Introduction
Thyroid hormone excess, also known as thyrotoxicosis, encompasses a wide range of signs and symptoms. Thyrotoxicosis and hyperthyroidism may have semantic distinctions but are often used interchangeably. Patients with clinical manifestations of severe thyrotoxicosis need urgent evaluation and may require hospitalization and emergency intervention. Therefore it is important to be able to recognize the presence of thyrotoxicosis, know the causative factors, evaluate its severity, and, when necessary, know the critical aspects of management for patients with life-threatening disease.
Thyroid storm is a clinical syndrome of decompensated thyrotoxicosis in which the compensatory physiologic mechanisms have been overwhelmed. It is considered an endocrine emergency due to its high morbidity and mortality, and prior to the availability of advanced intensive care and multimodality therapeutic interventions, this condition was uniformly fatal. Outcomes remain very poor for patients not quickly identified and treated. Historically, cases of thyroid storm were associated with surgical interventions, but the majority of recognized cases are now medical, related to underlying infections, cardiovascular events, or other conditions. Not all patients will have a previous diagnosis of hyperthyroidism, and thyroid storm may occur in many circumstances with myriad precipitants. Despite its rarity, thyroid storm has been estimated to represent 1%–16% of hospital admissions for thyrotoxicosis, with estimates varying across studies depending upon methodology. , Providers should be vigilant in identifying patients who may have thyroid storm and initiating appropriate care.
This chapter provides a summary of the evaluation and management of patients with severe thyrotoxicosis and thyroid storm, with emphasis on the latter given the importance of recognizing and treating this condition.
Pathophysiology of Thyrotoxicosis and Thyroid Storm
Thyroid hormone exerts effects throughout the body. During thyrotoxicosis, the influences of excess thyroid hormone, particularly upon energy expenditure and the cardiovascular system, result in altered metabolism and hemodynamics for which the body may compensate but lacks the reserve capacity to adapt to additional stresses.
Excess thyroid hormone, predominantly through the nuclear actions of triiodothyronine (T3) on gene transcription and posttranslational modification, causes increased cardiac contractility and cardiac output (CO). Upregulated cardiac genes include myosin heavy chain, voltage-gated potassium channels, and sarcoplasmic reticulum calcium ATPase. T3 also directly induces vascular smooth muscle relaxation and vasodilation that is further augmented by the need to remove excess heat generated by upregulation of uncoupling protein-3, Na + /K + ATPase, and increased energy expenditure. Vasodilation in thyrotoxicosis causes relative underperfusion of renal and splanchnic circulation, resulting in increased activation of the renin-angiotensin-aldosterone system (RAAS) and subsequent increased blood volume and cardiac preload. This new compensated steady state puts a chronic workload on the cardiovascular system. Due to these changes, patients with thyrotoxicosis will typically demonstrate increased resting heart rate (HR) and respiratory rate. In compensated thyrotoxicosis, the skin is often warm and sweating may be present to dissipate heat, but fever is absent. Cardiovascular findings include reduced systemic vascular resistance (SVR), increased CO and ejection fraction, and increased pulmonary artery pressure. Systolic blood pressure is increased whereas diastolic and mean arterial pressure are reduced, leading to a widened pulse pressure. Thyrotoxic patients experience exercise intolerance due to the inability to further augment HR, CO, or SVR, as would occur in the euthyroid state. Additionally, weakness results from T3-mediated protein catabolism and skeletal muscle loss, including the diaphragm.
What differentiates thyroid storm from thyrotoxicosis is hemodynamic decompensation. Although an exact pathophysiology is unknown, the close association with precipitating physiologic stresses provides some clues. Events such as infection, acute coronary syndromes (ACS), hypovolemia, or trauma upset the tenuous hemodynamic balance created by the aforementioned physiologic changes, and there is an inability by the body to augment cardiovascular function further. Loss of effective circulation results in heat retention and organ hypoperfusion leading to the classic findings of hyperthermia and altered mental status. ,
Evaluation of Patients for Thyrotoxicosis
SIGNS AND SYMPTOMS OF THYROID STORM
The acute evaluation of a patient with thyrotoxicosis should proceed similarly to other patients, with emergent evaluation of cardiopulmonary, hemodynamic, and neurologic status. The initial secondary survey should seek to identify not only the presence of thyrotoxicosis but its most severe manifestations. These would include hyperthermia, altered mentation (e.g., confusion, lethargy, seizures, coma), tachyarrhythmia, or congestive heart failure (CHF; e.g., elevated jugular venous pressure, lower extremity swelling, pulmonary edema, congestive hepatopathy), and the presence of jaundice. Other manifestations may be evident but do not necessarily indicate thyroid storm.
The presentation of thyrotoxicosis may include classic symptoms or be atypical in nature. The influence of excess thyroid hormone on the body leads to a number of predictable symptoms. Heat intolerance, tachycardia and/or palpitations, fine bilateral tremor, weight loss, muscle weakness or fatigue, and dyspnea on exertion or shortness of breath are all symptoms of moderate to severe thyrotoxicosis regardless of the etiology. On physical examination, patients without thyroid storm are usually afebrile but their skin is warm to the touch from cutaneous vasodilation. The resting heart rate may be modestly elevated (80–100 beats per minute [bpm]) or tachycardic (>100 bpm). More significant cardiac effects include supraventricular tachyarrhythmias (SVT), particularly atrial fibrillation (AF) with rapid ventricular rate, or manifestations of heart failure. Not all patients with signs of heart failure will have reduced systolic function, but cardiomyopathy with markedly reduced ejection fraction can occur in a small percentage. In patients with preexisting arrhythmias or heart failure, these may be nonspecific findings or may demonstrate an acute worsening. In one retrospective cohort analysis, patients with a history of coronary artery disease, AF, peripheral vascular disease, renal failure, pulmonary circulation disorders, or valvular disease were more likely to have cardiogenic shock with thyroid storm. Additionally, 45% of patients with thyroid storm complicated by cardiogenic shock had a preexisting diagnosis of CHF.
Less commonly, these overt symptoms of thyrotoxicosis are absent. Symptoms may be limited, particularly in older individuals. Termed apathetic hyperthyroidism , in these individuals symptoms might only include weight loss, failure to thrive, fatigue, or lethargy. In patients already taking medications blocking the β-adrenergic system, classic symptoms of palpitations, tremor, or agitation may also be blunted. Rare manifestations of thyrotoxicosis include paroxysmal periodic paralysis, related to changes in potassium channel function, affecting the lower before the upper extremities, proximal more than distal muscle groups, and usually sparing the diaphragm.
CAUSES OF THYROTOXICOSIS AND THYROID STORM
Historical information, or specific signs or symptoms, may suggest an underlying cause of thyrotoxicosis. Common and significant etiologies are shown in Table 1.1 . A diffusely enlarged nontender thyroid gland suggests Graves’ disease, and the presence of a thyroid bruit is pathognomonic. Similarly, the presence of proptosis or other aspects of ophthalmopathy (periorbital edema, chemosis, optic nerve compression) are seen only in Graves’ disease. Exquisite thyroid tenderness and recent onset of symptoms suggest subacute thyroiditis; recent pregnancy may indicate postpartum thyroiditis; and the presence of a large nodule may represent an autonomously functioning nodule. Iatrogenic causes of thyroiditis include iodine exposure (including iodinated contrast agents), amiodarone-induced thyrotoxicosis (AIT), lithium, tyrosine kinase inhibitors, and immune therapy agents such as programmed death receptor (PD)-1 and cytotoxic T-lymphocyte–associated protein (CTLA)-4 inhibitors. The absence of thyroid pathology in the appropriate clinical setting may suggest accidental or surreptitious patient use of thyroid hormone, often exogenous T3 if symptoms are severe. Lastly, patients presenting with thyroid storm may not have a prior known diagnosis of thyroid disease (up to 30% of patients in one series ), and therefore clinician suspicion for underlying hyperthyroidism as a cause of clinical manifestations is paramount.
| Increased Thyroid Hormone Production | |
|---|---|
| Diagnosis | Mechanism |
| Graves’ disease | Stimulatory TSH receptor antibody |
| Inappropriate TSH secretion | TSH-secreting pituitary adenoma or pituitary resistance to thyroid hormone |
| Solitary or multiple thyroid nodule(s) | Autonomous thyroid hormone production by one or more adenoma(s) |
| Trophoblastic tumor or choriocarcinoma | HCG stimulation of the TSH receptor |
| Hyperemesis gravidarum | |
| Familial gestational hyperthyroidism | Mutant TSH receptor with increased sensitivity to HCG |
| Stuma ovarii | Ovarian teratoma with functional thyroid tissue a |
| Increased Thyroid Hormone Without Increased Production | |
| Diagnosis | Mechanism |
| Subacute thyroiditis (de Quervains’, granulomatous) | Release of preformed stored hormone |
| Postpartum and sporadic silent thyroiditis | |
| Medication induced thyroiditis (e.g., amiodarone, immune checkpoint inhibitor, tyrosine kinase inhibitor) | |
| Acute (infectious) thyroiditis | |
| Surgical manipulation | |
| Thyroid hormone ingestion | Excess exogenous thyroid hormone administration (particularly T3 containing) |
a Increased hormone not by the thyroid itself but by extra-thyroidal tissue. HCG, Human chorionic gonadotropin; T3, triiodothyronine; TSH, thyroid stimulating hormone.
The most common events precipitating thyroid storm are infections, ACS, venous thromboembolism or pulmonary embolism, trauma, surgery, childbirth, diabetic ketoacidosis (DKA), or discontinuation of medical treatment of Graves’ disease, with many other potential causes possible. , , , Unusual causes of thyroid storm reported in the literature include strangulation, stew containing marine neurotoxin, and thyroid impaction by a fishing trident. In short, any stressful event or concurrent medical condition may be a destabilizing force to push a patient with thyrotoxicosis into thyroid storm.
LABORATORY FINDINGS
If thyrotoxicosis in the hospital is suspected clinically, serum thyrotropin (thyroid stimulating hormone; TSH) is the most important test to establish this diagnosis definitively. In patients without a previous diagnosis of thyroid disease, obtaining a free thyroxine (T4) is also a practical and helpful test to demonstrate the presence and degree of thyroid hormone excess. However, the degree of thyroid hormone excess is not helpful in determining which patients simply have severe thyrotoxicosis and which have thyroid storm. , ,
When thyroid storm is suspected, other biochemical testing will help to determine the existence of organ system failure and/or presence of other acute conditions. Although laboratory information can be helpful in the evaluation of these patients, there is no test that confirms or excludes the diagnosis of thyroid storm. , Many laboratory abnormalities, including mild hyperglycemia, hypercalcemia, normocytic anemia, and elevation in alkaline phosphatase, are commonly seen in thyrotoxicosis. Because serum creatinine levels are lowered in the thyrotoxic state, providers should recognize that acute kidney injury may be underestimated. Despite frequently exhibiting mildly increased international normalized ratio (INR), studies have indicated relative hypercoagulability and increased risk of thrombosis in thyrotoxic patients. Elevated transaminase levels may be present in thyroid storm complicated by hepatic dysfunction, and elevated bilirubin is a particularly important finding, as it has been correlated with adverse outcomes in thyroid storm. ,
It is critical to identify concurrent illnesses that may be precipitants of thyroid storm. In addition to a thorough physical examination, sources of infection may be identified through urinalysis, blood cultures, chest and abdominal imaging, or lumbar puncture as clinically indicated. Evaluations should include looking for potential ACS, hyperglycemia and ketosis consistent with DKA, and drug use (especially cocaine and methamphetamines).
DIAGNOSIS OF THYROID STORM
Thyroid storm is a clinical diagnosis. Hospitalized patients with suspected or confirmed thyrotoxicosis should be evaluated for the severity of disease to identify those with clinical decompensation who would be defined as having thyroid storm. Coming to absolute agreement on the diagnosis of thyroid storm is less important than identifying the subset of thyrotoxic patients with the features of thyroid storm, because these patients are at the highest risk of morbidity or mortality and should receive emergent and directed therapy.
Traditionally, thyroid storm has been recognized as a clinical syndrome involving thyrotoxicosis, hyperthermia, alerted mentation, and a precipitating event. , , These findings, along with clinical evidence of congestive heart failure, identify patients at greatest risk for adverse hospital-based outcomes and mortality. Biochemical confirmation of thyrotoxicosis is not necessary to diagnose thyroid storm and treatment of suspected thyroid storm should not be delayed awaiting test results. However, in unclear cases, TSH concentration should be suppressed, confirming the presence of clinically significant thyroid hormone excess. TSH levels will most often be at the lower limit of detectability (e.g., 0.01 mIU/L) or undetectable. Mildly reduced TSH concentrations (0.1–0.5 mIU/L) frequently seen in patients with nonthyroidal illness, or the “euthyroid-sick syndrome,” are less suggestive of thyroid storm. The absolute level of thyroid hormone elevation is not predictive of the presence or absence of thyroid storm.
Any elevated temperature should be considered consistent with thyroid storm, but fevers will frequently be pronounced (>102°F). Additional clinical manifestations of thyrotoxicosis will frequently be present, but are less specific and often present in patients with severe thyrotoxicosis without thyroid storm. Because of the subjectivity of these assessments, the variability of patient presentations, and significant overlap between these features and other acute medical conditions in hospitalized patients, , , more objective diagnostic criteria have been published.
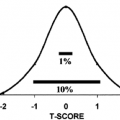
The Burch-Wartofsky Score (BWS) ( Table 1.2 ) assigns points for dysfunction of the thermoregulatory, central nervous, gastrointestinal-hepatic, and cardiovascular systems, with increasing points given for greater severity of dysfunction. A score of greater than 45 is considered highly suspicious, and very sensitive, for thyroid storm, but this cut-off is not specific, indicating thyroid storm in patients for whom this label is likely not appropriate. Furthermore, a patient with a score below 45 may still clinically be considered to have thyroid storm for which treatment should be given. Although potentially useful in quantifying disease severity, the numerical score should not supplant physician judgment. Other reported diagnostic criteria have not been clinically validated. Regardless of the precise criteria used, once a diagnosis of thyroid storm is confirmed or highly suspected, treatment should be initiated without delay.
| Parameter | Score | Parameter | Score |
|---|---|---|---|
| Thermoregulatory | Cardiovascular | ||
|
| ||
| 99.0–99.9 | 5 | 100–109 | 5 |
| 100.0–100.9 | 10 | 110–119 | 10 |
| 101.0–101.9 | 15 | 120–129 | 15 |
| 102.0–102.9 | 20 | 130–139 | 20 |
| 103.0–103.9 | 25 | >=140 | 25 |
| >=104.0 | 30 |
| |
| Absent | 0 | ||
| Central Nervous System | Present | 10 | |
| Absent | 0 |
| |
| Mild (agitation) | 10 | Absent | 0 |
| Moderate (delirium, psychosis, extreme lethargy) | 20 | Mild (pedal edema) | 5 |
| Severe (seizure, coma) | 30 | Moderate (bibasilar rales) | 10 |
| Severe (Pulmonary edema) | 15 | ||
| Precipitant History | |||
| Negative | 0 | Gastrointestinal–Hepatic | |
| Positive | 10 | Absent | 0 |
| Moderate (diarrhea, abdominal pain, nausea/vomiting) | 10 | ||
| Severe (jaundice) | 20 | ||
| Total Score | Diagnosis of Thyroid Storm | ||
| >45 | Likely | ||
| 25–45 | Impending | ||
| <25 | Unlikely | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree