Fig. 2.1
Embryologic origin of the parathyroid glands, thyroid, and thymus (Source: Ferrari CC et al. Surgical strategy for primary hyperparathyreoidism with thyroid hemiagenesis. Langenbecks Arch Surg 2014;399:1077–1081. Springer)
The embryonic pharynx develops early from the rostral-most part of the foregut. At about three to four weeks of human development, the lateral walls of the pharynx show a non-uniform growth that gives genesis laterally to the pharyngeal apparatus [1, 2]. It consists of five pairs of pharyngeal (branchial) pouches and corresponding pharyngeal clefts, with pharyngeal arches between each pair [3]. This relatively simple metameric organization has a transient existence between the 4th and 6th weeks of embryonic life [1]. As development progresses, it becomes obscured by a complex rearrangement process.
The parathyroid glands develop from the embryonic endoderm of the pharyngeal region between the 5th and 12th week of gestation. Each pair of glands has a different origin. The inferior ones originate from the dorsal part of the third branchial pouch and, therefore, are designated as parathyroid III (P III). The thymus arises from the ventral portion of the same pouch; this common origin justifies labeling P III and thymus as parathymus. The superior parathyroid glands arise from the dorsal part of the fourth branchial pouch and are referred to as parathyroid IV (P IV). The fate of the ventral portion of this pouch is little understood in humans. Some authors believe that it gives rise to a small amount of thymic tissue (rudimentary thymus IV), which subsequently undergoes involution [1]. The fourth and possibly rudimentary fifth pharyngeal pouches also produce ultimobranchial bodies, which contribute to the formation of the lateral thyroid anlages and contain migrating neural cleft cells that will become the parafollicular (C) cells of the thyroid [1].
The earliest appearance of a parathyroid anlage occurs at the 5th week of gestation, in embryos from 4 to 8 mm in length [4–6]. When the embryo is about 9 mm in length (6th week of gestation), the tissue destined to become the parathyroid can be recognized as a thickening of the third branchial pouch, and a solid budlike nodule in the fourth [5, 6]. At this stage, the branchial pouches are still joined to the pharynx by pharyngobranchial ducts. Subsequently the ducts narrow and finally divide, leaving a pair of lobulated bodies at each side of the midline. One pair represents the thymus and the P III (third branchial complex), and the other the lateral thyroid and the P IV (fourth branchial complex) [6].
At the 13 to 14 mm stage, the thymus undergoes a phase of rapid ventral growth, and the third branchial complex migrates in a medial and caudal direction through the entire length of the embryonic neck [4, 5, 7]. At the beginning the thymus and the P III primordia are intimately joined, then the P III remains as a budlike projection from its upper end. Finally, it takes a spherical shape, intimately attached to the cephalic pole of the thymus cord [5]. After completing the descent through the neck, the P III increases in size and separates from the thymus, remaining at the level of the lower thyroid pole or within the thyrothymic ligament, a vestigial structure indicative of their former connections [7].
During this time, the P IV rudiment remains attached to the ultimobranchial body and follows its medial migration toward the lateral lobe of the median thyroid anlage [5–7]. The two elements of the fourth branchial complex are initially connected by an interlobular stalk, which is interrupted when the lateral and median thyroid become incorporated [5, 6].
The separation of the parathyroids from the other elements of the third and fourth branchial complexes is usually accomplished when the embryo is approximately 20 mm in length [5,6].
2.2 Anatomy
2.2.1 Number
Typically, superior and inferior paired glands develop to a total of four. Nevertheless, supernumerary parathyroid glands represent a relatively frequent finding, and the presence of less than four glands has also been reported.
Autopsy studies report supernumerary parathyroid glands in 2.5–20% of cases [8–12]. However, it seems probable that the frequency is higher, as small parathyroid rudiments may be difficult to discover. In a series of surgical patients operated on for renal hyperparathyroidism, a condition where even microscopic parathyroid rests of embryological origin undergo hyperplasia, supernumerary glands and/or microscopic deposits of parathyroid tissue were found in 30-37% of cases, most frequently within the thymus [13, 14].
In the classic autopsy study of Åkerström et al. [10] supernumerary parathyroid glands were found in 12.7% of cases. The majority of these glands were either rudimentary or divided, small (weight <5 mg), and in close proximity of a normal gland. Proper supernumerary glands (weight >5 mg) occurred in 5% of subjects; in two thirds of the cases they were found below the thyroid, in the thymus or in relation to the thyrothymic ligament. Most of the individuals had just one supernumerary gland, but in a single subject up to 11 glands were counted.
Large studies from postmortem dissections report the finding of three parathyroid glands in 2-3.6% of cases [10, 12]. Obviously, the exact number of individuals with less than four parathyroids may be impossible to determine, because a missing gland could represent a failure of identification rather than an absent gland.
2.2.2 Gross Appearance
The parathyroid glands may vary in size, shape and color, but retain a gross appearance that allows them to be identified and differentiated from other structures.
The average dimensions are about 5–7 × 3–4 × 1–2 mm [8, 11, 12]; the mean weight of a single gland is 35 to 40 mg [8, 11, 12], but it may range from 10 to 70 mg [6]. The total weight of adult parathyroids usually ranges from 120 to 160 mg [4].
According to Åkerström et al. [10] in 83% of cases the parathyroid glands are oval, bean-shaped or spherical. Sometimes they are elongated (11%), and more rarely they appear bilobated (5%) or flattened to form a thin multilobated structure (1%). Other variations such as teardrop, pancake, rod-like, sausage, and leaf-shaped parathyroid glands have been described [8].
The color varies with age. In the newborn, the parathyroids are gray and semitransparent. In children, they are light pink. In the adult, their color varies from a light yellow-brown to a darker red-brown, depending on the adipocytes content and vascularization [6, 7].
Whatever their size, shape, or color, the parathyroid glands always share some distinctive characteristics. They have a soft elastic consistency and retain their original shape during dissection. If flattened by the development of a thyroid nodule, they can become rounded again when detached from its surface. They are encapsulated and have sharp outlines and a smooth, glistening surface. Parathyroids have a particular affinity for fat and are often found completely or partially embedded in a fatty globule; characteristically, they can be easily separated from the adjacent fatty structures. Fat is softer, paler, and straw-colored, with no definite shape. Thyroid tissue is firmer, less homogeneous, and a darker wine-red in color with bluish-gray tints. Lymph nodes are firmer, more rounded, less homogeneous, and their color is white or dirty gray. Thymic tissue is paler, grayish-yellow or grayish-pink, and granular [7].
2.2.3 Normal Location
2.2.3.1 Superior Parathyroid Glands
As already mentioned, the superior parathyroid glands originate from the fourth pharyngeal pouch. As they lose their attachment with the pharyngeal wall, they migrate along with the ultimobranchial body toward the posterior surface of the lateral lobes of the median thyroid anlage. The short migration distance accounts for a relatively constant location behind the upper half of the thyroid lobe (Fig. 2.2).
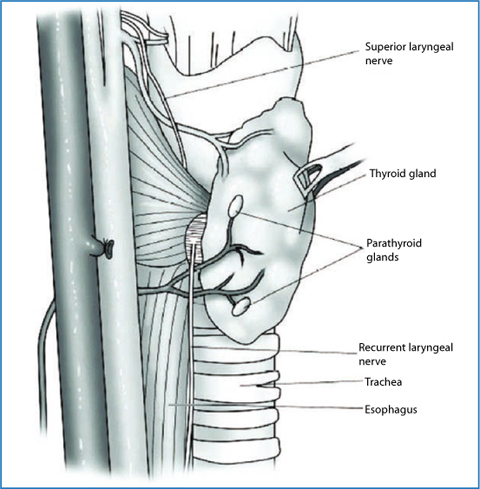
Fig. 2.2
Normal anatomy of the parathyroid glands (Source: Phitayakorn R, McHenry CR. Parathyroidectomy: Overview of the anatomic basis and surgical strategies for parathyroid operations. Clin Rev Bone Miner Metab 2007;5:89-102. Springer)
In a study of 645 parathyroid glands from 160 postmortem subjects, Wang [8] found that the most common site of the P IV was the cricothyroid junction posterior to the thyroid lobe, where he identified 77% of the glands. Here the glands were intimately associated and occasionally hidden by the recurrent laryngeal nerve and the adjacent vascular branches. Most were suspended by a small pedicle and enveloped by a pad of fatty tissue. Another 22% of the glands were tucked behind the upper pole of the thyroid lobe, where they invariably laid beneath the thyroid-investing fascial sheath.
In an autopsy study of 503 cases, Åkerström et al. [10] found that 80% of the P IV were located on the posterior aspect of the thyroid gland, within a circumscribed area 2 cm in diameter centered about 1 cm above the crossing point of the recurrent laryngeal nerve and the inferior thyroid artery. Another 12% of the glands were identified in a more cranial location, behind the upper pole of the thyroid lobe, and 4% resulted in a lower position, behind the middle third of the lobe, sometimes obscured by the inferior thyroid artery, the recurrent laryngeal nerve, of the posterior protrusion of the thyroid named tubercle of Zuckerkandl.
2.2.3.2 Inferior Parathyroid Glands
The inferior parathyroid glands arise from the third pharyngeal pouch and have a common origin and migration with the thymus. Starting at the region of the pharyngeal wall, they migrate inferior and medially in the neck, and normally separate from the thymus before it enters the anterior mediastinum. This accounts for the fact that the inferior parathyroid glands are more widely distributed. They are usually found around or just below the lower pole of the thyroid lobe, in a plane ventral to that of the superior parathyroids, and anterior to the recurrent laryngeal nerves (Fig. 2.2).
In the study of Wang [8], 81% of the P III were distributed in the area between the lower poles of the thyroid gland and the thymus. In 42% of the cases, the P III was found in the anterior or posterolateral surface of the lower thyroid pole. In 39% of the cases, the P III were located below the thyroid in the lower neck, within the thyrothymic ligament, or in the upper pole of the thymus itself.
The results of Åkerström et al. [10] are quite similar. More than half of the P III (61%) were located around the lower thyroid pole. Another common location (26%) was in the area inferior to the thyroid, in intimate association with the thyrothymic ligament, or within the cervical part of the thymus.
Due to the embryologic descent of the P III crossing that of the P I V, an inferior parathyroid gland can rarely be found at the same level as the superior one, above or below the crossing of the inferior thyroid artery and recurrent laryngeal nerve. In this instance, it may not be possible to differentiate the superior and inferior glands [10, 15]. Occasionally the two glands are so close to each other that they appear to be fused; this rare finding is known as kissing pairs [6]. A kissing-paired parathyroid can be differentiated from a bilobular gland by the presence of a cleavage plane between the glands.
2.2.3.3 Symmetry of Locations
In the majority of cases, parathyroid glands are located in a symmetrical position in the neck. Åkerström et al. [10] found symmetrical positions of the superior and the inferior glands in 80% and 70% of the cases, respectively. In 60% of the subjects they observed a relative symmetry for all four glands.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree