Chapter Outline
Plain Language Summary 265
General Introduction and Structure of the Chapter 266
Genetic Predisposition to Breast Cancer 266
Characteristics of BRCA- Associated Breast Cancers Related to Screening 267
Screening Women With Known or Suspected Gene Mutation 267
Effectiveness of Screening Women With a Known or Suspected Gene Mutation 268
Increased Sensitivity of Screening MRI as an Adjunct to Mammography 269
The Role of Other Screening Modalities 276
Potential Mortality Benefits of Screening With MRI 277
Potential Harms of Screening With MRI and Mammography 281
Cost-Effectiveness of Screening Strategies Including MRI as an Adjunct to Mammography 287
Conclusion 293
References
Plain Language Summary
Women with certain genetic mutations (eg, BRCA1 and BRCA2 ) or with familial risk (without a known gene mutation but with a strong family history of breast or ovarian cancer) are at an elevated risk of developing breast cancer; from 57% to 65% in women with a BRCA1 mutation and from 45% to 49% in women with a BRCA2 mutation. The risk of developing breast cancer for women with familial risk depends on number, closeness and age of relatives with breast and ovarian cancer and is between the population risk (11%) and of women with known gene mutations. In some countries, these women at elevated (high) breast cancer risk are offered screening with annual magnetic resonance imaging (MRI) and mammography starting at age 30 or earlier, with the goal of detecting breast cancers at an early stage. This chapter reviews evidence on the benefits and the harms of breast cancer screening strategies in these women. Large-scale studies in women with a BRCA gene mutation have been conducted, whereas evidence for women at familial risk is limited. Recent evidence supports screening women at high risk with both MRI and mammography annually because this strategy detects most (84–94%) breast cancers and a large proportion are detected at an early stage. However, this strategy results in more false-positive results (ie, additional imaging and biopsies in women without cancer) compared to screening with a single modality, and some breast cancers are still missed by screening. Further, young women at elevated risk who undergo mammography before age 30 may be at an increased risk of radiation-induced breast cancer. In addition, using MRI is more expensive than mammography, and is more invasive as it requires intravenous contrast. The evidence on whether screening with both MRI and mammography saves lives is based on few, limited studies. Simulation models suggest that yearly screening with both MRI and mammography from age 30 is the most cost-effective strategy for women at elevated risk.
General Introduction and Structure of the Chapter
As women with known or suspected gene mutations have an increased lifetime breast cancer risk with an earlier age of onset, there has been much attention focused on effective breast screening of this high-risk population. In this chapter, the evidence regarding breast cancer screening in these women is reviewed. Evidence is based on studies considering different aspects of breast cancer screening including screening accuracy, mortality reduction, potential harms, and cost-effectiveness.
Genetic Predisposition to Breast Cancer
In the past two decades several major genes have been identified that are associated with an increased lifetime risk of breast cancer, such as BRCA1 , BRCA2 , TP53, CDH1 , STK11 , and PTEN . The two most common high-risk cancer-predisposing genes are BRCA1 and BRCA2 , and their association with breast cancer as well as ovarian cancer has been extensively studied. Other genes, such as TP53, STK11 , and PTEN , are rarer and associated with broader tumor syndromes. Guidelines on breast cancer prevention and management in BRCA families are based on very large series; however, large studies are not possible for the rarer tumor syndromes. Genes like PALB2, NF1, MEN1, RECQL , and CHEK2 mutations, especially the CHEK2*1100delC mutation, are known to be associated with a moderately increased risk of breast cancer and breast cancer recurrence; in general breast cancer risk management in these carriers has not been studied as extensively as in BRCA carriers. The largest group however, are the women with an increased risk due to a substantial family history, but without any detectable genetic mutation. In this section we will examine the breast cancer risk related to women with BRCA1/2 gene mutations and to women with a substantial family history of breast cancer without a proven gene mutation.
BRCA1 and BRCA2 gene mutations and their penetrance
The BRCA1 and BRCA2 gene mutations are related to the Hereditary Breast Ovarian Cancer Syndrome. The BRCA genes are tumor suppressor genes and belong to a family of genes involved in DNA repair or for eliminating DNA that cannot be repaired. Pathogenic mutations in either of these genes impair this process. The wild-type allele BRCA gene mutations are dominantly inherited which means any child of a BRCA mutation carrier has a 50% chance of carrying the mutation.
BRCA1 and BRCA2 are the two most common high-risk cancer-predisposing genes. Although the estimated prevalence in the general population is low (0.11% and 0.12%, respectively), carriers have an increased lifetime risk of breast cancer and associated earlier age at onset. From two metaanalyses based on retrospective studies, the estimated cumulative risk of breast cancer by the age of 70 vary from 57% (95% confidence interval (CI) 47–66) to 65% (95% CI 44–78) in women with a BRCA1 mutation and from 45% (95% CI 31–56) to 49% (95% CI 40–57) in women with a BRCA2 mutation. These estimated breast cancer risks were confirmed in a prospective study, and vary by type and location of BRCA1/2 mutations, as well as by methods of risk estimation.
Women with high familial risk
Women with a suspected genetic predisposition include women who have a strong family history of breast cancer or with a family history of ovarian cancer without a proven mutation. These women are at increased risk of breast cancer and are referred to as women at familial risk for breast cancer. Though there is no single definition of strong family history of breast cancer, generally accepted criteria include: (1) at least three breast and/or ovarian cancer cases from the same side in a family (first or second degree relatives); or (2) two breast cancer cases diagnosed before the age of 40; or (3) a family member with both breast and ovarian cancer; (4) two breast cancer cases in first degree relatives, with at least one case diagnosed before age 50; (5) any male relative with breast cancer; and (6) Ashkenazi Jewish ancestry with a family member with breast cancer, particularly triple-negative breast cancer diagnosed before age 60.
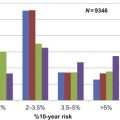
Risk assessment tools are designed to identify women at risk of carrying a mutation in a high-risk gene or to identify the risk of developing breast cancer during their lifetime with or without such a mutation. A recent study concluded that for current clinical practice, the IBIS (or Tyrer-Cuzick) model based on the International Breast Intervention Study and the Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA) models are the most accurate for assessing the risk of breast cancer. BOADICEA is used to compute BRCA1/2 mutation carrier probabilities and age-specific risks of breast and ovarian cancer. However, there is much variation between countries in the use of these risk assessment tools as well as in the applied thresholds for recommending testing or screening.
Characteristics of BRCA -Associated Breast Cancers Related to Screening
Several studies observed differences in the pathology of BRCA1/2 associated breast tumors as compared to non- BRCA- associated breast tumors. In general, BRCA1/2 associated breast tumors more frequently are estrogen and progesterone receptor positive, where BRCA2 -related tumors are more likely to have a lobular morphology and BRCA1 -related tumors a medullary carcinoma morphology. In general, women with a BRCA1/2 mutation have a significantly faster growth rate of their tumors than women with sporadic breast cancer. It is likely that this faster tumor growth rate in BRCA mutation carriers is due to a combined effect of having a BRCA mutation and the relatively young age at cancer diagnosis, where this effect is more pronounced in BRCA1 than in BRCA2 . In addition, the mean preclinical duration in BRCA1 mutation carriers is supposed to be shorter than in BRCA2 mutation carriers.
Screening Women With Known or Suspected Gene Mutation
Because screening mammography has been shown to be effective in reducing breast cancer mortality, screening for breast cancer is applied widely in many countries either through a national screening program or through clinical guidelines for average risk women, usually starting between the ages of 40 and 50 with intervals of 1–3 years. Women with known or suspected gene mutations have an increased lifetime breast cancer risk with an earlier age of onset, therefore, much attention has been focused on effective screening of this high-risk population. Although mammography screening is effective in the early detection of breast cancer in average risk women, its sensitivity to detect breast cancer in this high-risk group is much lower. Therefore, most studies have examined the sensitivity of the addition of screening tests to mammography for screening of younger women with known or suspected gene mutation using a nonrandomized design. Recent evidence from prospective cohort studies suggest that women at high risk for breast cancer benefit from screening, which includes breast MRI in addition to mammography, at an earlier age and shorter intervals than usually recommended for population screening. Although MRI with mammography is more sensitive than mammography alone, its specificity is lower, leading to false-positives and unnecessary tests. Further, repeated screening of young women with mammography annually before the age of 40 may increase the risk of breast cancer due to radiation exposure. To minimize the risk of radiation-induced cancer in young women, some guidelines recommend starting screening with MRI alone at the age of 25, while delaying screening with mammography until the age of 30. The decision on what age to start screening with mammography, therefore, should consider both the benefit of early detection and the potential harm of false-positives and increased risk of radiation-induced cancer.
Effectiveness of Screening Women With a Known or Suspected Gene Mutation
International collaborative groups have published guidelines for the managing and surveillance of women at high risk for breast cancer, often based on experts’ opinion. Preventive options for these women include risk-reducing mastectomy, salpingo-oophorectomy or use of tamoxifen. Although prophylactic mastectomy offers the greatest reduction in breast cancer risk, an international comparison of the uptake of this preventive option found that the minority of women opt for this. Therefore, it is important to identify in addition an acceptable and effective screening strategy. Many prospective cohort studies have been conducted examining the effectiveness of breast cancer screening in this high-risk population that includes MRI of the breast in addition to mammography. This section summarizes the evidence on the effectiveness of screening with MRI as an adjunct to mammography as compared to mammography-only in women with BRCA gene mutations and women at familial risk for breast cancer. The effectiveness of screening strategies is summarized in terms of expected benefits, such as improved cancer detection, the potential reduction in breast cancer mortality, cost-effectiveness of screening strategies, and the potential harms such as false-positives and false-negatives and radiation-induced tumor risk.
The literature was searched for studies reporting on screening for breast cancer in high-risk women from 1990 to 2015, to identify and summarize relevant evidence on this issue. Women were considered to have a high-risk of developing breast cancer if they had a BRCA1 or a BRCA2 mutation, or had a high familial risk without a known gene mutation. In a study setting, MRI and mammography had to be performed prospectively and simultaneously and these two tests had to be read independently of each other. In a real-world screening setting, MRI and mammography are not interpreted independently of each other. Prospective and model-based studies included are those that reported the screening sensitivity and specificity of MRI and mammography or related data from which sensitivity and specificity could be derived; those that examined survival or mortality rate; and those that compared cost-effectiveness of screening strategies.
Increased Sensitivity of Screening MRI as an Adjunct to Mammography
Evidence from prospective studies and metaanalyses
Fourteen prospective cohort studies including seven single center and seven multicenter studies were published through 2015 (see Table 11.1 ). These studies report sensitivity, specificity, and cancer yield (how many additional cancers detected by each screening modality) of screening modalities in a high-risk population.
| Author, Year, Study/Time Frame | Study Design/Reading Policy | Positive Test | Follow-Up and Intermediate Tests | Risk Category | Total ( n ) | Breast Cancers ( n ) | MRI Sens–Spec (%) | Mammography Sens–Spec (%) | Ultrasound Sens–Spec (%) | MRI+Mammography Sens–Spec (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Prospective Studies Including Annual MRI and Mammography Simultaneously | ||||||||||
| Passaperuma et al. (2012) Toronto-Canada 11/1997−6/2009 | Single center study/Single reading | BI-RADS 0,3,4,5 | Positive test: Biopsy. If MRI is positive but no other tests are, MRI is repeated within 1 month Intermediate test: (BI-RADS 3) 6,12,24-month follow-up | Total | 496 | 57 | 86–90 | 19–97 | NA | NA |
| BRCA1 | 267 | 31 | 90–NA | 19–NA | NA | NA | ||||
| BRCA2 | 229 | 26 | 80–NA | 20–NA | NA | NA | ||||
| Familial risk | 0 | 0 | NA | NA | NA | NA | ||||
| Sardanelli et al. (2011) Italy HIBCRIT 1 Study 6/2000–1/2007 | Multicenter study/Single reading | BI-RADS 4,5 | Positive test: Biopsy Negative test: 12-month follow-up Intermediate test: (BI-RADS 3) 4-month follow-up | Total | 501 | 52 | 91.3–96.7 | 50–99 | 52–98.4 | NA |
| BRCA1 | 184 | 21 | NA | NA | NA | NA | ||||
| BRCA2 | 146 | 10 | NA | NA | NA | NA | ||||
| Familial risk | 171 | 21 | NA | NA | NA | NA | ||||
| Leach et al. (2005) UK MARIBS 8/1997–5/2004 | Multicenter study/Double reading | BI-RADS 0,3,4,5 | Positive test: Biopsy Negative test: 12-month follow-up No intermediate test | Total | 649 | 35 | 77–81 | 40–93 | NA | 94–77 |
| BRCA1 | 82 | 13 | 92–79 | 23–92 | NA | 92–74 | ||||
| BRCA2 | 43 | 12 | 58–82 | 50–94 | NA | 92–78 | ||||
| Familial risk | 524 | 10 | NA | NA | NA | NA | ||||
| Riedl et al. (2015) Austria 1/1999–7/2006 | Single center study/Single reading | BI-RADS 4,5 | Positive test: Biopsy Negative test: Follow-up till the last round Intermediate test: (BI-RADS 3) 6-month follow-up | Total | 559 | 40 | 85.7–92.3 | 37.5–97.1 | 37.5–96.9 | 95–88.2 |
| BRCA1/2 | 156 | 16 | 81.3–94.3 | 43.8–98.9 | 37.5–99.1 | 87.5–NA | ||||
| Familial risk | 297 | 24 | 95.8–NA | 33.3–NA | 37.5–NA | 100–NA | ||||
| Rijnsburger (2010) The Netherlands MRISC 11/1999–3/2006 | Multicenter study/Single reading | BI-RADS 0,3,4,5 | Positive test: Biopsy Negative test: If imaging test was negative and CBE was suspect, additional test was required Intermediate test: (BI-RADS 0,3) US w/wo fine needle aspiration or imaging test | Total | 2157 | 97 | 70.7–89.7 | 41.3 | NA | |
| BRCA1 | 422 | 35 | 66.7–91 | 25–94.6 | NA | 70.8–NA | ||||
| BRCA2 | 172 | 18 | 69.2–91 | 61.5–93.8 | NA | 92.3–NA | ||||
| Familial risk | 1563 | 44 | 73–89.2 | 46–94.6 | NA | 89.2–NA | ||||
| Trop et al. (2010) Montreal-Canada 8/2003–5/2007 | Single center study/Single reading | BI-RADS 4,5 | Positive test: Biopsy Negative test: Follow-up till the last round Intermediate test: (BI-RADS 3) 6-month follow-up | Total | 184 | 12 | 83–93.6 | 58–95.4 | 42–93.8 | 100–NA |
| BRCA1 | 75 | 6 | 83.3–NA | 50–NA | 50–NA | NA | ||||
| BRCA2 | 68 | 5 | 80–NA | 60–NA | 20–NA | NA | ||||
| Familial risk | 41 | 1 | 100–NA | 100–NA | 100–NA | NA | ||||
| Lehman et al. (2005) USA 7/1999–1/2002 | Multicenter study/Single reading | BI-RADS 4,5 | Positive test: Biopsy | Total | 390 | 4 | 100–NA | 25–NA | NA | NA |
| Lehman et al. (2007) USA 11/2002–4/2003 | Multicenter study/Single reading | BI-RADS 3,4,5 | Positive test: Biopsy | Total | 190 | 6 | 100–NA | 66.7–NA | 16.7–NA | NA |
| BRCA1 | 41 | 2 | 100–NA | 0 | 0 | NA | ||||
| BRCA2 | 39 | 1 | 100–NA | 0 | 0 | NA | ||||
| Familial risk | 110 | 3 | 100–NA | 66.7–NA | 33.4–NA | NA | ||||
| Kuhl et al. (2005) Germany 3/1996–2/2002 | Single center study/Double reading | BI-RADS 4,5 | Positive test: Biopsy Negative test: Follow-up | Total | 529 | 43 | 90.7–NA | 32.6–NA | 39.5–NA | 93–NA |
| BRCA1/2 | 43 | 8 | 100–NA | 37.5–NA | 25–NA | 100–NA | ||||
| Familial risk | 486 | 35 | 88.6–NA | NA | NA | NA | ||||
| Kuhl et al. (2010) Germany 10/2002–12/2005 | Multicenter study/Single reading | BI-RADS 4,5 | Positive test: Biopsy Negative test: Follow-up | Total | 687 | 27 | 92.6–98.4 | 33.3–99.1 | 37–98 | 100–97.5 |
| BRCA1 | 53 | NA | NA | NA | NA | NA | ||||
| BRCA2 | 12 | NA | NA | NA | NA | NA | ||||
| Familial risk | 622 | NA | NA | NA | NA | NA | ||||
| Hagen et al. (2007) Norway 2002–01/2006 | Multicenter study/Single reading | BI-RADS 3,4,5 | Positive test: Biopsy Negative test: Follow-up till the last round Intermediate test: (BI-RADS 3) short term follow-up | Total | 491 | 21 | 86–NA | 48–NA | NA | 95.2–NA |
| BRCA1 | 445 | 19 | 84–NA | 53–NA | NA | 94.7–NA | ||||
| BRCA2 | 46 | 2 | 100–NA | 0–NA | NA | 100–NA | ||||
| Weinstein et al. (2009) USA 5/2002–7/2007 | Single center study/Single reading | BI-RADS 0,3,4,5 | Final conclusion made by consensus combining all results from different modalities. If all the tests gave suspicious finding, biopsy was performed | Total | 609 | 0.18 | 71–NA | 33 (FSM) | 17–88 | 95–NA |
| 39 (DM) | ||||||||||
| BRCA1 | 27 | 2 | 50–NA | 50 (FSM) | 0 | 100–NA | ||||
| 50 (DM) | ||||||||||
| BRCA2 | 17 | 2 | 0 | 100 (DM) | 0 | 100–NA | ||||
| Familial risk | 565 | 14 | 78.6–NA | 35.7 (DM) | 21–NA | 93–NA | ||||
| 35.7 (FSM) | ||||||||||
| Cortesi et al. (2006) Modena study, Italy 1/1994–9/2000 | Single center study/Single reading | Not specified | Total | 1325 | 36 | 100–NA | 78–NA | 50–NA | NA | |
| BRCA1/2 | 48 | 4 | 100–NA | 50–NA | 75–NA | NA | ||||
| High risk | 647 | 21 | NA | 90–NA | 52–NA | NA | ||||
| Intermediate risk | 257 | 8 | NA | 50–NA | 50–NA | NA | ||||
| Slightly increased | 346 | 3 | NA | 100–NA | 0 | NA | ||||
| Warner et al. (2004) Toronto, Canada 11/1997–3/2003 | Single center study/Single reading | BI-RADS 4,5 | Positive test: Biopsy If MRI is positive but no other tests are, MRI is repeated within 1 month Intermediate test: (BI-RADS 3) 6,12,24-month follow-up | BRCA1/2 | 236 | 22 | 77–NA | 36–NA | 33–NA | NA |
| Prospective Study on Additional Value of Ultrasound/Clinical Breast Examination to Screening | ||||||||||
| Bosse et al. (2014) 1/1997–10/2008 | Single-center study/Single reading | BI-RADS 4,5 | Positive test: Biopsy | Total | 221 | 27 | 100–55.5 | 27–82.3 | 81–84.2 | NA |
| Tilanus-Linthorst et al. (2000) 1/1994–4/1998 | Single-center study/Single reading | Not reported | Not reported | Women at high risk (>15%) | 678 | 50 | 8–NA* (only in subgroup of high risk over 25% risk underwent MRI) | 68–NA | 62–NA | NA |
| Metaanalysis of High-Risk Screening Studies | ||||||||||
| Included study | Study population | Test threshold | MRI+Mammography | Mammography | MRI | |||||
| Sens–Spec | Sens–Spec | Sens–Spec | ||||||||
| (%) (95% CI) | (%) (95% CI) | (%) (95% CI) | ||||||||
| Lord et al. (2007) | Kuhl et al. (2005) MARIBS study (2005) Lehman et al. HIBCRIT study 2006 (interim results) Warner et al. (2004) | Women with BRCA1/2 mutation and women at familial risk | 94 (86–98)–NA Incremental sensitivity: 58% (95% CI 47–70) | NA | NA | |||||
| Warner et al. (2008) | Kuhl et al. (2005) MRISC study (2004) Warner et al. (2001) Warner et al. (2004) Trecate et al. (2006) Hartman et al. (2004) Lehman et al. (2005) Lehman et al. (2007) Hagen et al. (2007) MARIBS study (2005) | Women with BRCA1/2 mutation and women at familial risk | BI-RADS 3,4,5 as positive | 94 (90–97)–77.2 (74.7–79.7) | 39 (37–41)–94.7 (93–96.5) | 77 (70–84)–86.3 (80.9–91.7) | ||||
| BI-RADS 4,5 as positive | 84 (70–797)–95.2 (93.7–96.6) | 32 (23–41)-98.5 (97.8–99.2) | 75 (62–88)–96.1 (94.8–97.4) | |||||||
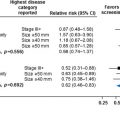
| Phi et al. (2015) | Montreal Canada study 2010 MARIBS study 2005 HIBCRIT study 2011 Austria study 2015 MRISC study 2010 Toronto Canada study 2012 | Women with BRCA1/2 mutation | BI-RADS 0,3,4,5 as positive | 93.4 (79.7–98.1)–80.3 (72.5–86.3) | 39.4 (30–49.7)–93.7 (88.8–96.5) | 85.3 (69.3–93.7)–84.7 (79–89.1) | ||||
| Roeke et al. (2014) | Tilanus-Linthorst (2000) Warner et al. (2001) Warner et al. (2004) MRISC study (2010) Kuhl CK et al. (2010) Montreal Canada study (2010) HIBCRIT study (2011) | Women with BRCA1/2 mutation and women at familial risk | NA | Cancer yield by clinical breast examination: 0–4% | NA | NA | ||||
Based on these studies, three metaanalyses have been performed ( Table 11.1 ). Two of the metaanalyses included screening studies in which women at high risk for breast cancer due to gene mutation or strong family history were included. The most recently published metaanalysis, consisting of individual patient data (IPD) from six large studies, reported data only on women with BRCA genes and it used a common categorization of screening test results.
Evidence in women with a BRCA1 or BRCA2 mutation
Overall, in women with a BRCA1 or a BRCA2 mutation, studies found low mammography sensitivity (the sensitivity ranged from 0% to 53%) and a much higher sensitivity of MRI (range 50–100%) in particular for MRI and mammography (range 70–100%) ( Table 11.1 ). The incremental sensitivity of MRI compared to mammography alone ranged from 40% to 100%. Sensitivity of mammography was higher in women with a BRCA2 mutation than in women with a BRCA1 mutation, possibly because of the higher proportion of Ductal Carcinoma in Situ (DCIS) in women with a BRCA2 mutation. Related to this, the incremental sensitivity of MRI was observed to be higher in women with a BRCA1 mutation than in women with a BRCA2 mutation, as MRI is less sensitive for DCIS.
The Lord et al. systematic review included five prospective studies with a total of 2059 women with a BRCA1/2 mutation or at high familial risk, reporting screening accuracy of the combination of MRI and mammography with or without breast ultrasound and clinical breast examination (CBE). A metaanalysis of the three studies that compared MRI and mammography versus mammography alone estimated a sensitivity of the combination of MRI and mammography of 94% (95% CI 86–98) and an incremental sensitivity of MRI as an adjunct to mammography of 58% (95% CI 47–70). The incremental sensitivity of MRI decreased when it was compared as an adjunct to mammography plus ultrasound or to the combination of mammography, ultrasound plus CBE. The main limitations of this review were that data for estimates of sensitivity and specificity of screening modalities were not reported, and that the pooled estimate was based on two different definitions of a positive screening test, which might result in biased estimates (one study used BI-RADS 0,3–5 as positive test and others used BI-RADS 4,5 as positive test).
The Warner et al. systematic review included 11 prospective studies with a total of 4983 women with a BRCA1/2 mutation or at high familial risk, reporting screening accuracy of MRI alone, mammography alone, and the combination if available. In this review, data were pooled for varying definitions of a positive test, and this showed that the sensitivity of screening modalities slightly decreased when the definition of a positive screening test was less strict. Using the stricter definition of BI-RADs scores of 4 and 5 considered to be positive, the sensitivity for mammography-only was 32% (95% CI 23–41) (based on seven studies, 4084 women), and the sensitivity for the combination of MRI and mammography was 84% (95% CI 70–97) (based on five studies, 1897 women), resulting in an incremental sensitivity for MRI of 52% (95% CI 42–62). The increase in sensitivity was traded off by a decrease in specificity from 98.5% of mammography-only, to 95.2% of the combination of MRI and mammography.
The Phi et al. metaanalysis consisting of IPD from six large prospective studies, and reported data on 1951 women with BRCA genes using a common categorization of screening test results. Considering a BI-RADS 3,4, or 5 as a positive test, the IPD estimated sensitivity of the combination of MRI and mammography was 93.4% (95% CI 80.2–98) and the incremental sensitivity of MRI was 53.8%, which is similar to the Warner et al. metaanalysis in 2008 (incremental sensitivity of 55%) when using the same cutoff point. In the general population, the sensitivity of mammography increases with increasing age and decreasing breast density. However, the IPD metaanalysis showed that mammography sensitivity was lower in women with a genetic mutation regardless of age (for women aged <50: 40% (95% CI 30.5–50.3) and for women older than 50: 38.1% (95% CI 22.4–56.7)), suggesting that screening with mammography alone would not be sufficient for these high-risk women over the age of 50. The evidence suggests that MRI continues to contribute to a high sensitivity in women with a BRCA1 or BRCA2 mutation older than 50 years old.
Evidence for women at high familial risk
The sensitivity and specificity of screening modalities were reported separately for women at high familial risk in a few studies. Women without a gene mutation, but at high familial risk for breast cancer, comprised varying proportions of the total study population in the studies (22.3–92.8%), as these women have a lower expected incidence of breast cancer, which is reflected by the small number of observed breast cancers ( Table 11.1 ). The reported sensitivity and specificity estimates are comparable to those for women with BRCA1/2 mutation in the few studies that had more than five breast cancer cases. However, as the observed incidence of breast cancer is lower in these women without a gene mutation, but at high familial risk for breast cancer, the positive predictive values of the screening will be lower and the negative predictive values will be higher than observed in the mutation carriers. Therefore, based on the trade-off of the lower positive and higher negative predictive values, the decision to add MRI to mammography in breast cancer screening may be different for this population. Further research is needed to strengthen the current evidence for this population on the added value of MRI to mammography in breast cancer screening.
Heterogeneity across studies
Due to the heterogeneity of methodology used, there are limitations when comparing results amongst the prospective studies evaluating the screening accuracy of MRI and mammography in high-risk women. First, these studies were conducted over different time periods, ranging from 1994 until 2011, during which the sensitivity and specificity of MRI may have improved. Second, the definition for a positive screening result was not consistent though all studies used BI-RADS assessments to classify the outcomes of screening. In some studies a positive screening test was defined as a BI-RADS 0,3,4,5, whereas in others a positive screening test was defined as BI-RADS 4, 5. Usually a BI-RADS 4 or 5 is followed by a biopsy. However, a BI-RADS 3 was either followed by additional imaging, within 4 months, or within 6 months. In one study, BI-RADS 0 also lead to additional testing. Third, the time between screening tests varied with screening modalities performed on the same day, within 1 month of each other, or 6 weeks to 3 months of each other. Fourth, some studies only included women with a BRCA1/2 mutation and others included women with BRCA mutations and with strong family history equivalent to a lifetime risk of breast cancer higher than 20%. This lifetime risk of breast cancer was defined and assessed by different risk assessment tools such as lifetime risk of being a carrier by BRCA PRO, or lifetime risk of developing breast cancer by the Gail or Claus model, or a study-specific risk model. Finally, inclusion criteria such as whether women with a personal history of breast cancer were excluded, or the age of recruitment differed between studies (age 35 ; age 25 ; or no specific age ).
Evidence from effectiveness studies evaluating screening program for high-risk women
Most of the prospective studies comparing MRI and mammography screening are efficacy studies in which annual MRI and mammography are performed simultaneously, and in which the results are blinded to ensure the comparison. There has been only one study of a real-world setting within a tailored screening program. A study from Ontario, Canada, reported first year results for the Ontario Breast Screening High Risk Program that offers annual MRI and mammography to women aged 30–69 years simultaneously but the results of both tests were not blinded. This study showed that no breast cancers were additionally detected by mammography and all the cancers were detected by MRI. The highest cancer detection (30.8/1000) was reported among women who were known gene mutation carriers.
Conclusions for cancer detection in women at high risk
Given the above evidence (summarized in Table 11.1 ), breast MRI screening as an adjunct to mammography improves the sensitivity of breast cancer detection in women with BRCA1/2 mutations, both in younger women and in women over the age of 50 years. For women without a BRCA mutation, the combination of MRI and mammography was also shown to be the most sensitive. However as the observed incidence of breast cancer is lower in these women without a gene mutation, the positive predictive values of the screening will be lower and the negative predictive values will be higher than observed in the mutation carriers. The evidence for women at familial risk is limited and does not consider different risk levels, and further research is needed to give more robust evidence in this particular population considering different risk levels. The prospective studies were heterogeneous in terms of methodology and study population and the aggregated metaanalyses were based on those studies. The most robust evidence comes from the IPD metaanalysis where the heterogeneity was minimized by using individual data from six studies, using common categorization of screening test results and women with similar risk profile.
The Role of Other Screening Modalities
Breast ultrasound
In addition to MRI and mammography, some studies included ultrasound (US) in their screening protocol. When US was performed annually with MRI and mammography, US alone had low sensitivity similar to mammography alone in women with or without BRCA mutation, ranging from 0% to 52% ( Table 11.1) . No breast cancers were detected by US only. In other settings, where US was offered semiannually, the sensitivity was 39.5–77%, and in one study three of 25 cancers were detected by US only, suggesting US as a screening modality every 6 months might help to detect more breast cancers. However, the cancer detection benefit should be balanced with the harm of screening, such as false-negative, and balanced with the cost per additional cancer detected.
Clinical breast examination
The contribution of CBE in screening women with or without BRCA mutation, was reviewed in a recent publication. The sensitivity of CBE ranged from 3% to 50% and the cancer yield of CBE was from 0% to 3% or 4% of the total breast cancers. The two studies reporting the contribution of CBE to be about 3–4% of the breast cancers had less screened detected breast cancers compared to other studies in which no additional breast cancers were detected by only CBE. Further, these two studies performed CBE semiannually compared to annually in the other studies. Another study which was not included in the review reported that biannual CBE detected four intervals cancers. Therefore, the contribution of annual CBE in screening women at high risk for breast cancer did not improve breast cancer detection. However, semi-annual CBE was shown to have a small contribution to breast cancer detection, though the evidence is very limited. It is important to balance the benefit with the harm of screening, as the price for detecting more breast cancer should be acceptable.
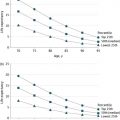
Potential Mortality Benefits of Screening With MRI
Early stage breast cancers are expected to have a better prognosis and to have an improved survival rate. The main goal of breast cancer screening is therefore to increase the rate of early stage tumor detection and to reduce mortality. To evaluate the mortality benefit of screening, there is a need for data derived from prospective studies including a control group with a long-term follow-up and for model-based studies, estimating survival rate due to screening with MRI and mammography as compared to no screening or mammography-only screening. In this section, results are reported from prospective studies that include a control group and from a model-based study using populations from prospective studies which estimated survival rates due to screening with MRI and mammography ( Table 11.2 ). The prospective studies either performed MRI and mammography in a study setting where the results of two tests were blinded (the MRISC study) or in a daily practice setting where the results of the test were not blinded (the Norway and UK study).