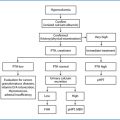
Fig. 13.1
Multiple cervical scars in a patient with persistent primary hyperparathyroidism MEN1-related, after three previous failed operations due to incorrect diagnosis and inadequate surgical approach
Moreover, both negative preoperative localization studies and misleading results of quick PTH assay contribute to an increased risk of P-HPT in the case of MGD.
A rarer but more deceptive cause of persistent disease is the synchronous double parathyroid adenoma that accounts for about 2–10% of cases with primary HPT [13]. Despite the use of accurate preoperative localization techniques and the availability of intraoperative adjuncts like quick PTH monitoring, double adenomas remain difficult to predict [17–18].
Finally, more rarely, negative explorations are due to supernumerary ectopic adenomas, which represent a real challenge also for skilled and experienced surgeons [19].
On the contrary, R-HPT represents a more complex and controversial problem since it usually arises after a successful primary operation in patients with MGD with regrowth of the remnant after subtotal parathyroidectomy or proliferation of unremoved supernumerary affected parathyroid glands in the case of total parathyroidectomy. Rarer causes include regrowth of autografted tissue in inherited syndromes.
In exceptional cases, R-HPT is due to metachronous double adenoma, local or distant recurrence of parathyroid carcinoma and a condition of parathyromatosis owing to local spread of parathyroid cells after capsule rupture during initial surgery [1–14].
In the case of P-pHPT and R-pHPT a careful analysis of the possible etiologies, based on a review of family history data, imaging performed before the first intervention and operative notes of primary surgery, is of utmost importance before stating the surgical indication and planning reoperation.
Furthermore, a careful preoperative evaluation, including laryngoscopic vocal cord evaluation and accurate preoperative localization imaging, should be routinely employed to assist the surgeon in minimizing the extent and morbidity of re-exploration.
Imaging studies play a critical role in reoperations. Since the need of an urgent exploration is a very rare event, a blind exploration should always be avoided. The aim of imaging is to obtain an adequate road map to guide the surgeon [20].
The description and the accuracy of the available imaging are discussed in detail in Chapter 9.
13.2 Indications
There is a general agreement that reoperation is indicated in the case of severe and ongoing symptoms or markedly elevated serum calcium levels. There are no data specifically addressing the efficacy of surgical versus conservative treatment for asymptomatic recurrent or persistent hyperparathyroidism disease. Therefore according to some authors [21], it is reasonable (grade C recommendation) to apply the same guidelines adopted for the management of asymptomatic primary hyperparathyroidism stated from the Third International Workshop held in 2009 [22]. At the same time, in a situation of asymptomatic persistent/recurrent HPT with mild hypercalcemia and negative localization studies, a “wait and watch” approach or medical treatment with bisphosphonates or cinacalcet may be preferred. In fact, sometimes, the higher risks related to the surgery should be considered worse than the effects of the disease. Finally, patients with profound comorbidity may not tolerate a surgical procedure, even if a recent article [23] showed that obesity and ASA 3 classification are independently associated with reoperation.
13.3 Surgical Technique
Cervical re-exploration is technically difficult due to the distorted neck anatomy from the fibrotic scar. Moreover, in the case of remedial surgery, causative hyperfunctioning parathyroid tissue can be located ectopically and thus can be more difficult to find. For all these reasons reoperative patients experience lower cure rates and an increased risk of injury to delicate cervical structures including recurrent laryngeal nerves and normal parathyroid tissue. In fact, permanent recurrent nerve palsy and permanent hypoparathyroidism rates have been reported up to 10 and 20%, respectively in these patients [24]. Moreover, in reoperative patients a significant increase in re-admission rate is demonstrated [23].
Consensus expert opinion states that the most important factor in minimizing morbidity and maximizing cure rates in HPT patients is surgeon experience [25, 26]. Although no data concerning the association between surgical case volumes and outcomes are available for remedial surgery, the reported findings in the case of primary surgery indicate that it should be recommended that these challenging cases are referred to experienced surgeons. It is critical that the surgeon has a clear knowledge of the neck anatomy and a deep understanding of embryology, developmental migration and both eutopic and ectopic locations of parathyroid glands [20].
In conclusion, a carefully planned operative procedure, eventually employing additional adjuncts, is of utmost importance for surgical success in reoperative settings [27].
13.4 Cervical Approach
Since hyperfunctioning parathyroid tissue is more frequently located in the neck, also in case of persistent/recurrent disease, often it could be removed via a cervical incision [28]. Two possible ways can be used for cervical exposure: a standard medial “front-door” approach and a posterolateral “back-door” access (Fig. 13.2). In the reoperated neck, the strap muscles become fused to the underlying thyroid gland and trachea. Therefore, by using a “front-door” approach the operator faces the same operative planes previously explored during the initial surgery, whereas by using the alternative approach he can avoid the scarred areas.
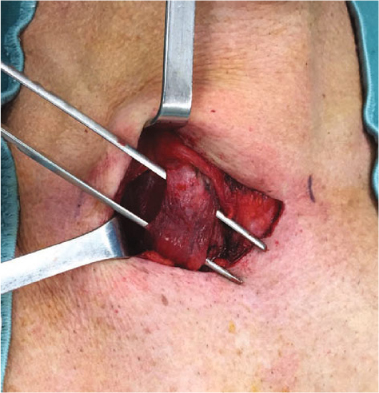
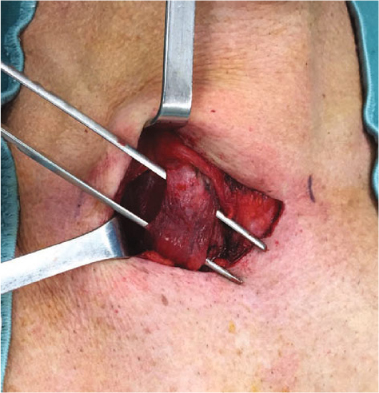
Fig 13.2
“Back-door” access in reoperative parathyroidectomy
The medial approach provides the most direct and easy access to any gland located close to the lower pole of the thyroid or in the thyrothymic ligament. Furthermore, this approach allows for bilateral neck exploration, when necessary. Nonetheless, the medial approach can be challenging because of the distortion of the operative field and the strong adhesions among the anatomic structures due to the fibrotic scar. On the contrary, the posterolateral approach, using the same previous skin incision but starting the subplatysmal dissection in the plane between the sternocleidomastoid and the strap muscles, permits avoidance of the scarred field and allows the recurrent laryngeal nerve and posteriorly located parathyroids (superior/paraesophageal glands) to be reached more directly [24, 28]. Obviously, the choice of the operative exposure is mainly dependent on the preoperative localization studies and the extension of primary surgery. An experienced surgeon could ultimately decide to use both the accesses when required.
Independent from the surgical access, the surgeon can decide to perform a targeted approach or a systematic bilateral neck exploration.
Focused parathyroidectomy. The focused approach, which has the main advantage of limiting the surgical exploration and reducing the risk of complications, should be proposed only if it is likely that a single well-localized hyperfunctioning tissue is present. This is the case with: a missed adenoma not found at primary operation; concomitant or metachronous double adenoma; regrowth of a parathyroid remnant after a subtotal parathyroidectomy; recurrence of supernumerary hyperplastic tissue after total parathyroidectomy; local recurrence of parathyroid carcinoma. Focused approaches should be avoided in the case of uncertain localization of the aberrant gland and the suspicion of MGD.
In the case of a focused approach, selected patients may be candidates for minimally invasive parathyroidectomy, under locoregional or general anesthesia, according to the patient’s characteristics and surgeon’s preference. Contraindications for a minimally invasive approach are in part correlated to the operator’s experience and familiarity with the technique. However, absolute contraindications remain the presence of voluminous parathyroid adenoma and suspicion of parathyroid carcinoma.
Among the minimally invasive approaches, for the widely diffuse, the open minimally invasive parathyroidectomy (OMIP, see Chapter 11) and the video-assisted parathyroidectomy (MIVAP, largely described in Chapter 12) should be mentioned.
Bilateral neck exploration. When multiglandular involvement is suspected, surgery should be aimed at resection of the remaining glands also considering the possibility of supernumerary and ectopic glands. The typical case is persistent hyperparathyroidism due to inadequate first intervention in the familiar forms where parathyroid hyperplasia is always present. In this case, a conventional Kocher cervicotomy and a systematic bilateral neck exploration should be considered the best approach. In the case of familiar forms, a concomitant cervical bilateral thymectomy should also be performed in order to reduce the risk of further recurrence. If the preservation of a viable parathyroid remnant is not certain, cryopreservation for possible future reimplantation or concomitant autograft to heterotopic site, such as in the forearm, should be considered. In fact, permanent hypoparathyroidism with severe postoperative hypocalcemia can represent a life-threatening complication in reoperative parathyroid surgery.
Despite the availability of performing preoperative imaging studies and the surgical skill, a subset of patients will require major efforts at the time of reexploration. In these cases, adjuvant techniques, including extensive bilateral cervical exploration, cervical thymectomy, retroesophageal and carotid sheath exploration, blind thyroid lobectomy on the side of the missing gland or at least selective internal jugular venous sampling for PTH, may be required.
In exceptional cases, despite a meticulous preoperative study and an extensive cervical dissection, hyperfunctioning parathyroid tissue may not be identified. When all but one parathyroid have been identified in eutopic position, the presence of ectopic parathyroid tissue on the ipsilateral side of the missed gland can support the strategy to stop its blood supply by ligating the artery. Selective parathyroid devascularization should be considered only when all the other maneuvers (also including resection of ipsilateral thyroid lobe) fail [20].
13.5 Extracervical Approach
Even if the vast majority of mediastinal parathyroid adenomas can be resected by a cervical approach that allows access to both anterior and posterior mediastinum, rarely a partial or complete median sternotomy is required [31]. Anterior low mediastinal glands may be approached by an anterior mediastinotomy. Video-assisted thoracoscopic surgery, particularly fit for lesions in the aorto-pulmonary window, might be preferred to classic thoracotomy because it is less invasive and more comfortable for the patient [20, 32, 33]. Endocrine surgeons should have the skill set required to explore the mediastinum and, sometimes, a multidisciplinary approach involving a thoracic surgeon might be necessary.
13.6 Operative Adjuncts
Radioguidance. Gamma probe detection of 99mTc-radiolabeled sestamibi (MIBI) can be used to guide cervical dissection in reoperative settings [34]. Nonetheless, this technique did not encounter a large consent because background signal from normal tissue and especially from the vessels may create interference [35]. Moreover, it adds little information to what is already offered by a well performed preoperative MIBI scan.
Rapid intraoperative PTH assay. The use of the rapid intraoperative PTH (ioPTH) assay is associated with a 94–96% cure rate in the remedial setting and it is routinely employed by most centers [36–38]. It allows the surgeon to confirm that the removed gland is the only source of abnormal PTH secretion and leads to terminate the operation stopping unnecessary and potentially harmful additional exploration. This may represent a real advantage in reoperative surgery where a more extensive exploration poses a higher risk of injuries. This intraoperative adjunct eliminates the need for an intraoperative frozen section, saving time and costs. In addition, in difficult explorations, it can guide the dissection, when an ipsilateral PTH gradient is present at the bilateral internal jugular vein sampling. However, several authors criticize the utility of PTH assay in patients with familiar forms, as well as in patients with other kind of MGD, especially during remedial exploration [15, 39, 40]. For these reasons we and other authors have suggested that delayed samples should be obtained at 20 minutes or later and stricter interpretative criteria to consider the patient cured [35, 41, 42].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree