Subclinical Thyrotoxicosis
Douglas S. Ross
The introduction of serum thyrotropin (TSH) measurements into clinical practice during the early 1970s provided the necessary tool for defining subclinical hypothyroidism, although it took several years for our present understanding and an accepted definition of this entity to evolve (see Chapter 47). Similarly, the introduction in the 1980s of sensitive immunometric TSH assays allowed detection of subnormal serum TSH values in patients with no symptoms or signs of thyrotoxicosis. Subclinical thyrotoxicosis is defined biochemically as a low serum TSH concentration and normal serum free thyroxine (T4) and triiodothyronine (T3) concentrations. While patients may have symptoms, the symptoms of thyroid dysfunction are so nonspecific that they do not reliably predict the presence or degree of thyroid dysfunction. Patients with low serum TSH concentrations who have high serum free thyroid hormone concentrations are defined as having overt thyrotoxicosis. Before the introduction of sensitive assays for serum TSH, subclinical thyrotoxicosis could be demonstrated by the finding of blunted responses of serum TSH after administration of thyrotropin-releasing hormone (TRH). Now, however, TRH testing is not necessary because serum TSH responses to TRH are usually proportional to basal serum TSH concentrations. The studies reviewed in this chapter document the clinical and biologic importance of subclinical thyrotoxicosis. The management guidelines of the American Thyroid Association and the American Association of Clinical Endocrinologists recommend treating subclinical hyperthyroidism in high-risk individuals when the TSH is persistently lower than 0.1 mU/L (1).
Table 33.1 Common Causes of Subclinical Thyrotoxicosis | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Etiology
The major causes of subclinical thyrotoxicosis are similar to those of overt thyrotoxicosis (Table 33.1). Conceptually, there are two groups of patients: Those who have subclinical thyrotoxicosis caused by exogenous thyroid hormone therapy and those in whom it is caused by slight endogenous overproduction of T4 and/or T3.
Exogenous Subclinical Thyrotoxicosis
On the basis of a 3.7% prevalence of hypothyroidism in the United States (NHANES 1999–2002) (2), as many as 10 million people in the United States, and perhaps as many as 200 million people worldwide, are taking thyroid hormone and are therefore at risk for subclinical thyrotoxicosis because of either overzealous replacement therapy or intentional suppressive therapy. When sensitive methods for measuring serum TSH first became available, an estimated 40% to 50% of patients
taking T4 replacement therapy had subnormal serum TSH concentrations (3), but the proportion has diminished as a result of the use of these assays to monitor therapy and recognition of the potential dangers of over-replacement. Nonetheless, in a 2010 population-based study, 19.8% of patients taking thyroid hormone replacement had a TSH less than 0.4 mU/L (4). The prevalence of low serum TSH was even higher (41%) in individuals over age 65 years (5). Patients with thyroid cancer, thyroid nodules, or multinodular or diffuse goiter who are treated with T4 to suppress serum TSH levels to below normal have subclinical (if not overt) thyrotoxicosis. Therapy with thyroid hormone to suppress serum TSH should be considered only when the benefits exceed the potential risks of subclinical thyrotoxicosis.
taking T4 replacement therapy had subnormal serum TSH concentrations (3), but the proportion has diminished as a result of the use of these assays to monitor therapy and recognition of the potential dangers of over-replacement. Nonetheless, in a 2010 population-based study, 19.8% of patients taking thyroid hormone replacement had a TSH less than 0.4 mU/L (4). The prevalence of low serum TSH was even higher (41%) in individuals over age 65 years (5). Patients with thyroid cancer, thyroid nodules, or multinodular or diffuse goiter who are treated with T4 to suppress serum TSH levels to below normal have subclinical (if not overt) thyrotoxicosis. Therapy with thyroid hormone to suppress serum TSH should be considered only when the benefits exceed the potential risks of subclinical thyrotoxicosis.
Endogenous Subclinical Thyrotoxicosis
The common causes of endogenous subclinical thyrotoxicosis include multinodular goiter with autonomy, autonomously functioning thyroid adenomas, Graves’ disease, and painless (lymphocytic) or subacute (granulomatous) thyroiditis (6).
In a study of patients over age 55 years, hyperthyroidism from autonomy in a nodular goiter was subclinical in 57% of patients, while hyperthyroidism due to Graves’ disease was subclinical in only 6% of patients (7). The prevalence of autonomously functioning adenomas and nodular goiter varies considerably from one region of the world to another. This variation is the result of differences in dietary iodine intake and perhaps also genetic differences. For example, in a US study, the ratio of patients with thyrotoxicosis caused by an autonomously functioning adenoma to those with thyrotoxicosis caused by Graves’ disease was 1:50 (8), whereas in Switzerland it was 1:2 (9). Thus in a European study, 22% of patients with nodular goiter had subclinical thyrotoxicosis, and 28% had autonomous areas on thyroid radionuclide imaging (10). Subclinical thyrotoxicosis also occurs in patients with mild Graves’ disease (11), or Graves’ eye disease (12), and can persist following treatment. In one study, about 20% of patients had a chronically suppressed serum TSH after a course of antithyroid drugs or surgery, and were more likely to relapse than a comparable group with normal serum TSH levels (13).
The thyrotropic activity of high serum chorionic gonadotropin concentrations during early pregnancy may cause a transient increase in serum free T4 and T3 concentrations, usually within the normal range, and low serum TSH concentrations in approximately 10% of pregnant women (14). This transient subclinical hyperthyroidism may be considered normal physiology; it is not associated with adverse pregnancy outcomes (15).
Evaluation
The evaluation of patients with subclinical thyrotoxicosis is similar to that of overt thyrotoxicosis (see Chapter 31), except, as noted above, autonomy in a nodular goiter is more common than Graves’ disease when hyperthyroidism is minimal (7). Free T3 should be measured if a reliable assay is available, since 3 of 148 patients (2%) with apparent subclinical thyrotoxicosis had free T3 toxicosis (16). Many defer definitive evaluation unless treatment is being considered. The management guidelines of the American Thyroid Association and the American Association of Clinical Endocrinologists recommend a radioactive iodine uptake, and scan when nodularity is present, to assess the etiology of thyrotoxicosis (1). One or more focal areas of increased uptake indicate an autonomous nodule or autonomy within an adenomatous goiter; diffuse uptake suggests Graves’ disease; and in the absence of an iodine load, nearly absent uptake suggests painless thyroiditis, subacute thyroiditis, factitious ingestion of thyroid hormone, or struma ovarii. Alternatively, Graves’ disease may be diagnosed by measuring TSH receptor antibodies.
Differential Diagnosis
There are other causes of low serum TSH concentrations, but many of the patients have abnormal serum T4 and T3 concentrations (Table 33.1). Patients with pituitary or hypothalamic disease who have hypothyroidism may have low serum TSH concentrations, and the concentrations are often low in patients with severe nonthyroidal illness, especially those receiving glucocorticoid or dopamine therapy (17). Following treatment and during resolution of overt thyrotoxicosis, low serum TSH concentrations may be associated with low or normal serum T4 and T3 concentrations due to delayed recovery of the pituitary–thyroid axis (18). Finally, epidemiologic data show that the distribution of serum TSH levels is shifted to the left in black persons in comparison to Caucasians (19) and in smokers (20). It is therefore possible that a mildly subnormal serum TSH could be normal for certain black individuals and cigarette smokers, and there is a risk of potential misdiagnosis of mild subclinical hyperthyroidism in these persons.
Epidemiology and Natural History
In the United States, among 13,344 people with no known thyroid disease in the National Health and Nutrition Examination Survey (NHANES III), 0.7% had subclinical thyrotoxicosis (19). In a Swedish community-based study of 2,000 people attending a medical clinic, 3.3% had low serum TSH concentrations without overt thyrotoxicosis (21); only 9% of the subjects with subclinical thyrotoxicosis had thyroid abnormalities (e.g., multinodular goiter, thyroiditis), and 40% had a normal serum TSH concentration on recall a few weeks later. In a US study of 968 subjects over 55 years of age, 0.7% had endogenous subclinical thyrotoxicosis (22). In another US study, 46 of 2,411 subjects (1.9%) over 60 years of age had subclinical thyrotoxicosis, with serum TSH values less than 0.1 mU/L (23); during a 4-year follow-up period, only two developed overt thyrotoxicosis, and serum TSH concentrations became normal in most of the remainder. In a similar study from England, 6.3% of women and 5.5% of men had low serum TSH concentrations (<0.5 mU/L); a year later, the serum TSH values were normal in 60% of these subjects, and only one (1.5%) had overt thyrotoxicosis (24). In Sweden, 1.8% of 886 subjects 85 years of age or older had subclinical thyrotoxicosis (25). And in the United States the prevalence of subclinical thyrotoxicosis in the Cardiovascular Health Study among those aged 65 years or more was 1.5% (26). Thus, the prevalence of subclinical thyrotoxicosis in the community has varied from 0.7% to 6.0%,
depending on the criteria used, the location, and the age of the population, being higher in older subjects. More than half of these subjects, especially those with slightly low serum TSH values, had normal values when retested during follow-up, and few developed thyrotoxicosis.
depending on the criteria used, the location, and the age of the population, being higher in older subjects. More than half of these subjects, especially those with slightly low serum TSH values, had normal values when retested during follow-up, and few developed thyrotoxicosis.
In an analysis of a primary care database that included over 442,000 patients without known thyroid disease, 52% of patients with TSH less than 0.35 mU/L had a normal value on follow-up testing in the absence of treatment (27). Accordingly, all patients suspected of having subclinical thyrotoxicosis should have repeat testing (e.g., after at least a 1-month interval) before being evaluated for underlying thyroid disease or considered for treatment.
In a 5-year follow-up study of 96 patients from New Zealand with subclinical thyrotoxicosis (TSH <0.25 mU/L), the progression to overt thyrotoxicosis occurred in 8% at 1 year, increasing to 26% at 5 years. At 5 years, overt hyperthyroidism occurred in 9%, 21%, and 61% of patients whose subclinical hyperthyroidism was due to Graves’ disease, nodular goiter, and autonomous nodules, respectively (28). In contrast, in a 2-year follow-up study from Brazil 20% (6 of 30) of patients with nodular disease and 40% (15 of 30) of patients with Graves’ disease progressed from subclinical (TSH <0.1 mU/L) to overt hyperthyroidism (29). However, among those with only minimal subclinical thyrotoxicosis (TSH 0.1 to 0.4 mU/L) with a mean follow-up of 41 months, only 3 of 102 women aged 60 years or more progressed to overt thyrotoxicosis (30).
Clinical and Biologic Importance
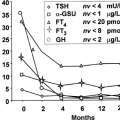
Although suppression of TSH secretion defines subclinical thyrotoxicosis, the increases in serum free thyroid hormone concentrations that cause the suppression have effects on other tissues that are similar to, but less marked, than those of overt thyrotoxicosis. Both the pituitary and the systemic effects of the increases are considered here.
Physiology of Suppression of TSH Secretion
The negative feedback relationship between serum TSH and free T4 (and T3) concentrations is log-linear. Therefore, very small increases in endogenous thyroid hormone production, or only slightly excessive doses of the exogenous thyroid hormone, decrease serum TSH concentrations to below the normal range (31) (see Regulation of Thyrotropin Secretion, Chapter 10D). Groups of patients with low serum TSH concentrations who receive slightly excessive doses of T4 have serum T4 and T3 concentrations greater than the mean values for normal subjects but within the respective normal ranges. Presently, most clinicians accept serum TSH measurements as the most sensitive indicator of thyroid hormone status (in the absence of pituitary or hypothalamic disease). Several findings, however, raise the question of whether this is always the case. In laboratory animals, intrapituitary deiodination of T4 to T3, a reaction that is catalyzed primarily by type 2 T4–5′-deiodinase (see Chapter 7), contributes more of the T3 bound to the T3 nuclear receptors, and serum T3 contributes less, compared with most other organs (32). Hence, the extent of T3-induced inhibition, or lack thereof, on TSH secretion, may vary somewhat independently of the serum T3 concentration. Polymorphisms in the type 2 T4–5′-deiodinase with reduced activity have been described (33). In addition, the concentrations of the different isoforms of the T3 nuclear receptor are different in the pituitary and peripheral organs (see Chapter 8), and these concentrations are altered discordantly in states of thyroid hormone excess or deficiency (34). Some euthyroid elderly patients with low serum T4 and normal serum TSH concentrations appear to have a decreased set point for T4– and T3-mediated feedback inhibition of TSH secretion (35). Thus, it is possible that serum TSH levels do not always accurately reflect thyroid function in peripheral tissues.
Bone and Mineral Metabolism
Thyroid hormone has a direct resorptive effect on bone, and overt thyrotoxicosis is associated with increased bone resorption and, to a lesser extent, increased bone formation and an increase in fracture rate (36). While some data suggest that TSH has a direct role inhibiting both osteoclasts and osteoblasts (37), other studies suggest that bone loss in thyrotoxicosis is primarily mediated by thyroid hormone interaction with its alpha receptor (38). Cortical bone is affected more than trabecular bone. Patients with a history of thyrotoxicosis have a 1.5-fold increased risk of osteoporosis (39) and a 1.8-fold increased risk of hip fracture (40). Even in patients with normal thyroid function, lower bone density (41,42) and vertebral fracture (43) correlate with TSH values in the lower portion of the normal range.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree