Salivary Gland-like Carcinomas
Primary salivary gland tumors of the lung are extremely rare, usually slow-growing, low-grade neoplasms that make up only 0.1% to 0.2% of all lung cancers.1 They originate from the submucosal glands of the tracheobronchial tree, and therefore, clinical signs and symptoms are related to endobronchial growth of these tumors. They have similar morphology and genetic abnormalities as their salivary gland counterparts. Patients with salivary gland lung tumors are often younger than other bronchogenic carcinoma patients and up to 40% of patients are nonsmokers. Only small case series about presentation, diagnosis, and management of these tumors have been reported in literature. The recommended treatment is complete surgical resection. The most important differential diagnosis is with a late metastasis from a head and neck salivary gland tumor. Since there are no morphologic criteria to distinguish between these two possibilities, a detailed clinical history should be obtained. Most frequently reported tumors include mucoepidermoid carcinoma (MEC), adenoid cystic carcinoma (ADC), and epithelial-myoepithelial carcinoma.2,3,4,5,6,7,8,9 and 10 Other salivary gland-like tumors have been rarely identified as primary lung tumors, including acinic cell carcinoma, pleomorphic adenoma, pneumocytic adenomyoepithelioma, and polymorphous low-grade adenocarcinomas.11,12,13,14,15,16 and 17
MUCOEPIDERMOID CARCINOMA
Pulmonary MECs are rare malignant neoplasms, making up fewer than 1% of primary lung neoplasms. Based on morphologic and cytologic features, tumors are divided into low- and high-grade subtypes. The prognosis of MUC depends on the tumor grade, clinical stage, and completeness of surgical resection. Low-grade tumors have excellent prognosis, whereas high-grade tumors tend to behave similarly to non-small cell lung carcinomas.
Mucoepidermoid Carcinoma, Cytology
MEC is not typically diagnosed cytologically; however, cytology may show bland glandular cells, squamoid cells, and goblet cells.
Mucoepidermoid Carcinoma, Gross Features
MECs usually present as sessile, polypoid, or pedunculated masses. They are generally centrally located, arising in the large airways and ranging in size from approximately 0.5 to 6 cm (Fig. 16-1).7 High-grade lesions frequently show infiltrative growth patterns. The cut surface is gray-white-tan in color, frequently with cystic change and a mucoid appearance.
Mucoepidermoid Carcinoma, Histology
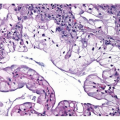
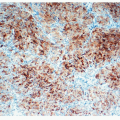
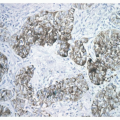
MEC is composed of three cell types including mucus-secreting, squamous, and intermediate cells. The relative proportion of each component is one of the criteria for histologic grading. Necrosis, nuclear pleomorphism, mitoses, and solid or nested growth patterns for the intermediate or squamous cells are commonly used criteria. Low-grade tumors predominantly show cystic changes admixed with solid areas ( Figs. 16-2,16-3 and 16-4). Cystic areas are lined by cytologically bland columnar, goblet, cuboidal, clear or oncocytic-appearing mucin-producing cells. High-grade
tumors show predominance of solid areas ( Figs. 16-5,16-6 and 16-7). Keratin pearls are not seen. The stroma is usually edematous, with hyalinization, calcification, ossification, and granulomatous reactions, adjacent to areas of mucus extravasation.
tumors show predominance of solid areas ( Figs. 16-5,16-6 and 16-7). Keratin pearls are not seen. The stroma is usually edematous, with hyalinization, calcification, ossification, and granulomatous reactions, adjacent to areas of mucus extravasation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree