© Springer International Publishing AG 2018
Philip T. Cagle, Timothy Craig Allen, Mary Beth Beasley, Lucian R. Chirieac, Sanja Dacic, Alain C. Borczuk, Keith M. Kerr, Lynette M. Sholl, Bryce Portier and Eric H. Bernicker (eds.)Precision Molecular Pathology of Lung CancerMolecular Pathology Libraryhttps://doi.org/10.1007/978-3-319-62941-4_1919. Targeted Therapies for Lung Cancer
(1)
Cancer Center, Houston Methodist Hospital, Houston, TX, USA
Keywords
Targeted therapyAdenocarcinoma of the lungEGFRALKROS1METHer-2RETKRASBRAFIntroduction
For many years, patients with advanced non-small-cell lung cancer (NSCLC) had poor prognoses because the disease did not have screening available and had a minimal response to available anticancer therapies. However, in the last 10 years, these patients’ outlook has improved due to two major therapeutic developments: the discovery that immunotherapy could achieve significant clinical responses in some patients and the identification of specific driver mutations that could be targeted by oral agents. This chapter will review clinical advances in the latter.
NSCLC is one of the most genomically diverse cancers, regardless of the histological subtype. This diversity creates immense challenges with respect to therapeutic options. Lung cancer is not a single uniform disease. On the molecular level, NSCLC can be stratified into discrete mutational subtypes that can be treated using different therapeutic approaches. One proof-of-principle example is the identification of a gain-of-function mutation in the tyrosine kinase-activating epidermal growth factor receptor (EGFR). This mutation is the best predictor for tumor response and overall survival following the administration of one of several FDA-approved EGFR inhibitors.
Biology
The perspective on NSCLC treatments has changed because of recent tumor biology studies. NSCLC cases can be subdivided into multiple molecular-level categories with variable prevalences [1]. Recent publications from the Cancer Atlas initiative and other groups have revealed significant tumor heterogeneity [2, 3]. The College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology has published guidelines for molecular testing of NSCLC. They recommend testing all advanced adenocarcinomas of the lung for mutations in EGFR, translocations in anaplastic lymphoma kinase (ALK) , and gene rearrangements in ROS1 regardless of clinical characteristics [4]. Testing for EGFR mutations and ALK translocations should also be considered for some patients with squamous cell histology, particularly among young patients with a light or nonsmoking history or a biopsy showing mixed histology.
Epidermal Growth Factor Receptor
EGFR is a member of the human epidermal growth factor receptor (HER)/erbB family of growth factor receptors [5]. These receptors are anchored to the cytoplasmic membrane and share a similar structure. They have an extracellular ligand-binding domain, a short hydrophobic transmembrane region, and an intracytoplasmic tyrosine kinase domain. Ligand binding activates receptor dimerization and tyrosine kinase autophosphorylation, which initiates an intracellular signaling cascade that activates multiple downstream receptor pathways. Activation of the RAS/RAF and phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt) pathways and transcription of their target genes leads to increased cell proliferation, angiogenesis, metastasis, and decreased apoptosis [6].
The presence of EGFR mutations is both a prognostic and predictive indicator [7]. EGFR mutations (detected using gene sequencing) hyperactivate EGFR, rendering the cancer cell dependent on EGFR for survival and progression. In NSCLC , activating mutations mostly occur in exons 18–21 [8]. The classic mutations, which occur in exon 19 and 21, account for 90% of EGFR mutations. Exon 19 mutations are commonly in-frame deletions of amino acids 747–750. Exon 21 mutations typically cause an L858R substitution. EGFR status at diagnosis is often mutually exclusive of aberrations in KRAS and ALK. It is also associated with certain clinicopathologic features, including a never or light smoking history, female sex, and Asian ethnicity.
Anaplastic Lymphoma Kinase
The ALK gene, which encodes a tyrosine kinase, was first identified in a subset of anaplastic large-cell lymphomas. In 2007, Soda and colleagues first identified the echinoderm microtubule-associated protein like 4 (EML4)-ALK fusion from a Japanese patient with lung adenocarcinoma [9]. The fusion is caused by an inversion on the short arm of chromosome 2 (p21p23) that joins exon 1–13 of EML4 to exons 20–29 of ALK [10]. The fusion activates the tyrosine kinase of ALK and drives downstream pathways that lead to cell proliferation and survival. Estimates indicate that 2–7% of NSCLC cases could harbor this oncogenic driver. ALK can also fuse with other partners, such as tropomyosin receptor kinase or kinesin family member 5B (KIF5B). These fusions have been described in lung cancer but are less common than EML4-ALK [11, 12].
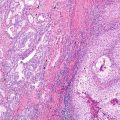
Immunohistochemistry (IHC), fluorescence in situ hybridization (FISH), and polymerase chain reaction (PCR) can all be used to identify ALK rearrangements. Of these, FISH is used most frequently in the clinic. However, it is increasingly apparent that IHC produces equivalent results while being cheaper and faster than FISH [13, 14]. EML4-ALK translocations are associated with certain clinicopathologic features, including young, never, or light smoking patients with adenocarcinoma, specifically those with signet ring-subtype histology [15, 16].
ROS1
ROS1 gene rearrangements are oncogenic drivers that are present in approximately 1–2% of NSCLC tumors [17]. ROS1 is a receptor tyrosine kinase of the insulin receptor family. Chromosomal rearrangements involving the ROS1 gene were originally described for glioblastoma. ROS1, located chromosome 6q22, is fused to the adjacent gene, fused in glioblastoma (FIG). ROS1 fusions were later identified as potential driver mutations in NSCLC cell lines (i.e., HCC78, SLC34A2-ROS1). These fusions have constitutive kinase activity. Similar to many oncogene-addicted lung cancers, tumors with ROS1 rearrangements commonly occur in young nonsmokers with lung adenocarcinoma histology.
BRAF
BRAF is a proto-oncogene encoding a serine/threonine protein kinase that promotes cell proliferation and survival [18]. BRAF lies downstream of RAS in the RAS-RAF-mitogen-activated protein kinase (MEK)-extracellular signal-regulated kinase (ERK) pathway and is a key molecular cascade in cellular growth. BRAF mutations account for 2–4% of NSCLC tumors [19]. Unlike melanoma, in which the majority of BRAF mutations are V600E, only approximately 50% of NSCLC cases harbor a V600E mutation. Other documented mutations include K601 N, L597Q, and G469 V. Similar to EGFR mutations and ALK fusions, BRAF mutations are generally exclusive of other driver mutations. However, unlike EGFR mutation and ALK rearrangements, BRAF mutations are common in patients who are current or former smokers. Clinically, BRAF-mutated lung cancers tend to have a worse prognosis, and many patients with early-stage BRAF-mutated lung cancer develop secondary tumors with KRAS mutations [20].
KRAS
KRAS mutations are among the earliest mutations discovered in human cancers and are the most commonly found mutation in lung cancer adenocarcinomas. They are observed in up to 30% of patients. Unfortunately, there are no KRAS-specific therapies at this time. These mutations are often associated with smoking, although approximately 5% of nonsmokers can have KRAS mutations. Activated KRAS can drive a number of downstream cellular pathways, including the MEK pathway. A number of MEK inhibitors have been studied to see if it is beneficial to block the activated MEK pathway; however, the drug was not effective in a recent clinical trial [21]. It may still be worthwhile to test biopsy specimens for KRAS mutations, because an EGFR-, ALK-, and ROS-negative result with a KRAS-positive result would eliminated the need for further driver mutation testing.
Human Epidermal Growth Factor Receptor-2
Her-2 mutations are seen in approximately 1–2% of lung adenocarcinomas. 97% of the time, when present they are found in female patients with a light or never smoking history [22]. Unlike the Her-2 mutations seen in breast cancers, the activating mutations in lung cancer patients are exon 20 insertion mutations. Gene amplification and overexpression do not appear to be causative factors for lung cancer tumorigenesis, and the exon 20 insertion is usually mutually exclusive of other driver mutations.
MET
MET is an attractive target for lung cancer therapeutic development; however, molecular clues as to which patients would benefit from this therapy have only recently been identified. The MET gene is found on chromosome 7. It codes for a receptor tyrosine kinase that binds hepatocyte growth factor [23]. Several mechanisms can lead to MET activation, including ligand binding, amplification/overexpression, mutation, or decreased degradation [24].
Recently, the MET exon 14 skipping mutation was shown to identify patients that are potentially responsive to the oral MET inhibitor crizotinib. It is thought that the deletion of the juxtamembrane domain containing the E3-ubiquitin ligase (CBL)-binding site leads to decreased turnover of aberrant MET protein [25]. MET exon 14 skipping-positive patients tend to be older than patients with EGFR- or KRAS-positive lung cancer. Studies showed that 68% of MET exon 14 skipping-positive patients were woman, and approximately one-third were nonsmokers [26].
RET
The RET proto-oncogene is a tyrosine kinase receptor that binds growth factors of the glial-derived neurotrophic factor family. RET rearrangements constitute a molecular subset of NSCLC [27]. Like ALK, there are several fusion partners that have been identified, including KIF5B, coiled-coil domain containing 6 (CCDC6), tripartite-motif containing 33 (TRIM33), and nuclear receptor coactivator 4 (NCOA4) [28]. Approximately 1–2% of adenocarcinomas have RET translocations; however, the frequency is increased in patients who never smoked, especially when EFGR is wild type [29]. RET rearrangements are often observed in patients with an earlier spread to nodal disease and more aggressive tumors.
Treatment
EGFR Inhibitors
There are two primary approaches for targeting EGFR : tyrosine kinase inhibitors (TKIs ) that cross the membrane then bind and inhibit the intracellular tyrosine kinase domain (e.g., erlotinib, gefitinib, afatinib) and monoclonal antibodies that bind the e xtracellular domain and interfere with receptor function and activation. Gefitinib and erlotinib were the first TKIs developed. They are reversible inhibitors that compete with ATP to bind the tyrosine kinase domain of EGFR. Gefitinib was approved by the FDA in 2003 as a monotherapy for the treatment of patients with stage IIIB–IV NSCLC after failure of both platinum-based and docetaxel chemotherapies. Median duration of response was 7.0 months (range, 4.6–18.6 months). Later, a large randomized trial, the ISEL trial, failed to show any survival benefit compared with best supportive care. The median duration of response with gefitinib was 5.6 months compared with 5.1 months for placebo and best supportive care [30]. After approval, gefitinib was studied to evaluate the benefit of adding it to chemotherapy as a first-line treatment for stage IIIB–IV NSCLC [31]. In the INTACT-1 trial, 1093 patients were randomized to placebo, 250 mg gefitinib/day, and 500 mg gefitinib/day combined with up to six cycles of cisplatin and gemcitabine. No differences in objective response rate (ORR), progression-free survival (PFS), or overall survival (OS) were found between the three arms after a median follow-up of 15.9 months. OS was 10.9, 9.9, and 9.9 months for the placebo, 250 mg gefitinib/day, and 500 mg gefitinib/day groups, respectively (p = 0.46).
In 2004, Lynch et al. published a study showing that clinical responsiveness to TKIs was correlated with the presence of activating mutations in the EGFR gene [32]. The same year, the FDA approved erlotinib following a study showing a significant survival benefit with drug administration. The BR21 study investigated the use of erlotinib as a second- or third-line treatment following progression on chemotherapy. The results showed an OS benefit of 6.7 months for the erlotinib group compared with 4.7 months for placebo group (p < 0.001) [33]. In the subsequent TRIBUTE study, erlotinib was studied as a first-line treatment in patients with stage IIIB–IV NSCLC. Participants did not show any improvement in survival or overall response rates. OS was 10.6 months for the erlotinib group compared with 10.5 months for the placebo group [34]. Despite the overall negative findings in this study, erlotinib-treated patients who never smoked, were younger, were female, and had adenocarcinomas had a median survival of 22.5 months compared with 10.1 months for placebo-treated patients who were prior/current smokers. Thus, patients with an EGFR mutation and those who never smoked were identified as patients that could significantly benefit from the treatment with EGFR inhibitors.
To further verify these results, the IPASS study was conducted to compare outcomes of treatment with gefitinib versus that of treatment with carboplatin/paclitaxel [35]. The inclusion criteria were East Asian patients who never smoked or were former light smokers and had stage IIIB–IV lung adenocarcinoma. In the gefitinib arm, there was a PFS benefit at 12 months, with a PFS of 24.9% for the gefitinib arm compared with 6.7% for the carboplatin/paclitaxel arm (p < 0.001). A better ORR was also associated with gefitinib (43% vs. 32.2% for the carboplatin/paclitaxel arm, p < 0.001). Among 437 patients with evaluable EGFR mutation data, 261 had an EGFR mutation. Of these 261 patients, 53.6% had exon 19 deletions, and 42.5% had a missense mutation at exon 21. Among patients with activating EGFR mutations on exon 19 or 21, ORR increased notably in patients who received gefitinib compared with those who received chemotherapy (71.2% vs. 47.3%, respectively, p < 0.001).
In 2015, the FDA approved gefitinib as a first-line therapy for metastatic EGFR-mutated NSCLC based on the IFUM study in which chemotherapy-naïve patients with NSCLC were administered gefitinib. The primary end point of that study was objective response [36]. For patients with exon 19 deletions and exon 21 L858R substitutions, ORRs were 50% and 70%, respectively, and the median duration of response was 6 months and 8.3 months, respectively. The IFUM study results were supported by the IPASS study which randomized East Asian light or never smoker patients between gefitinib and chemotherapy with paclitaxel and carboplatin. That trial showed a PFS benefit with gefitinib treatment. As patients who were initially treated with chemotherapy were allowed to cross over to gefitinib upon progression, no overall survival was demonstrable in the gefitniib group. Similar results were observed for erlotinib as a first-line therapy in EGFR-mutated lung cancer [37]. In 2013, the FDA approved erlotinib as a first-line treatment for cases of metastatic NSCLC with EGFR exon 19 deletions or exon 21 L858R substitutions based on the EURTAC trial. In that study, a PFS of 10.4 months was observed for the erlotinib group compared with 5.2 months for the chemotherapy group (p < 0.001, hazard ratio [HR] 0.34).
The approved dose of gefitinib is 250 mg daily. The most common adverse events include rash (45% of cases), diarrhea (31%), vomiting (13%), and asthenia and dry cough (10%). In rare cases, interstitial lung disease and pneumonitis have been observed. The approved dose of erlotinib is 150 mg daily. The most common adverse events are similar to those of gefitinib.
Afatinib is another FDA-approved first-line therapy for metastatic adenocarcinoma of lung. Afatinib is a TKI that irreversibly binds the intracellular domain of EGFR and Her-2. The approval was based on the LUX-Lung 3 study in which patients were randomized to either the 40 mg afatinib daily arm or chemotherapy arm [38]. The primary end point was PFS. The median PFS for the afatinib arm was 11.1 months compared with 6.9 months for the chemotherapy arm (p < 0.001, HR 0.58). No OS benefit was observed, but there was a difference in ORR (50.4% for the afatinib arm vs. 19.1% for the chemotherapy arm). The most common adverse events were diarrhea (70% of cases), rash (70%), stomatitis (30%), and decreased appetite (25%). Afatinib can also be used as a second-line agent for metastatic squamous cell carcinoma based on the LUX LUNG 8 study. That study showed a 19% improvement in OS and a significant 18% improvement in PFS in the afatinib arm [39].
Despite the initial dramatic response to EGFR inhibitors among patients who harbor EGFR mutations, drug resistance generally develops within 12–18 months. One mechanism of resistance is the development of an EGFR c.2369C > T point mutation (T790 M) that hinders TKI binding and alters ATP handling in approximately 60% of the cases [40, 41]. Secondary resistance can also result from overexpression of c-MET or Her-2. In addition, approximately 5% of patients who experience disease progression after frontline TKIs are used undergo a small-cell transformation. Those transformed cells retain the initial EGFR truncation. Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) mutations and HER2 amplification are additional mechanisms of resistance [42].
The T790 M mutation is rarely detected at diagnosis in cases of lung cancer. Recently, the third-generation TKI osimertinib was approved for patients with EGFR-mutated adenocarcinoma who develop acquired resistance via a T790 M mutation following first-line targeted therapy. The AURA-2 study showed that the ORR was 51% and the median duration of response was 12.4 months for patients with a T790 M mutation who were treated with osimertinib [43]. In that study, common adverse events were diarrhea (42% of cases), rash (41%), dry skin (31%), nail toxicity (25%), eye disorders (18%), and prolonged QTc. (0.2%).
Mok and colleagues published the results of a randomized study of patients with a confirmed T790 M mutation who had cancer progression following first-line TKI therapy. Patients were assigned in a 2:1 ratio to the osimertinib group or the chemotherapy group, which was treated with either a combination of pemetrexed and carboplatin or cisplatin [44]. The median PFS was higher for the osimertinib group (10.1 months vs. 4.4 months for the chemotherapy group, HR, 0.30). The observed response rate was also higher (71% compared with 31% for the chemotherapy group). The percentage of patients with CNS disease who responded to osimertinib was also higher than that of the chemotherapy group (8.5 months vs. 4.2 months, respectively). The toxicity of osimertinib was generally mild with statistically fewer grade III adverse events compared with that of chemotherapy (23% vs. 47%, respectively).
Given the inevitable acquisition of TKI resistance and the clinical need to develop new active agents targeting resistant mutations, it is very important to perform repeated molecular studies of patients. Many patients with advanced lung cancer are willing to undergo repeat biopsies [45]. However, these procedures are invasive, and there is no guarantee that molecular studies will produce a useable result. Approximately 30% of genomic assays fail. This issue has increased the interest in “liquid biopsies .” These tests are advantageous because they are blood- or urine based, are less invasive, and often have a faster turnaround time [46].
Oxnard and colleagues recently compared serum and tissue genotyping of samples acquired from an osimertinib clinical trial [47]. Cell-free serum DNA was assessed and compared with the results of tissue genotyping from a central laboratory. The sensitivity of serum testing was 70%. Among 58 patients who were negative for T790 M based on tissue genotyping, 31% had detectable T790 M mutations upon serum genotyping. The ORRs were similar regardless of whether the T790 M was detected in tissue or blood (62% vs. 63%, respectively). Further validation is needed; however, the success of this cell-free assay suggests that it could be used as an initial test once radiographic progression has been documented. This evaluation scheme would allow clinicians to limit invasive biopsies to those patients with negative cell-free assay results. At this time, there is insufficient evidence to recommend serum monitoring for patients with oncogene-addicted lung cancers in a manner similar to that of patients with chronic myeloid leukemia.
In contrast to EGFR TKIs, the effect of anti-EGFR monoclonal antibodies is not directly associated with any EGFR mutations. Two phase III clinical trials investigating anti-EGFR monoclonal antibodies have been performed. The BMS099 trial randomly assigned patients into two groups: carboplatin/paclitaxel with cetuximab and carboplatin/paclitaxel without cetuximab. In this trial, no significant OS benefit was observed (9.7 months for the with cetuximab group vs. 8.4 months for the without cetuximab group, p = 0.17). The FLEX trial investigated the administration of cisplatin/vinorelbine with or without cetuximab in patients who were EGFR mutation positive. A significant difference in OS benefit was observed in the with cetuximab group compared with the without cetuximab group (11.3 months vs. 10.1 months, respectively, p = 0.04) [48]. It is unclear whether the different results seen in these trials were related to inclusion criteria or chemotherapy regimen. Another anti-EGFR antibody, necitumumab, showed modest activity in cases of stage IV squamous cell carcinoma. In the randomized SQUIRE trial, patients were administered cisplatin/gemcitabine either with or without necitumumab. There was a modest improvement in OS (11.5 months vs. 9.9 months in the with and without necitumumab groups, respectively; HR 0.84; p = 0.012) and PFS (HR 0.85, p = 0.02). No difference in ORR was observed (31% vs. 29%) in the with and without necitumumab groups, respectively; p = 0.4) [49]. The most common adverse events with cetuximab are infusion reactions (3% of cases), dermatologic toxicity (3%), fever (5%), and diarrhea (6%).
ALK and ROS1 Inhibitors
Crizotinib is a first-generation oral small-molecule inhibitor targeting ALK, ROS, and MET tyrosine kinases. In 2011, the FDA approved crizotinib for ALK-mutated adenocarcinoma of the lung. Crizotinib showed an approximately 60% ORR response rate in phase I and phase II trials [50]. These results were confirmed by the PROFILE 1007 trial investigating crizotinib as a second-line therapy for patients with ALK-positive NSCLC. This phase III trial showed significantly higher response rates for the crizotinib group compared with the chemotherapy group (65% vs. 29%, respectively). There was also significant improvement in PFS (7.7 months vs. 3 months for the crizotinib group and chemotherapy group, respectively, p < 0.001) [51]. Moreover, crizotinib was shown to be superior to standard platinum/pemetrexed chemotherapy in the PROFILE 1014 trial in which patients were treated with chemotherapy or crizotinib [52]. In that study, the ORR of the crizotinib arm was 74% compared with 45% for the chemotherapy arm. In addition, PFS was significantly improved in the crizotinib arm compared with the chemotherapy arm (10.9 months vs. 7 months, respectively; p < 0.001; HR 0.45). The most common adverse events with crizotinib are visual disturbances (60% of cases), diarrhea (60%), nausea and vomiting (50%), and constipation (40%).
Similar to EGFR TKI therapies, the dramatic treatment response is not sustained due to the development of drug resistance. The resistance mechanism can be ALK dependent (e.g., the development of the L1196M gatekeeper or C1156Y mutation, an increase in the number of ALK fusion copies) or ALK independent (e.g., through the activation of other bypass agents such as EGFR and KRAS) [53]. In addition, recent studies indicate that the spectrum of secondary mutations varies depending on the TKI used. For example, the ALK G1202R mutation is more commonly observed following therapy with a second-generation ALK inhibitor [54]. Thus, repeated sampling of a patient’s genetic markers as they progress through various therapies will allow us to better understand the mechanisms underlying resistance and improve treatment planning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree