Fig. 12.1
EORTC QLQ-H&N 35 multi-item symptom scale score: mean change from baseline to worst post-baseline score [69]
Table 12.1
Percentage of risk reduction on overall survival for chemoradiotherapy compared with radiotherapy. (a) All patients in EORTC and RTOG trials; (b) subset analyses in patients eligible for both trials or one trial only
Number | Risk reduction for CRT (%) | Probability | |
|---|---|---|---|
EORTC | 334 | 30 | 0.04 |
ROG | 416 | 16 | 0.19 |
Combined | 750 | 28 | <0.05 |
Number | Risk reduction for CRT (%) | Probability | |
(Eligible for both studies) | |||
EORTC | 233 | 33 | Not described |
RTOG | 246 | 30 | Not described |
Combined | 479 | 26 | Not described |
(Eligible for only one study) | |||
EORTC | 101 | 25 | 0.06 |
RTOG | 170 | 6 | 0.73 |
At the American Society of Clinical Oncology (ASCO) meeting of 2006, Fietkau et al. presented the results of the phase III part (ARO 96–3), which compared two postoperative adjuvant treatments, radiation monotherapy and 5-FU plus cisplatin CRT [8]. This study targeted 440 patients with postoperative risk factors for recurrence for head and neck squamous cell carcinoma (microscopic resection margin positivity, extracapsular nodal extension positivity, or multiple cervical lymph node metastasis [≥3]). Five-year DFS rate in the radiation monotherapy and CRT groups was 50 % versus 62 %, respectively (P = 0.023), showing the statistically significant superiority of CRT, whereas 5-year OS rate was 49 % versus 58 %, respectively, showing no significant difference. These results failed to demonstrate the usefulness of postoperative 5-FU plus cisplatin CRT.
In 2008, Argiris et al. [9] reported the results of a phase III study of postoperative adjuvant treatment which compared radiation monotherapy and CRT using carboplatin in 72 patients with postoperative risk factors for recurrence (microscopic resection margin positivity, extracapsular nodal extension positivity, perineural infiltration, or signs of vascular infiltration) for SCCHN. In this study, the CRT group showed no superiority to the radiation monotherapy group in either 5-year DFS rate or 5-year OS rate, and thus the usefulness of postoperative CRT with carboplatin was not demonstrated.
Although no major meta-analysis of postoperative CRT has appeared, a meta-analysis of the above four phase III studies by Bachaud, Smid, Bernier, and Cooper and their colleagues demonstrated that CRT significantly contributes to survival compared with radiation monotherapy (relative risk, 0.80; 95 %CI, 0.71–0.90; P = 0.0002) [10].
Based on the above results, CRT has been the standard postoperative adjuvant treatment for patients with postoperative high-risk relapse factors (microscopic resection margin positivity or extracapsular nodal extension positivity) for locally advanced SCCHN in Europe and the USA. Cisplatin 100 mg/m2 every 3 weeks, as used in the EORTC22931 and RTOG95-01 studies, is believed to be the most commonly used standard regimen for concurrent monotherapy [5, 7, 10, 6].
12.3 Postoperative Adjuvant Chemotherapy
Although the role of postoperative adjuvant chemotherapy remains unclear, it is widely used in Japan. UFT was investigated in a randomized trial as adjuvant therapy after radical treatment of SCCHN in Japan [11]. Patients were randomly assigned to a UFT group or non-treatment group. The following three categories were included: (1) stages II–IV, receiving radical surgery (n = 424); (2) stage II, receiving radical radiotherapy (n = 111); and (3) nasopharyngeal cancer (n = 25). In patients undergoing radical surgery, no significant difference was observed in 3-year overall survival (77.9 % for the UFT group vs. 72.9 % for the non-treatment group) or 3-year relapse-free survival (73.4 % vs. 66.2 %) between the two groups. In the patients receiving radical radiotherapy, furthermore, no significant difference was observed in either 3-year OS rate or 3-year relapse-free rate.
Recently, the results of a randomized phase III trial comparing S-1 with UFT as adjuvant chemotherapy after completion of definitive therapy for stages III–IVB SCCHN (ACTS-HC) were reported at the annual ASCO meeting of 2013 [12]. A total of 526 patients were enrolled and randomly assigned to UFT (n = 262) or S-1 (n = 264). Definitive therapy included surgery with or without adjuvant therapy, including radiotherapy or concurrent CRT (n = 149 in the UFT group, n = 151 in the S-1 group) and definitive radiotherapy or CRT with or without salvage surgery (n = 105 in the UFT group, n = 100 in the S-1 group). No significant difference was seen in DFS, the primary end point (3-year DFS: 60 % in the UFT group vs. 64.1 % in the S-1 group, HR 0.87; 95 % CI 0.66–1.16; p = 0.34), whereas a significant difference was seen in OS (3-year OS: 75.8 % in the UFT group vs. 82.9 % in the S-1 group, HR 0.87; 95 %CI 0.44–0.94; p = 0.022). Grade 3 or 4 toxicities were significantly more frequent in the S-1 group, including mucositis or stomatitis (2.4 % vs. 0 %), hyperpigmentation (3.6 % vs. 0 %), leukopenia (5.2 % vs. 0.8 %), neutropenia (3.6 % vs. 0 %), and thrombocytopenia (2.0 % vs. 0 %). Although S-1 was superior to UFT in terms of 3-year OS, this trial could not establish a role for adjuvant chemotherapy for a number of reasons: first, the choice of UFT as control arm was criticized because UFT did not demonstrate survival benefits compared with placebo in a previous study; second, the absence of a difference in DFS made it difficult to explain the improvement in OS; and third, subjects were not limited to patients with high-risk SCCHN, resulting in markedly prognoses in both groups than in previous trials of adjuvant therapy. In other words, there is concern that this study included patients who do not require adjuvant therapy.
12.4 Preoperative Concurrent Chemoradiotherapy
Combinations of surgery and radiotherapy with or without chemotherapy are used pre- or postoperatively [13], but there is no consensus regarding the sequence of surgery, radiotherapy, and/or chemotherapy for resectable advanced OSCC. The controversy about pre- or postoperative chemoradiotherapy continues for adjuvant therapy. However, in general, it is clear that radiotherapy and chemotherapy are more effective in unaffected and well-oxygenated tissue where the regional vasculature is intact, less hypoxic regions exist, and the drug delivery to the tumor may be better.
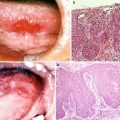
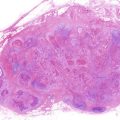
Preoperative concurrent chemoradiotherapy has been recently reported to be effective in advanced cases although the cases of postoperative radiotherapy or chemoradiotherapy outnumber those of preoperative concepts. These reports demonstrate that this approach is feasible with tolerable adverse events and that a high rate of completion of treatment regimen results in promising overall and disease-free survival rates [14–18]. Klug et al. [17] reviewed the survival data of 1,927 patients from 32 publications in the literature using a meta-analysis of preoperative CRT and radical surgery for advanced OSCC and SCC of the head and neck. They reanalyzed some reports and demonstrated that the mean 5-year survival rate was 62.6 % (58.4–66.8 %). This appears to be remarkably good when compared with the prospective randomized RTOG [6] and EORTC [5] studies with postoperative CRT (50 % and 53 %, respectively). Kirita et al. [19] also reported that the preoperative CRT followed by surgery for resectable advanced OSCC produced high clinical and histopathologic complete response and survival rates. In their study, the 5-year overall and progression-free survival rates were 87.1 % and 90.3 % for stage III patients and 70.0 % and 71.6 % for stage IV patients in all 154 patients. They also showed that the pathological CR in the primary tumors was seen in 89.1 % in the patients with CR (complete response) and in 73.1 % in the patients with good PR (partial response) and that 90.2 % of CR and 73.1 % of good PR patients have no residual tumor cells or viable tumor cells remained only within the central submucosa or shallow in the muscularis propria (central superficial portion). In the CR patients in the neck, pN + rate was 10.3 %, which was very low, and pathologically positive lymph nodes were only seen in levels IB (7.7 %) and IIA (7.7 %). In the PR and SD patients in the neck, pN + rate was 44.6 %, which was higher than that of the CR patients; pathologically positive lymph nodes were seen widely in several levels, especially in levels IB, IIA, and IIB.
Therefore, it is considered that even in advanced oral cancers, it could be possible to avoid extended resection and perform minimally invasive surgery in which the extent of resection on primary tumor and neck is reduced to preserve morphology and function in patients who achieve good response (CR and good PR in the primary tumor, CR in the neck) following preoperative CRT [19].
It is thought that the advantages of preoperative CRT followed by surgery for advanced but resectable OSCC patients are as follows. This treatment approach will produce better locoregional control rate and survival than postoperative CRT [20] and contribute to organ-function preservation with minimally invasive surgery, that is, less invasive surgery in the primary tumor and selective neck dissection for residual neck disease. Other advantages of this approach with a lower radiation dose would give better quality of life and reduce the critical complication of osteoradionecrosis. There is no evidence of a significantly higher rate of postoperative morbidity and more frequent occurrence of local complications such as wound infection, free flap failure, and prolonged duration of hospitalization from this treatment approach [15]. In case dental implants are used in OSCC patients for functional reconstruction, a lower radiation dose (<50 Gy) is reported to be significantly associated with improved implant survival compared with higher doses (>50 Gy), and no failures were observed with radiation doses <45 Gy [21].
12.5 Concurrent Chemoradiotherapy as Primary Treatment or Salvage Treatment
CRT for OSCC has been conducted either as primary treatment for patients who are unable to tolerate or who are unsuited for surgery or as salvage treatment in the persistent or recurrent disease setting.
A retrospective review of patients from four multi-institutional phase II studies with T4 OSCC aimed at evaluating long-term toxicity, locoregional control (LC), PFS, and OS of primary CRT [22] and identified 39 subjects, 16 (42 %) of whom had bony involvement. All regimens utilized concomitant 5-fluorouracil, hydroxyurea, and radiotherapy (FHX)-based regimens and added a third agent (cisplatin, paclitaxel continuous infusion, or paclitaxel 1-h infusion). Median radiotherapy dose delivered to the primary tumor was 74 Gy. Five-year OS, PFS, and LC rates were 56 %, 51 %, and 75 %, respectively. Sixty-nine percent of subjects with bony involvement never relapsed. Seven subjects developed osteoradionecrosis. Bone involvement with the primary tumor did not appear to be associated with an increased risk of death, relapse, or long-term complications. These data suggest that primary CRT is an effective treatment approach in patients with T4 OC tumors, including those with bone involvement. However, this study had several limitations, including its retrospective design and no control group for comparison; limited power of analysis due to a relatively small population; and specific subjects who were on a protocol with specific eligibility requirements. The results could not therefore be generalized into clinical practice, and further investigation is warranted.
In a meta-analysis of individual patient data from clinical trials comparing radiotherapy versus CRT (MACH-NC) in locally advanced head and neck cancers, OSCC accounted for 21 % of cases [23]. Result showed that CRT provided better survival than radiotherapy alone in OSCC (HR = 0.8). The results of his meta-analysis appear to suggest that concurrent chemotherapy may be a treatment option in patients unable to receive primary surgery.
Recently, numerous molecular targeted drug s have been investigated for cancer treatment, including head and neck cancer. Epidermal growth factor receptor (EGFR ) has emerged as a promising target for cancer therapy. EGFR is a tyrosine kinase receptor of the ErbB family that is highly expressed and/or abnormally activated in many epithelial tumors, including SCCHN, colorectal cancer, and non-small-cell lung cancer [24–26]. EGFR ligand binding stimulates multiple cellular functions essential to tumor growth, including invasiveness, cell damage repair, and angiogenesis. EGFR expression in tumors is usually associated with more aggressive disease, increased resistance to chemotherapy and radiotherapy, increased metastasis, poor prognosis, and decreased survival [27, 28]. EGFR overexpression has been reported in more than 80 % of cases of SCCHN, and multivariate analyses have shown EGFR levels to be an independent predictor of a poor outcome in SCCHN [29].
Cetuximab , a chimeric monoclonal antibody that binds to the extracellular domain of EGFR [30], has shown both in vitro [31] and in vivo activity against SCCHN-derived cells and tumors [32]. Importantly, cetuximab has been shown to enhance the antitumor activity of radiotherapy [32, 33].
Bonner et al. conducted a multinational, randomized study to compare radiotherapy alone with radiotherapy plus cetuximab for locally advanced SCCHN, including in the larynx, hypopharynx, and oropharynx [34]. A total of 424 patients were randomly assigned to treatment with radiotherapy alone (213 patients) or radiotherapy plus weekly cetuximab (211 patients) at an initial dose of 400 mg/m2, followed by 250 mg/m2 weekly for the duration of radiotherapy. The addition of cetuximab to radiotherapy demonstrated a significant improvement in locoregional control (24.4 months in the cetuximab group vs. 14.9 months in the radiotherapy alone group, HR for locoregional progression or death, 0.68; P = 0.005), progression-free survival (17.1 months vs. 12.4 months, HR for disease progression or death, 0.70; P = 0.006), and overall survival (49.0 months vs. 29.3 months, HR for death, 0.74; P = 0.03). Based on this result, cetuximab plus radiotherapy is superior to radiotherapy alone in increasing both the duration of locoregional disease control and survival in locoregionally advanced SCCHN. None of the subjects in this trial had OSCC, and the role of cetuximab in combination with radiotherapy for OSCC therefore remains unclear.
12.6 Neoadjuvant Chemotherapy
The role of neoadjuvant chemotherapy prior to surgery remains controversial. In a randomized study of neoadjuvant chemotherapy with cisplatin and fluorouracil (PF) followed by surgery compared with surgery in OSCC [35], 195 patients with resectable, stage T2–T4 (>3 cm), N0–N2, M0 untreated, squamous cell carcinoma of the oral cavity were randomly assigned to three cycles of PF followed by surgery (chemotherapy arm) or surgery alone (control arm). In both arms, postoperative radiotherapy was reserved for high-risk patients. Postoperative radiotherapy was administered to 33 % of patients in the chemotherapy arm versus 46 % in the control arm. Mandible resection was performed in 52 % of patients in the control arm versus 31 % in the chemotherapy arm. In the chemotherapy arm, three toxic deaths were recorded. Five-year OS was 55 % for both arms, indicating that the addition of neoadjuvant chemotherapy with PF to standard surgery was unable to improve survival.
However, primary chemotherapy appeared to play a role in reducing the number of patients in this study who required mandibulectomy, radiation therapy, or both. Variations in the criteria used to select patients for these treatment options may hamper generalization of these results, but there appears to be room to use preoperative chemotherapy to spare destructive surgery or radiation therapy in patients with advanced, resectable oral cavity cancer.
Novel induction chemotherapy regimens which add docetaxel to PF (TPF) have shown promising results in two recent phase III trials (TAX323 and TAX324) in the setting of nonsurgical treatment of locally advanced SCCHN [26, 37, 38]. In both studies, patients were randomly assigned to receive PF versus TPF before radiotherapy (TAX323) or CRT (TAX324). Results showed a statistically significant improvement in OS in patients randomly assigned to the TPF arm, and TPF is accordingly suggested as the preferred combination chemotherapy regimen when induction treatment is used for nonsurgical management of patients with SCCHN. However, the potential benefits of TPF induction have recently been questioned: the DeCIDE and PARADIGM trials compared up-front chemoradiotherapy with TPF induction followed by CRT and failed to demonstrate a significant improvement in OS or disease-free survival (DFS) with TPF [39, 40]
Further, a recent randomized trial of neoadjuvant chemotherapy with TPF versus up-front surgery in patients with OSCC also failed to demonstrate a significant improvement in OS or DFS with TPF [41]. In this study, 256 patients with stage III or IVA locally advanced resectable OSCC were randomly assigned to two cycles of TPF followed by surgery and postoperative RT (54–66 Gy) or up-front surgery and postoperative RT. TPF consisted of two cycles of docetaxel 75 mg/m2 on day 1, cisplatin 75 mg/m2 on day 1, and 5-FU 750 mg/m2 on days 1–5, repeated every 3 weeks. The clinical response rate to TPF was 80.6 %. TPF did not increase perioperative morbidity. After a median follow-up of 30 months, however, no significant difference was seen in either OS (HR 0.977; 95 % CI, 0.634–1.507; p = 0.918) or DFS (HR 0.974; 95 % CI, 0.654–1.45; p = 0.897).
Together, these findings suggest that neoadjuvant chemotherapy should not be recommended for clinical use in locally advanced OSCC.
12.7 Palliative Chemotherapy for Recurrent and/or Metastatic Setting
Despite aggressive surgery with or without adjuvant therapy, or multidisciplinary approaches, approximately 50 % of patients will develop incurable locoregional or distant recurrence. In this setting, chemotherapy is one treatment option. Because the prognosis of patients with recurrent and/or metastatic head and neck cancer is generally poor, the therapeutic goal is to extend survival without worsening quality of life.
The most common chemotherapy drugs used for advanced SCCHN include taxanes (paclitaxel and docetaxel), anthracyclines (adriamycin, epirubicin, and pirarubicin), platinums (cisplatin and carboplatin), and antimetabolites (e.g., methotrexate and 5-fluorouracil). However, no prospective clinical trial of chemotherapy drugs for recurrent or metastatic OSCC patients only has been conducted. Approximately 20–30 % of patients with recurrent or metastatic SCCHN who have enrolled in clinical trials to date had OSCC.
Cisplatin remains one of the most widely used standard agents in the recurrent and/or metastatic setting, with an average single-agent response rate of 28 %. Most single-agent studies have employed doses of 80–120 mg/m2 administered as an intravenous bolus every 3–4 weeks. A small randomized trial compared cisplatin given as a single bolus of 120 mg/m2 with 20 mg/m2/day for 5 days, repeated every 3 weeks. In this study, antitumor activity was comparable between the two arms. Veronesi et al. [42] conducted a small randomized trial comparing 120 mg/m2 versus 60 mg/m2 of cisplatin administered as a bolus. Of 62 eligible patients, 59 were evaluable, with response rates in patients receiving high- and low-dose cisplatin of 16.1 % and 17.8 %, respectively. Median OS was 34 weeks, and survival in the two treatment arms was superimposable. These studies provided no evidence of dose dependency of cisplatin activity in advanced SCCHN.
Morton et al. [43] conducted a small randomized trial of cisplatin and bleomycin using a 2 × 2 factorial design for patients with recurrent or metastatic SCCHN. Of 116 enrolled patients, 30 % proved to be unfit for chemotherapy. Cisplatin significantly prolonged median survival by 10 weeks. This trial led to the widespread use of cisplatin alone.
Carboplatin is a second-generation platinum analog with a similar spectrum of activity against a number of solid tumors as cisplatin. Phase II studies of single-agent carboplatin have demonstrated a response rate of 20–26 % [44–47]. Although carboplatin is often considered to be less effective than cisplatin in SCCHN, little direct comparison has been done. In a Southwest Oncology Group (SWOG) study, 277 patients were randomly assigned to receive either cisplatin plus 5-FU, carboplatin plus 5-FU, or single-agent methotrexate [48]. Although no formal statistical comparison of cisplatin and carboplatin was performed, response rate was higher in the cisplatin arm than the carboplatin arm (32 % vs. 21 %), while median survival in these two arms was similar. Carboplatin may be preferred in some patients since it is associated with less neurotoxicity, nephrotoxicity, and nausea and vomiting than cisplatin, although it does cause more myelosuppression.
Docetaxel is a semisynthetic taxane analog that also possesses significant activity in SCCHN. Several single-agent phase II studies in chemotherapy-naïve patients with recurrent or metastatic SCCHN yielded response rate of 21–42 % [49–52]. Guardiola et al. [53] reported the results of a randomized phase II study which compared docetaxel with methotrexate in patients with recurrent SCCHN. Response rate was significantly higher in the docetaxel arm, with an objective response rate of 27 % vs. 15 % in the methotrexate arm. In contrast, no significant differences were seen between the arms in either OS or time to progression. Inuyama at al. employed a lower dose of docetaxel (60 mg/m2, every 3–4 weeks). Response rate was 22 % in 59 evaluable patients and 17.4 % in 46 patients who received prior chemotherapy.
Paclitaxel is a diterpene plant-derived product that exerts cytotoxic effects by promoting microtubule assembly, ultimately leading to the disruption of mitosis and cell death. Single-agent activity for recurrent or metastatic SCCHN in phase II trials demonstrated an encouraging response rate range of 20–40 %. Previous studies of high-dose tri-weekly paclitaxel (200–250 mg/m2) in patients with advanced or recurrent/metastatic SCCHN demonstrated an overall response of 35–40 %, which was associated with severe neuropathy and myelosuppression [54, 55]. A prospective phase II study of weekly paclitaxel for recurrent or metastatic head and neck cancer that paclitaxel showed acceptable toxicity but a poor response rate of 9.3 % (4/43) [56]. Japanese phase II trials, including an early and late phase II trial of weekly paclitaxel in patients with recurrent or metastatic head and neck cancer [57], enrolled a total of 74 patients. Overall response rate was 29.0 % according to RECIST. The median duration of response, median time to progression, and median survival time were 7.4 months, 3.4 months, and 14.3 months, respectively. Together, these findings suggested that weekly paclitaxel has promising activity with acceptable toxicity in recurrent or metastatic head and neck cancer.
Numerous trials have compared various combinations of cytotoxic agents in patients with recurrent or metastatic SCCHN. One of the most widely used regimens is the combination of cisplatin plus 5-FU, with a response rate of approximately 30 % in this setting. Several phase III trials demonstrated a higher response rate but no significant prolongation of survival compared with single agents, including cisplatin and methotrexate [48, 58] (Table 12.2). The combination of cisplatin plus 5-FU has higher toxicity than the single agents alone, particularly in patients with a poor performance status or serious comorbidity, and any use of combination chemotherapy requires careful selection of both agents and patients.
Table 12.2
Randomized trials of chemotherapy for recurrence or metastatic SCCHN
Author | Treatment | Number of patients | Response rate (%) | MST (months) |
|---|---|---|---|---|
Morton et al. [43] | CDDP + bleomycin | 116 | 13 | 4 |
Bleomycin | 14 | 2.8 | ||
CDDP | 24 | 4.2a | ||
No therapy | 0 | 2.1 | ||
Forastiere et al. [48] | CDDP + 5-FU | 87 | 32 | 6.6 |
CBDCA + 5-FU | 86 | 21 | 5.0 | |
MTX | 88 | 10 | 5.6 | |
Jacobs et al. [58] | CDDP + 5-FU | 79 | 32a | 5.5 |
CDDP | 83 | 17 | 5.0 | |
5-FU | 83 | 13 | 6.1 | |
Gibson et al. [84] | CDDP + 5-FU | 104 | 41.4 | 8.7 |
CDDP + paclitaxel | 100 | 32.4 | 8.1 |
Over the past decade, the combination of platinum plus a taxane analog, including paclitaxel and docetaxel, has demonstrated significant activity in recurrent or metastatic SCCHN. Several phase II trials of cisplatin plus paclitaxel yielded a response rate of 32–48 %. A randomized phase III trial of cisplatin plus 5-FU versus cisplatin plus paclitaxel, conducted as an intergroup trial of the ECOG and SWOG, reported no significant difference in response rate, survival, or quality of life measures (Table 12.2). Nevertheless, there is concern that the addition of paclitaxel to cisplatin increases the incidence and severity of neuropathy and combination treatment with carboplatin plus paclitaxel is now widely used.
Combination treatment with docetaxel plus cisplatin has also been investigated. Phase II studies in recurrent or metastatic SCCHN yielded response rates of 33–50 % with acceptable toxicity. These finding support the use of platinum plus taxane as a reasonable treatment option.
Molecular targeted drugs have been also investigated for recurrent or metastatic SCCHN. Cetuximab has been shown to enhance the antitumor activity of cisplatin [59] without any effect on its pharmacokinetic profile [60]. One of the most interesting aspects of cetuximab is that it appears to reverse tumor resistance to chemotherapy, such that the tumor again responds to therapy under which it previously progressed. This effect was initially noted in nonclinical studies with cetuximab plus irinotecan in irinotecan-refractory colorectal xenografts [61] and was subsequently confirmed in the clinical setting [62], leading many countries to approve the use of cetuximab in combination with irinotecan in patients with EGFR-expressing metastatic colorectal cancer that progressed on irinotecan-containing therapy.
A phase IB study in patients with SCCHN demonstrated that the combination of cetuximab and cisplatin was active, even in a subset of patients who had been previously treated with cisplatin and had documented cisplatin resistance [63]. In patients with platinum-refractory recurrent and metastatic SCCHN, a combination of cetuximab plus cisplatin or carboplatin demonstrated response rates of 6–20 % in two phase II studies [64, 65], whereas single-agent cetuximab produced a major objective response rate of 13 % in a phase II study [66] (Table 12.3). These findings indicate that there is no clear evidence that cetuximab reverses platinum resistance in SCCHN.
Table 12.3




Clinical trials of cetuximab for recurrent or metastatic SCCHN
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree