Hormones
Precursor/activator
Products
Amines
Tryptophan
Serotonin
5-Hydroxytryptophan
5-HIAA
Histidine
Histamine
Peptides
Kallikrein
Bradykinin
Kallidin
Tachykinins
Substance P
Neurokinin A
Neurokinin B
Neuropeptide K
Hemokinin-1
–
Motilin
ACTH
Chromogranin A
Prostaglandins
PGE synthase
Prostaglandins E
PGF synthase
Prostaglandins F
The early symptoms of carcinoid tumor are nonspecific and may include abdominal pain, diarrhea, intermittent intestinal obstruction, and gastrointestinal bleeding. These often vague and generalized signs and symptoms produce a delay in diagnosis in many patients. Although symptoms may be caused by mechanical effects of the tumors, symptoms of carcinoid tumors are also caused by the effects of amine and neuropeptide substances secreted into the gastrointestinal tract or the systemic circulation [1]. The effects of these chemicals, collectively referred to as the carcinoid syndrome , are diverse and include cutaneous flushing, diarrhea, carcinoid heart disease, bronchoconstriction, hypotension, hypertension, and pellagra (Fig. 1) [1].
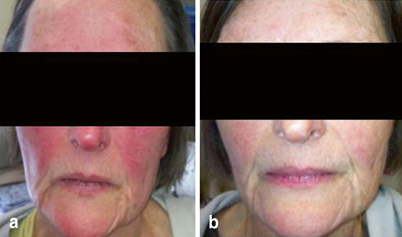
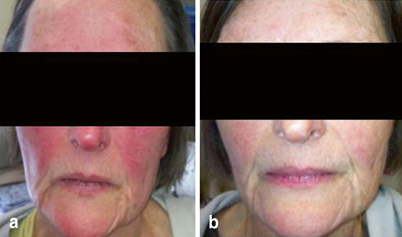
Fig. 1
A 62-year-old woman with carcinoid syndrome-related flushing, elevated urinary 5-HIAA, and an unknown primary. The image shows flushing in the patient before octreotide therapy (a) and after octreotide therapy (b)
The classic carcinoid syndrome does not develop until a tumor has metastasized to the liver and or lung, and the hormonal products released by the tumor reach the central venous circulation in substantial concentrations [5]. Some patients with functioning gastric or bronchial carcinoids have clinical and biochemical variations from the classic syndrome [6].
Epidemiology
The incidence of classical carcinoid syndrome , which is characterized by flushing, diarrhea, abdominal cramping, and, less often, wheezing, heart-valve dysfunction, and pellagra, varies depending on the study population. While studies that include patients with localized and incidental tumors report the frequency of carcinoid syndrome to be about 10–18 %, the prevalence may be as high as 50 % among patients with advanced and metastatic disease [7–11]. The syndrome results from synergistic interactions between biochemical substances secreted by the tumor, and it is often observed in patients with metastatic disease or when the primary tumor site allows the secreted amines to escape enteral hepatic circulation The presence of carcinoid syndrome is associated with poor survival [10].
Biochemistry of Carcinoid Syndrome
In 1954, Pernow and Waldenstrom demonstrated the presence of serotonin in the blood and urine of two patients with carcinoid tumor during an attack of flushing [12]. Originally, the whole spectrum of symptoms was related to the production and secretion of serotonin by the tumor and its metastases [5, 12]; however, since that time, a number of hormonal substances contributing to the signs and symptoms of carcinoid syndrome have been described, and the syndrome itself has been more fully characterized [8].
Carcinoid tumors produce and secrete a great variety of bioactive compounds, including serotonin, histamine, bradykinin, tachykinin, motilin, substance P, kallikrein, prostaglandins, catecholamines, and in some cases adrenocorticotropic hormone [1, 10, 13]. Although the contribution of each of these mediators is not yet completely understood, some of them including serotonin , histamine, tachykinins, and kallikrein are thought to play a major role in the development of the clinical picture of carcinoid syndrome .
Tryptophan and Serotonin
Tryptophan is an essential amino acid, and, therefore, must be obtained from the diet. In healthy people, as much as 99 % of dietary tryptophan is metabolized by the oxidative pathway into nicotinic acid, and 1 % or less is converted into 5-hydroxytryptophane [7, 10, 14]. In carcinoid tumors , however, a disequilibrium of tryptophan metabolism has been hypothesized whereby as much as 60–70 % of the body’s tryptophan may be shunted to 5-hydroxylation and production of 5-hydroxytryptophane instead of nicotinic acid (Fig. 2) [7, 15]. This is the most constant biochemical feature of carcinoid tumors.
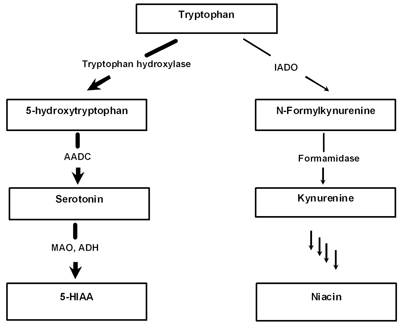
Fig. 2
Tryptophan metabolism in carcinoid tumors. Thick lines depict predominant tryptophan metabolic pathway in carcinoid tumors. AADC aromatic amino acid decarboxylase, MAO monoamine oxidase, ADH aldehyde dehydrogenase, 5-HIAA 5-hydroxyindoleacetic acid, IADO Indoleamine-2,3-dioxygenase
The typical midgut carcinoid tumors also contain aromatic amino acid decarboxylase (AADC), which catalyzes the conversion of 5-hydroxytryptophane to 5-hydroxytryptamine (serotonin) (Fig. 2). Hindgut and foregut tumors such as gastric carcinoids, however, are frequently deficient in this enzyme and release 5-hydroxytryptophane instead of serotonin. Following its release into the portal circulation, almost all circulating serotonin is rapidly metabolized by the liver enzymes monoamine oxidase and aldehyde dehydrogenase and converted into the respective inactive metabolites 5-hydroxyindoleacetaldehyde and 5-hydroxyindoleacetic acid (5-HIAA) . 5-HIAA is excreted into the urine as urinary 5-HIAA, which can be used as a biomarker of the tumor activity. Although in smaller amounts, removal of serotonin from the bloodstream can also be mediated by its active uptake in the platelets.
5-Hydroxyindoleacetic Acid
5-HIAA is the end product of serotonin metabolism (Fig. 2) . The measurement of 24-h urinary excretion in patients suspected to have carcinoid syndrome is a useful initial diagnostic test with a sensitivity and specificity of over 90 % [16, 17]. However, certain drugs and tryptophan/serotonin-rich foods can lead to false positive results, and these foods should be avoided for at least 24 h prior to urine collection [18]. While the test is generally most useful in patients with midgut carcinoid tumors , its sensitivity could be lower in patients with carcinoid tumors without carcinoid syndrome [16]. The normal rate of 5-HIAA excretion ranges from 2 to 8 mg/day (10–42 µmol/day). Patients with carcinoid syndrome may have variable 5-HIAA urinary levels ranging from mildly elevated (30 mg/day) to more than 2000 mg/day [17] .
Tachykinins
The peptides of the tachykinin family are one of the largest families of neuropeptides many of which are present in normal enterochromaffin cells of the gastrointestinal tract and in many neuroendocrine tumors including carcinoid tumors [11, 19–23]. Among the members of the tachykinin family are substance P, neurokinin A and B, neuropeptide K, and hemokinin-1 [24, 25]. Tachykinins have been shown to possess a number of biological activities, including smooth-muscle contraction, vasodilatation, pain transmission, activation of the immune system, and stimulation of endocrine gland secretion [20, 26].
Histamine
Although primary gastric carcinoids are frequently deficient in the enzyme AADC and lack the ability to produce serotonin, they overexpress the enzyme histidine decarboxylase, which converts the essential amino acid histidine into histamine [27]. Histamine has been suggested to be the primary causative agent for the atypical flushing and pruritus associated with these tumors [28]. This hypothesis was supported by the observation that administration of histidine markedly increased the frequency, severity, and duration of flushing [29]. In addition, this flushing can be ameliorated by combined H1 and H2 antagonists [30]. Healthy people excrete normally < 20 μg of histamine per 24 h, while patents with gastric carcinoid syndrome may excrete > 200 μg per 24 h [30].
Kallikrein and Prostaglandins
Series of investigations have implicated the kallikrein–kinin system in the pathogenesis of carcinoid syndrome [28, 29, 31]. Kallikrein is a protease that cleaves kininogens to form kinins (bradykinin and kallidin) plasma proteins that are further converted into vasoactive peptides. It has been shown that some carcinoid tumors contain kallikrein, and the hepatic venous blood draining carcinoid liver metastases contains bradykinin [28, 29]. Bradykinin is one of the most potent vasodilators known and may be responsible for flushing in some carcinoid patients [29]. Kinins also stimulate intestinal motility and increase vascular permeability [28].
It has been suggested that prostaglandins E and F stimulate intestinal motility and fluid secretion in the normal gastrointestinal tract [32–34]. Elevated serum prostaglandin concentrations have been found in patients with the carcinoid syndrome, suggesting that these compounds may also play a role in some aspects of the carcinoid syndrome. However, there is no direct evidence to support this hypothesis and their role in the constellation of symptoms that are present in carcinoid syndrome is uncertain [35].
Clinical Presentation of Classical Carcinoid Syndrome
Carcinoid syndrome is generally characterized by flushing, diarrhea, and, less commonly, wheezing, heart-valve dysfunction, and pellagra (Table 2) [1, 10, 23, 36]. The frequency of carcinoid syndrome correlates with the extent of the metastatic carcinoid disease, and it can be as low as 10 % in localized cases, but can occur in 40–50 % of patients with more advanced disease [7–11, 37]. The presence of carcinoid syndrome is associated with poor survival [10].
Table 2
Common symptoms in patients with the carcinoid syndrome: frequency and association with secreted compounds
Symptoms | Putative substances | Frequency (%) | References |
|---|---|---|---|
Flushing | Histamine, tachykinins, kallikrein, bradykinin | > 90 | |
Diarrhea | Serotonin, substance P, motilin, prostaglandins | 70–85 | |
Cardiac valvular disease | Serotonin, 5-HIAA, neurokinin A, substance P | ~40–60 | |
Telangiectasias | Serotonin, bradykinin, prostaglandins | 25 | |
Bronchospasm | Serotonin, bradykinin | 15–19 | |
Pellagra (dermatitis, diarrhea, dementia) | Niacin deficiency due to excess tryptophan metabolism | 5–7 |
Not all patients with carcinoid tumors develop the carcinoid syndrome. Symptoms develop when the secretory products released from the tumors gain direct access to the systemic circulation, bypassing metabolism in the liver. The conditions in which such a bypass may develop include the presence of liver and lung metastases draining directly into the caval circulation, retroperitoneal disease with drainage into paravertebral veins, or primary sites of disease outside the gastrointestinal tract [37, 38]. In up to 90 % of patients, the development of the carcinoid syndrome is associated with metastatic tumors originating in the midgut [37]. In contrast, bronchial carcinoid tumors are associated with the carcinoid syndrome in approximately 10 % of cases, and nearly all hindgut tumors are hormonally silent. As many as 40 different substances have been identified in various carcinoid tumors (Table 3) [18]. Some of these tumor products are responsible for the carcinoid syndrome, but the relative contributions of each and specificity of any for particular components of the syndrome are yet unknown.
Table 3
Association of carcinoid syndrome with carcinoid tumor localization and secreted compounds
Site of tumor | Localization | Secreted substances | Carcinoid syndrome |
|---|---|---|---|
Foregut | Bronchus | 5-Hydroxytryptophan, histamine, peptide hormones, ACTH (bronchial, thymus) | Atypical, rarely Cushing’s syndrome |
Thymus | |||
Stomach | |||
Duodenum | |||
Pancreas | |||
Midgut | Jejunum | Serotonin, peptide hormones, prostaglandins | Classical |
Ileum | |||
Appendix | |||
Ascending colon | |||
Hindgut | Transverse colon | Variable peptide hormones | Rare |
Descending colon | |||
Sigmoid colon | |||
Rectum |
Skin Flushing
Most studies cite flushing in the skin as the most common and first discernible symptom of carcinoid syndrome that occurs in over 90 % of patients [5, 39, 40]. Four types of flushing patterns may occur including the diffuse erythematous, violaceous, prolonged, and bright red patchy type. These patterns can last from 2 to 10 min, affecting the face, neck, and upper chest, or up to 2–3 days, affecting the whole body with lacrimation, edema of the salivary glands, and hypotension [8, 10]. The diffuse erythematous flush is short-lived, lasts 2–10 min, affects the face, neck, and upper chest, and is usually associated with midgut carcinoids [8, 11]. The violaceous flush type is similar to the diffuse erythematous flush, except that attacks may be longer and patients may develop a permanent cyanotic flush with facial telangiectasias, watery eyes, and injected conjunctiva. This type of flushing is usually associated with foregut carcinoids. Prolonged flushes last up to 2–3 days, may involve the whole body, and may also be associated with profuse lacrimation, swelling of the salivary glands, hypotension, and facial edema. This type of flushing is a hallmark of bronchial carcinoids. The bright red, patchy flushing typically seen with gastric carcinoids is the result of increased histamine production. As a consequence of prolonged vasodilatation, some patients may develop venous telangiectasia characterized by purplish vascular lesions, similar to those seen in acne and rosacea. These lesions most often occur on the nose, upper lip, and malar areas may appear late in the course of the carcinoid syndrome.
Based on the fact that serotonin is the major recognized chemical secreted by the majority of carcinoid tumors, it is commonly, but incorrectly, thought that serotonin is the cause of the flushing. It has been shown that the magnitude of the facial flushing does not correlate with the levels of serotonin present [41]. In addition, it was found that the injection of serotonin does not cause flushing, and serotonin antagonists, which ameliorate the diarrhea, do not alleviate the flushing [5, 30, 41].
A correlation between tachykinins levels and flushing has been described [19, 21, 42, 43]; however, direct proof that tachykinins can cause flushing has not yet been provided [10]. It has been shown that intraluminal tachykinin concentrations are higher in patients with carcinoid syndrome than in healthy control subjects [44]. An association between flushing and secretion of kallikrein (the enzyme producing bradykinin, one of the most powerful vasodilators known) has been reported by some investigators [7, 45] but questioned by others [31, 41].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree