SPECIFIC CAUSES OF HYPOCALCEMIA
HYPOPARATHYROIDISM
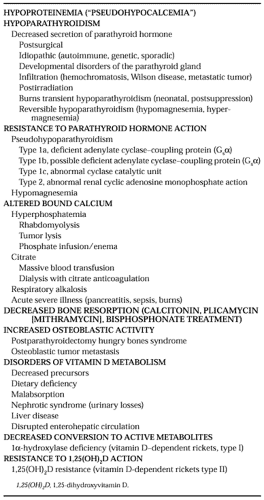
A biochemical state of functional hypoparathyroidism occurs either because of failure of secretion of PTH or, less commonly, failure of PTH action at its target tissues. The clinical forms and characteristics of hypoparathyroidism are described below and in Table 60-2.
SURGICAL HYPOPARATHYROIDISM
Hypoparathyroidism occurs most commonly as a result of parathyroid or thyroid surgery or after radical surgery for laryngeal or esophageal carcinoma. The resulting hypoparathyroidism can be transient or permanent and sometimes may not develop for many years. In some patients, a chronic state of “decreased parathyroid reserve” may exist18 in which hypocalcemia becomes apparent only when mineral homeostasis is stressed further by other factors such as pregnancy, lactation, or illness.
Transient Hypocalcemia after Parathyroid Surgery.
Hypocalcemia frequently occurs after removal of a hyperfunctioning parathyroid adenoma because of deficient secretion of PTH by the remaining previously suppressed parathyroid tissue. Hypoparathyroidism is usually transient, because the normal parathyroid glands recover function quickly (generally within 1
week), even after long-term suppression. Transient postoperative hypocalcemia may be exaggerated or prolonged in those patients who have significant preexisting hyperparathyroid bone disease. In these patients the surgically induced reduction of previously elevated plasma PTH results in an increased movement of plasma calcium (and phosphorus) into remineralizing “hungry bones.”19 Treatment with calcium and a short-acting vitamin D metabolite may be required until the bones heal.
week), even after long-term suppression. Transient postoperative hypocalcemia may be exaggerated or prolonged in those patients who have significant preexisting hyperparathyroid bone disease. In these patients the surgically induced reduction of previously elevated plasma PTH results in an increased movement of plasma calcium (and phosphorus) into remineralizing “hungry bones.”19 Treatment with calcium and a short-acting vitamin D metabolite may be required until the bones heal.
Permanent Hypoparathyroidism after Parathyroid Surgery.
Permanent hypoparathyroidism after an initial neck exploration for primary hyperparathyroidism is rare and develops in ˜1% of patients. The incidence is greatly increased with repeated neck surgery for recurrent or persistent hyperparathyroidism, after subtotal parathyroidectomy for parathyroid hyperplasia, or when surgery is performed by an inexperienced surgeon.
Hypocalcemia after Thyroid Surgery.
After thyroid surgery, the incidence of permanent hypoparathyroidism varies widely, depending on the underlying thyroid lesion and the extent of the procedure, as well as on the experience of the surgeon. Hypoparathyroidism may result from direct injury, inadvertent removal, or devascularization of the parathyroid glands. Permanent hypoparathyroidism is distinctly unusual after a hemithyroidectomy and should be relatively uncommon even after total thyroidectomy.20,21 However, up to 33% of patients who undergo a total thyroidectomy for cancer may develop transient postoperative parathyroid insufficiency.22
Transient hypocalcemia occurs in approximately one-third of patients who undergo a subtotal thyroidectomy for thyrotoxicosis. The fall in plasma calcium level generally occurs within 24 to 48 hours after surgery and can be sufficient to produce symptoms of tetany. The mechanism of this hypocalcemia is not well understood. Frequently, hyperthyroidism is associated with increased bone turnover and resorption, elevated plasma ionized calcium levels, and suppressed parathyroid function. Although the proposal has been made that hypocalcemia occurs as calcium moves into remineralizing hungry bones after reduction of thyroid hormone levels,23 the early development of hypocalcemia appears to be inconsistent with this abnormality. Some patients may have unappreciated damage to the parathyroid glands18; whether thyroidectomy causes hypocalcemia by producing hypercalcitonemia is disputed.24,25 Clearly, whatever the initiating cause, the secretory response of the suppressed parathyroid glands is inadequate to maintain a normal plasma calcium.24,25
IDIOPATHIC HYPOPARATHYROIDISM
The term idiopathic hypoparathyroidism describes a heterogeneous group of rare disorders that share in common the deficient secretion of PTH. Although most cases are sporadic, the familial occurrence of idiopathic hypoparathyroidism has been reported. Within these families hypoparathyroidism may occur as part of a complex autoimmune disorder (see Chap. 197) associated with multiple endocrine deficiencies (i.e., type 1 polyglandular syndrome)26 or in association with diverse developmental abnormalities (e.g., nephropathy, lymphedema, nerve deafness, or tetralogy of Fallot).27,28,29,30,31,32,33,34,35,36,37,38,39,40,41 and 42 The pleiotropic nature of many of these various syndromes suggests that the genetic basis of PTH deficiency is not related to a specific defect intrinsic to the parathyroid gland.
Type 1 Polyglandular Syndrome.
Type 1 polyglandular syndrome may be sporadic or familial with an autosomal recessive inheritance pattern. The classic triad of this syndrome is hypoparathyroidism, adrenal insufficiency, and mucocutaneous candidiasis (HAM). The recognition that affected patients may have additional components has led to the suggestion that a more inclusive term be used to describe the syndrome: autoimmune polyendocrinopathy–candidiasis–ectodermal dystrophy (APECED).43 The syndrome is first recognized in early childhood, although a few individuals have developed the condition after the first decade of life. The clinical onset of the three principal components of the syndrome typically follows a predictable pattern, in which mucocutaneous candidiasis first appears at a mean age of 5 years, followed by hypoparathyroidism at a mean age of 9 years and adrenal insufficiency at a mean age of 14 years.43 Patients may not manifest all three elements of the triad. Alopecia, keratoconjunctivitis, malabsorption and steatorrhea, gonadal failure, pernicious anemia, chronic active hepatitis, thyroid disease, and insulin-requiring diabetes mellitus occur in some patients.26 Antibodies directed against the parathyroid, thyroid, and adrenal glands are demonstrable in many patients,44 and a T-cell abnormality has been described.45,46 The presence of antibodies may not correlate well with the clinical findings. In those cases that have been examined pathologically, complete parathyroid atrophy or destruction has been demonstrated. In some patients, treatment of hypoparathyroidism has been complicated by apparent vitamin D “resistance,” possibly related to coexistent hepatic disease or steatorrhea, or both. Mutations in the gene AIRE (autoimmune regulator gene) have been identified in patients with APECED. AIRE, located on chromosome 21 (21q22.3), encodes a nuclear protein containing zinc-finger motifs; this suggests that it may play a role as a transcriptional regulator.47,48 AIRE is expressed in tissues important in the development and regulation of the immune system (e.g., the thymus and lymph nodes). Although many different mutations have been reported throughout the world,48a the majority of patients harbor either the R257X mutation or a 13-base-pair deletion in exon 8, each resulting in a truncated AIRE protein.49,50 The function of the AIRE protein remains unknown. The hypothesis has been made that the AIRE protein may regulate the immune response via B- and T-cell stimuli.47 Functional analysis of the AIRE protein and further molecular analysis of the AIRE gene will elucidate the molecular pathogenesis of APECED.
Isolated Hypoparathyroidism.
Isolated idiopathic hypoparathyroidism, in which PTH deficiency is unassociated with other endocrine disorders or developmental defects, is usually sporadic, but it may occur on a familial basis. Most commonly, the onset of isolated hypoparathyroidism is between the ages of 2 and 10 years, although it may first be recognized in adult life, and the onset may be at any age up to the eighth decade. Females are affected twice as often as males.
A high incidence of parathyroid antibodies is seen in patients with isolated idiopathic hypoparathyroidism, and some cases may be examples of incomplete expression of the type 1 polyglandular syndrome (APECED, see earlier). Some patients may possess antibodies that inhibit the secretion of PTH,51 rather than cause parathyroid gland destruction.52 In other cases that have been examined pathologically, fatty replacement53 or atrophy with fatty infiltration and fibrosis54 has been described.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree