Small Cell Carcinoma
Mary Beth Beasley
Small cell lung carcinoma (SCLC) comprises approximately 20% of all lung carcinomas, classically presenting as a hilar mass with extensive adenopathy, although approximately 20% of SCLC are peripherally located.1-3 The incidence of SCLC appears to have decreased slightly in the past decade.3 SCLC frequently presents at an advanced stage and has a poor prognosis with a 5-year survival rate of 10% and a 10-year survival rate of <5%.1,2,4 Less than 10% of patients with SCLC have stage 1 disease.3 SCLC is seen almost exclusively in cigarette smokers and is more common in males. Depending on the location, size, and extent of spread, symptoms may include cough, dyspnea, hemoptysis, weight loss, or other constitutional symptoms. Superior vena cava syndrome is a presenting finding in 10% of patients. Associated paraneoplastic syndromes such as syndrome of inappropriate antidiuretic hormone, Cushing syndrome, autoimmune neuropathies, and encephalomyelitis, among others, maybe encountered.4,5 SCLC has typically been regarded as distinct from other lung carcinomas due to its responsiveness to chemotherapy; however, some studies have shown that surgery is of potential benefit in low-stage disease.6,7,8,9 SCLC has been historically divided into limited (confined to the thorax) and extensive stage disease; however, in the 7th edition of the AJCC staging guidelines it is recommended that SCLC be staged using the same criteria as non-small cell lung carcinoma (NSCLC).10,11
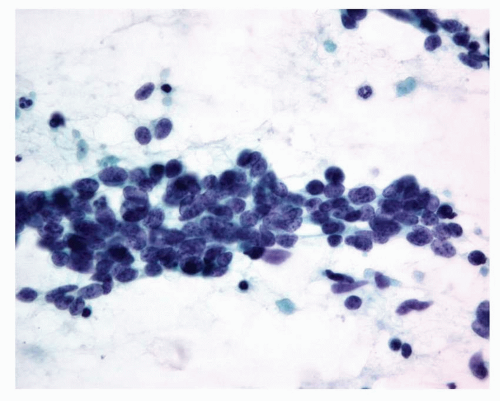
SMALL CELL CARCINOMA, CYTOLOGY
Cytologically, SCLCs exhibit cells that are approximately three to four times the size of a resting lymphocyte, generally arranged singly and in small clusters. Tumor cells show a finely granular (“salt and pepper”) chromatin pattern, with scant cytoplasm. Small nucleoli maybe present occasionally, but do not predominate. Typically, there are frequent mitotic figures and nuclear molding is common. Necrotic cells or necrotic debris maybe found in the background (Figs. 9-1 and 9-2).
SMALL CELL CARCINOMA, GROSS FEATURES
SCLCs are typically centrally located tumors, often not involving the bronchus but frequently involving hilar lymph nodes. The surface is typically off-white to tan-gray, and frequently areas of tumor necrosis or hemorrhage are present (Fig. 9-3).
SMALL CELL CARCINOMA, HISTOLOGY
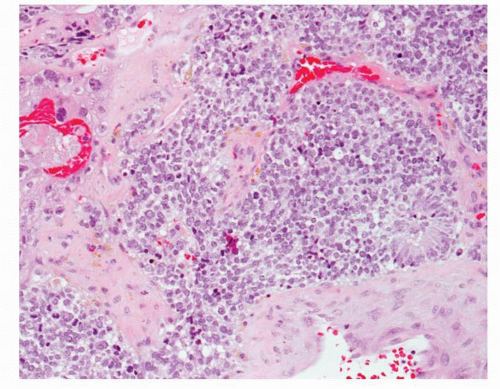
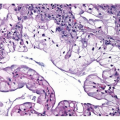
The World Health Organization (WHO) classification of lung tumors defines SCLC as a tumor with >10 mitoses per10 high-power fields (HPF) and small cell cytologic features.2 Histologically, SCLC is characterized by oval to spindle shaped cells approximately three to four times the size of a resting lymphocyte, as noted above. The cells have very high nuclear/cytoplasmic ratios and scant, almost indiscernible cytoplasm. Nuclear molding may be observed, and cytoplasmic borders are usually indistinct. Nuclear chromatin is finely granular and nucleoli are typically absent
or inconspicuous (Fig. 9-4). While the mitotic rate is by definition >10 per 10 HPF, the mitotic rate is generally in excess of 50 to 60 per 10 HPF, with a median of 80 mitotic figures per 10 HPF.2,12 Necrosis, both infarct like and single cell, is usually present (Fig. 9-5). Encrustation of blood vessels with basophilic material, the so-called Azzopardi phenomenon, may also be encountered. SCLC may occur in combination with large cell neuroendocrine carcinoma (LCNEC) or with other NSCLCs such as adenocarcinoma or squamous cell carcinoma (Figs. 9-6 and 9-7).2,13 Such tumors are termed “combined SCLC” in the WHO classification, and the histology of the additional component should be specified. Pure SCLC may exhibit a range of cell sizes and it is recommended that any second component comprise at least 10% of the tumor before assigning the designation of combined SCLC.2
or inconspicuous (Fig. 9-4). While the mitotic rate is by definition >10 per 10 HPF, the mitotic rate is generally in excess of 50 to 60 per 10 HPF, with a median of 80 mitotic figures per 10 HPF.2,12 Necrosis, both infarct like and single cell, is usually present (Fig. 9-5). Encrustation of blood vessels with basophilic material, the so-called Azzopardi phenomenon, may also be encountered. SCLC may occur in combination with large cell neuroendocrine carcinoma (LCNEC) or with other NSCLCs such as adenocarcinoma or squamous cell carcinoma (Figs. 9-6 and 9-7).2,13 Such tumors are termed “combined SCLC” in the WHO classification, and the histology of the additional component should be specified. Pure SCLC may exhibit a range of cell sizes and it is recommended that any second component comprise at least 10% of the tumor before assigning the designation of combined SCLC.2
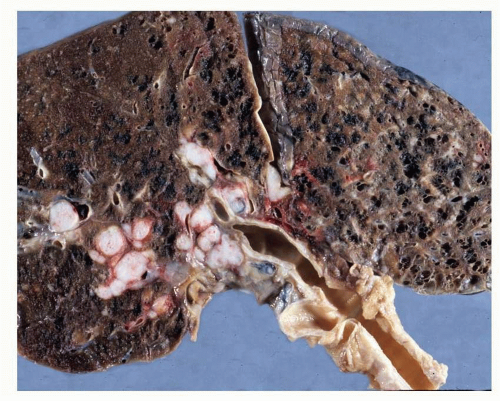 FIGURE 9-3 Gross image of lung with SCLC, showing off-white central tumor nodules that abut but do not involve the bronchi, and associated more peripheral intrapulmonary metastatic tumor nodules. |
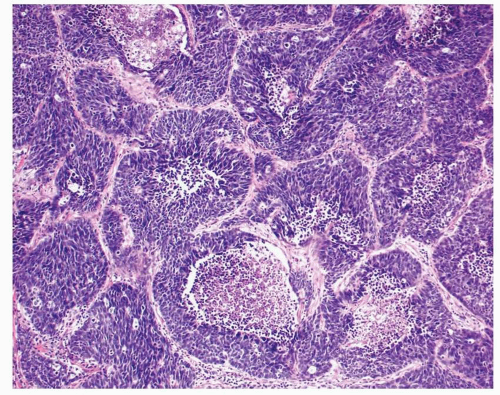
On small transbronchial biopsies (TBBX), SCLC may exhibit significant crush artifact. Such cases should be interpreted with caution as other tumors such as lymphoma, squamous cell carcinoma, and carcinoid tumors may also show considerable crush artifact (Figs. 9-8 and 9-9). In needle core biopsies and larger or resected specimens, the cells of SCLC may appear larger in comparison to their appearance on a TBBX and have slightly more discernable cytoplasm; however, in comparison to lymphocytes the cells remain proportionally small and nuclear cytoplasmic ratios
remain very high. Additionally, a more obvious neuroendocrine growth pattern with organoid morphology and rosette formation may be seen in larger specimens (Fig. 9-10).13
remain very high. Additionally, a more obvious neuroendocrine growth pattern with organoid morphology and rosette formation may be seen in larger specimens (Fig. 9-10).13
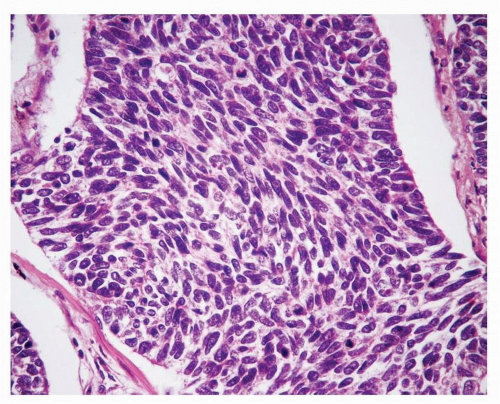 FIGURE 9-4 SCLC is comprised of oval to spindle cells with granular nuclear chromatin, absent or inconspicuous nucleoli, and scant cytoplasm. |
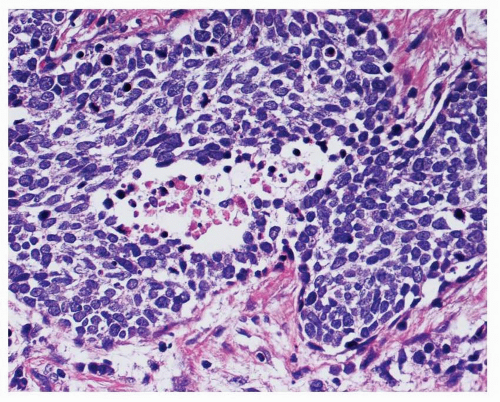 FIGURE 9-5 SCLC is characterized by a very high mitotic rate and areas of necrosis are frequently present. |
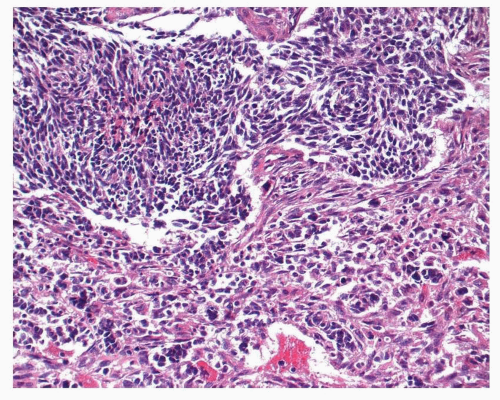 FIGURE 9-6 Combined SCLC. In this unusual case, SCLC (top) is combined with a pleomorphic/spindle cell carcinoma (bottom). |
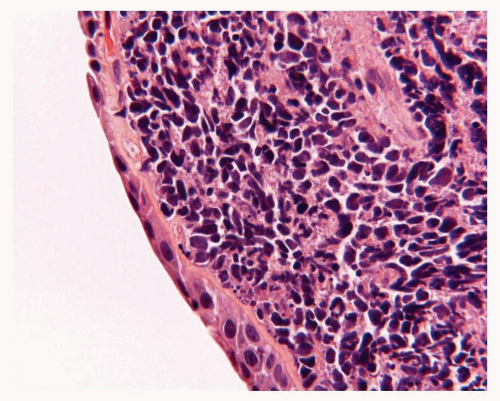 FIGURE 9-8 High-power image of SCLC showing typical crush artifact. Crush artifact is frequently seem in biopsies of SCLC but should be interpreted with caution. |
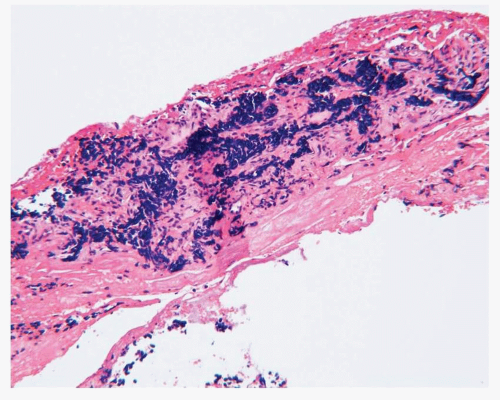 FIGURE 9-9 High-power image of a typical carcinoid tumor with extensive crush artifact mimicking SCLC. The case was initially misdiagnosed as SCLC. |
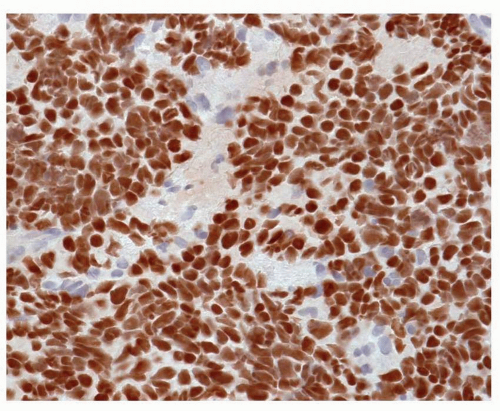
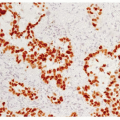
SMALL CELL CARCINOMA, IMMUNOHISTOCHEMISTRY
SCLC is positive for cytokeratins such as AE1/AE3 or CAM 5.2 and characteristically exhibits a “dotlike” pattern (Fig. 9-11). Cytokeratin 7 is frequently negative, but may be positive in a significant minority of cases, whereas cytokeratin 20 is consistently negative.14 Other cytokeratins such as CK 34βE12 and CK5/6 are also typically negative.15 Neuroendocrine markers such as chromogranin, synaptophysin, and CD56 (NCAM) are positive in the majority of cases; however, it should be noted that individual markers may be negative in up to 30% of cases and multiple markers may be negative in 10% to 15% of cases (Fig. 9-12).13,16 As such, negative neuroendocrine markers do not necessarily militate against a diagnosis of SCLC in the presence of otherwise appropriate morphologic features. Thyroid transcription factor-1 (TTF-1) is also positive in the majority of SCLC but, unlike TTF-1 expression in adenocarcinoma, TTF-1 expression in SCLC does not definitively support a pulmonary origin and maybe found in SCLC arising in other locations (Fig. 9-13).17,18 and 19 Napsin A has thus far been negative in SCLC but needs to be evaluated in a larger number of cases at this time.20
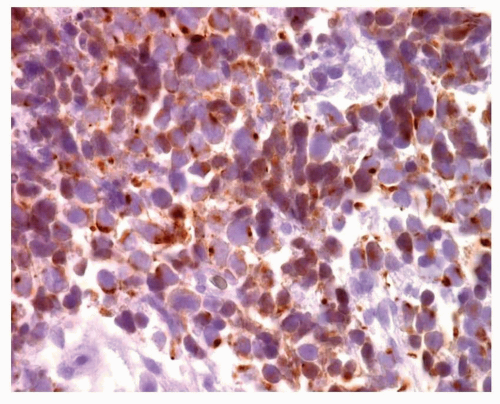 FIGURE 9-11 High-power image of SCLC with AE1/AE3 immunostain showing punctuate or “dot-like” cytoplasmic positivity. |
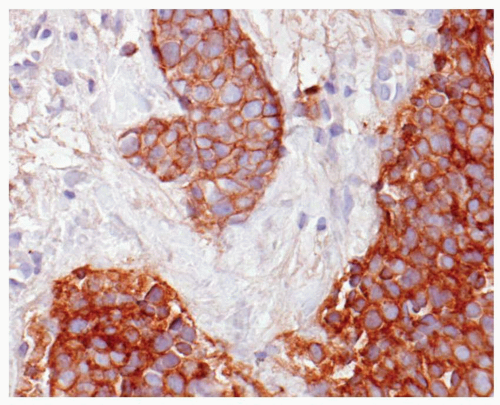 FIGURE 9-12 High-power image of SCLC stained with one of the neuroendocrine markers, CD56 (NCAM), showing strong cytoplasmic immunopositivity. |
SCLC is also typically positive for bcl-2 and c-kit.21 More recently, PAX-5, a marker typically seen in some lymphomas, has been reported to be positive in the majority of high-grade neuroendocrine carcinomas and negative in carcinoids.22 Estrogen receptor and progesterone receptor expression has also been reported in SCLC.23 Molecular studies have shown that SCLC, in contrast to typical (TC) and atypical carcinoid tumors (AC), typically exhibits a very high frequency of p53 mutations and Rb inactivation. Rb inactivation demonstrates an inverse correlation with p 16 and cyclin D1.24,25,26 and 27 SCLC also typically has a high frequency of deletions on chromosomes 3p and 17p and has an inverted bcl-2/Bax ratio.24,25 and 26 SCLC also has a high level of telomerase activity28 Loss of heterozygosity for 3p, 5q21, and 9p has also been found.25,26 Mutations of the MEN1 gene, as seen in TC and AC, are not seen in SCLC.29 SCLC has not been shown to harbor EGFR mutations.30
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree