SEX CORD STROMAL TUMORS
Tumors given this designation are thought to be derived from the specialized ovarian stroma. They are the most common type of hormonally active neoplasm. The components include granulosa, theca, Sertoli, Leydig, and gonadal stromal cells.13,14 (See also ref.14a.)
GRANULOSA TUMORS
The granulosa tumor is the most common malignant functioning tumor of the ovary. When functional, granulosa tumors almost always are estrinizing, although rare tumors are virilizing. These tumors occur in all age groups but are most frequent in women between 30 and 50 years of age. Approximately 5% of granulosa tumors occur in young girls. The symptoms differ with the age of the patient. Most young girls present with isosexual precocious pseudopuberty, whereas women in their reproductive years usually experience disturbances of the menstrual cycle that range from amenorrhea to menometrorrhagia. Occasionally, breast enlargement occurs. Postmenopausal women typically present with vaginal bleeding secondary to endometrial hyperplasia. The frequency of endometrial hyperplasia and carcinoma ranges from 10% to 20%, depending on the criteria used for the diagnosis of these lesions. Androgenic granulosa cell tumors are associated with recent onset of hirsutism.
Granulosa tumors are bilateral in 5% of patients and range in size from microscopic to >30 cm in diameter (median, 9 cm). Small neoplasms are solid, encapsulated by a thin fibrous layer, and located in the ovarian cortex, whereas larger tumors may replace the ovary and become focally cystic. Virilizing tumors tend to be thin-walled, cystic tumors. Blood is often present within the cysts and explains the presentation of hemoperitoneum secondary to rupture that occurs in 10% of cases.
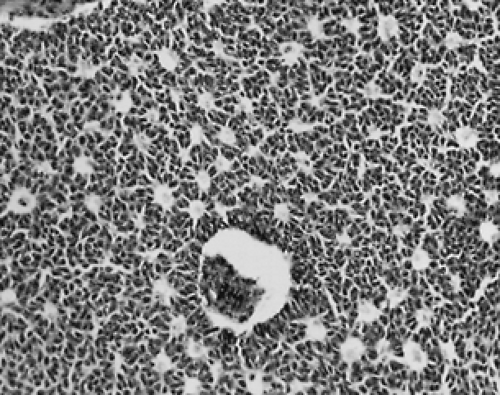
Granulosa tumors display many histologic patterns, including microfollicular (the most characteristic, showing many Call-Exner bodies; Fig. 102-3), macrofollicular, trabecular, insular, solid or diffuse, and juvenile. The pathologist must be aware of these patterns so that poorly differentiated carcinomas are not misdiagnosed as diffuse granulosa tumors. This relatively common error accounts for many of the examples of poor-prognosis granulosa tumors reported in the literature. Alpha-inhibin is expressed in granulosa cell tumors and other sex cord stromal tumors, but not in most carcinomas.15 Immunohistochemical staining for this peptide may aid in the differential diagnosis. The histologic appearance of granulosa cell tumors does not correlate with the prognosis in most studies. The neoplastic cells resemble normal granulosa cells, being small, round to ovoid, and uniform. The nuclei have a characteristic longitudinal groove (a “coffee bean” appearance), and the cytoplasm is pale with poorly defined borders. Occasional cells are luteinized. Reactive thecal cells occur in ˜25% of granulosa tumors. Anti-mullerian hormont (AMH) is a useful serum marker for these tumors.15a
The juvenile granulosa tumor, which accounts for 85% of granulosa cell tumors occurring before puberty, has distinctive features: the cells are larger, more pleomorphic, and often luteinized. Nuclear grooves are rare, and mitoses may be numerous.16 Despite these ominous-appearing features, the prognosis is excellent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree