the angiosomes of the foot and ankle in order to preserve optimal vascularity [9]. If a minor foot amputation is required, the level of viable soft tissue and bone combined with the level of healthy perfusion should help guide the level of amputation. Multiple surgical debridements may be often necessary to adequately resolve the infection and produce a healthy granular wound that can be considered for future soft tissue reconstruction. Staged surgical procedures using local antibiotic delivery systems in the form of beads or spacers can be used to produce an infection-free yet mechanically stable environment for delayed reconstruction [10]. Major amputation may play a role in cases where infection involves the entire foot and is extending proximally to the leg or when arterial perfusion is not sufficient for diabetic limb salvage despite efforts for revascularization. Rehabilitation following an amputation can be facilitated by physical and occupational therapy services at home or in skilled nursing facilities if necessary. After surgical debridement and/or amputation, continued medical management, patient education, counseling, and postoperative care should be maintained in order to achieve long-term prevention of further complications.
Diabetic Charcot Foot Neuroarthropathy
Charcot neuroarthropathy (CN) is a complication of diabetic peripheral neuropathy that involves progressive fractures and/or dislocations that result in severe foot and ankle deformities causing potential for skin ulceration and infection. Diabetes mellitus is the leading cause of CN in the western world and each diabetic patient should be screened and educated about the risk of this debilitating condition [11]. The ideal situation in the subacute or acute stages of diabetic CN is to initially immobilize the patient and further protect the affected areas with appropriate custom bracing to prevent any related CN complications. Even with the early recognition of CN, certain deformities are not amenable to conservative treatment and require surgical reconstruction to establish a limb that is braceable, functional, and non-ulcerated. Continuous patient education about their loss of protective sensation and devastating complications of CN is essential to avoid a potential leg amputation. Close monitoring of this population with proper medical and surgical intervention when necessary is crucial for the overall patient’s successful outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree