© Springer-Verlag Italia 2016
Guido Gasparri, Nicola Palestini and Michele Camandona (eds.)Primary, Secondary and Tertiary HyperparathyroidismUpdates in Surgery10.1007/978-88-470-5758-6_88. Management of Primary Hyperparathyroidism
(1)
Department of Surgical Sciences, University of Turin, Turin, Italy
8.1 Medical vs. Surgical Treatment
The treatment of symptomatic primary hyperparathyroidism (pHPT) is surgical. Medical therapy has a role for the patient who does not want to, or cannot, be operated on: in these cases hypercalcemia is controlled with cinacalet and the bone mineral density (BMD) is improved with bisphosphonates.
In the asymptomatic forms the treatment is surgical when at least one of the criteria proposed by the 4th International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism is present [1]. In the cases in which there are no indications for surgery, the medical treatment must be personalized to the individual case working out when it is considered necessary to improve the BMD and to lower the level of calcium [2–4].
Further information about the medical therapy can be found in Chapter 5.
8.2 Alternative to Surgery
Do alternatives to surgery for the removal of parathyroid tissue exist? Only in selected cases — that is in recurrence of pHPT in patients with MEN1 — syndrome, can therapy with the administration of ethanol by percutaneous injection be proposed. A study by the Mayo Clinic reported 37 cases subjected to 123 sessions of administration of ethanol with satisfactory results in 73% of the cases and transitory complications in 5% [5]. This experience is limited to complex cases and therefore cannot be proposed as a standard alternative to surgery.
8.3 Indications for Parathyroidectomy in Primary Hyperparathyroidism
When observing the clinical manifestations, pHPT is typically classified as either symptomatic or asymptomatic. As you will see in our description with the perfecting of diagnostic methods and with the progress of pathophysiology studies on the activity of the parathyroid hormone, the dividing line between these two forms is becoming finer. Patients who have high levels of calcium and parathyroid hormone associated with hypercalciuria, and phosphorus at levels lower than normal, are considered symptomatic.
Precise clinical manifestations accompany the change in the results of the blood tests:
Renal symptoms: renal lithiasis, nephrocalcinosis with possible colic. Bone symptoms: bone fragility, fractures caused by minor traumas, due to a reduction of the bone density, especially in the cortical sites. Neurological symptoms: emotional instability, depression, difficulty in concentrating, asthenia and precocious fatigue. Gastrointestinal symptoms: gastric hyperacidity, abdominal pain. Cardiological symptoms: left ventricular hypertrophy, presence of calcification of the myocardium. Acute hypercalcemia.
All these symptoms, except those which are characteristic of a neuropsychiatric syndrome, tend to improve after parathyroidectomy (PTx) and, therefore, it is widely accepted that the treatment of symptomatic forms is surgical.
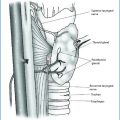
The preoperative localization of the pathological glands is important but must not be considered criteria for operability, in that, besides experience, the surgeon has at his disposition the intraoperative dosage of parathyroid hormone (PTH), which is fundamental in modulating the surgical exploration.
If the patient cannot undergo an operation due to serious comorbidities or because he chooses not to be operated, medical treatment is necessary, which must be based on the intake of cinacalet for the control of the calcemia, while the intake of bisphosphonates controls bone diseases.
The treatment of the asymptomatic forms is much more difficult, controversial and above all still in evolution. This issue is important because today almost 80% of the diagnoses of hyperparathyroidism are performed on patients without symptoms.
In reality, the definition “asymptomatic disease”, conceived to indicate the presence of hyperparathyroidism with more or less high levels of calcemia but without the clinical symptoms of symptomatic HPT, can be considered surpassed. This is so because hyperparathyroidism seems to be ever more responsible for the pathological situations, which in recent years have been studied in greater detail.
In 1990, the National Institutes of Health (NIH) organized a Consensus Development Conference, which recommended the following elements as parameters for the indication for surgery in the asymptomatic forms: calcemia greater than 12 mg/dL, episodes of hypercalcemia, reduced creatinine clearance, nephrolithiasis, high calciuria, osteoporosis, age <50 years old [6].
From 1990 up until today, there have been four workshops on the Management of Asymptomatic Primary Hyperparathyroidism, the last of which was in 2013 in Florence, Italy [2].
What has changed in recent years in respect to the indications of 1990? Besides the identification of new parameters, a better knowledge of the natural history of pHPT has been obtained. Even if there is evidence in favor of the stability of the disease with regards to the blood tests and BMD, the new data show that this stability does not last. The duration is 8 years for the blood values and 12 years for the BMD. After 15 years of observation, a third of the subjects followed presented the appearance of nephrolithiasis, high calcemia values and a worsening of the BMD. On the contrary, after a PTx intervention, the blood values improve in a short time and the bone density improves and in time stabilizes.
Therefore, the choice of surgery in asymptomatic forms must be proposed when it is sure that there is a period of time in which a careful follow-up can be carried out.
The guidelines certified at the 4th Workshop in 2013 tried to make it possible to highlight the symptomatic picture earlier while being aware of the difficulty in defining the asymptomatic one. The premise is that surgery remains the definitive therapy as long as it is carried out by expert surgeons who are dedicated to this pathology [7].
At the 2013 Workshop in Florence experts were set 25 questions compared to the 22 set in 2008 [8]. The first questions concerned the correctness of the diagnosis of pHPT: the PTH measurement using second- and third-generation kits and the level of 25-dihydroxyvitamin D, which must be within the normal range, are fundamental. The diagnosis of pHPT is also confirmed when the calcemia values are normal, both ionized and total, and there are no known causes responsible for the increase of values of PTH. The clinical course of these forms over time is unforeseeable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree