(1)
Department of Radiation Oncology, University of Michigan Health System, 1500 East Medical Center Drive, 48109 Ann Arbor, MI, USA
Keywords
DCISMastectomyRadiationLocal recurrenceBreast cancerDecision makingRadiation side effectsMargin statusBackground
As discussed in other chapters in this book, radiation therapy in the adjuvant setting plays an important role in the management of patients with ductal carcinoma in situ (DCIS). Multiple previous studies have established the role of postoperative radiotherapy at reducing the risk of local recurrence after breast-conserving surgery [1–3]. There exist, however, limited data for the role of postmastectomy radiation in women with DCIS, and much of the rationale for postmastectomy radiation in the few DCIS patients who receive this treatment is extrapolated from experiences in women with invasive disease treated surgically with mastectomy.
Even within the context of invasive disease, however, the indications for postmastectomy radiation remain somewhat controversial. The rationale for radiation treatment in this setting, as in the adjuvant treatment of invasive breast cancer after lumpectomy, is to not only mitigate the potential of disease recurrence from disease reservoirs within the chest wall and regional lymphatics but also to eliminate any microscopic disease that might serve as the nidus for distant metastasis. For patients with DCIS, in whom adjuvant treatment after lumpectomy is primarily pursued for local control, the rationale for postmastectomy radiotherapy is similarly more restricted with local control as the primary aim. In both settings, to ensure net benefit from treatment, one must begin by identifying which patients have significant risk of harboring residual microscopic disease that might be eradicated by radiotherapy. The adequate and appropriate identification of patients who are at significant risk of harboring such microscopic disease, however, remains an area of controversy.
In this chapter, we begin by reviewing the role of postmastectomy radiation for invasive breast cancer, including the randomized trials that have established its role in the management of node-positive patients and the retrospective studies that have sought to identify subgroups of node-negative patients who also might benefit. The chapter describes the studies that identified surgical margin status as a risk factor for locoregional recurrence in node-negative patients with invasive cancer. It then proceeds to discuss in detail the few retrospective studies that have explored risk factors for local recurrence after mastectomy for DCIS. Because many of these studies have considered margin status as a risk factor, it reflects on the challenges of margin assessment before reflecting briefly on the limited data regarding outcomes in patients with DCIS treated with postmastectomy radiotherapy. Finally, treatment techniques and expected toxicities in this setting, again extrapolating from the much larger experience in the invasive cancer setting, are summarized. Ultimately, the chapter concludes that the decision regarding postmastectomy radiotherapy in patients with DCIS is challenging, given the limited data available, but that through extrapolation from existing studies, physicians may guide patients to make appropriate choices that reflect their personal values and preferences in this setting.
The Role of Postmastectomy Radiation for Invasive Breast Cancer
Before discussing the more limited role of postmastectomy radiation therapy for DCIS, it is important to examine the rationale and experience in the more common setting of invasive disease . Initial randomized trials evaluating the efficacy of postmastectomy radiation in women with invasive breast cancer were limited by increased toxicity and late complications associated with more primitive radiation techniques. Those early studies clearly showed an improvement in locoregional control with the administration of postoperative radiotherapy, but this did not translate into an overall survival benefit given the higher rates of noncancer-related mortality likely associated with the side effects of radiation treatment techniques that, at the time, did not spare the dose to surrounding critical structures including the heart and lungs [4–6]. This, coupled with the lack of effective systemic treatments at the time, meant that effective locoregional control of disease was not translated into an overall survival benefit [1, 7–12]. Despite the limitations to the early postmastectomy radiation trials in women with invasive breast cancer, subsequent trials in a more modern era that incorporated increasingly sophisticated radiation treatment techniques and effective systemic therapies have shown both a locoregional disease control benefit as well as a survival benefit for appropriately selected patients [13, 14]. These trials, which included primarily lymph-node-positive patients as well as locally advanced, lymph-node-negative patients, provide the evidence upon which current recommendations and guidelines are based [1, 2, 15] .
One such study, from investigators in Denmark, evaluated the role of postmastectomy radiation in premenopausal women with invasive breast cancer and clearly demonstrated a substantial reduction on locoregional recurrences (from 32 to 9 % at 10 years) and an overall survival benefit at 10 years of 10 % (from 45 % with no radiation to 54 % with radiation, P-value < 0.001) [16]. Perhaps just as importantly, analysis of the patients and tumor characteristics in this study identified risk factors associated with local recurrence and overall survival that remain foundational to the current indications for postmastectomy radiation in the invasive disease settings. In this study, multivariate analysis identified tumor size, number of involved lymph nodes, grade, age, and the use of radiation therapy as all being significantly associated with, and independent predictors of, outcome in these patients [16]. Subsequent analysis of the data failed to show a difference in survival in patients with left-sided versus right-sided disease and there was no excess risk of ischemic heart disease or death in irradiated versus nonirradiated patients [17]. Thus, in an era of more sophisticated radiation treatment techniques, the abrogation of a survival benefit seen in previous trials was lost once radiation treatment techniques were adapted to limit heart and lung toxicity .
Another trial from the Danish group, this time in postmenopausal women, also not only demonstrated a locoregional disease control benefit, with local recurrences at 10 years reduced from 35 % without radiation to 8 % with radiation, but also confirmed an absolute overall survival benefit at 10 years of 9 % (from 36 to 45 %, P-value 0.03) [18]. A similarly designed Canadian study in postmenopausal women also showed a 20-year survival advantage with the administration of postmastectomy radiotherapy [19]. Perhaps most compellingly, the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) published meta-analyses that demonstrated the benefit of local control with adjuvant radiation therapy after mastectomy [3]. In this meta-analysis in more than 8000 women who underwent mastectomy and axillary clearance for lymph-node-positive disease, the 5-year local recurrence risk was reduced by the addition of adjuvant radiation from 22.8 to 5.8 % with an associated reduction in 15-year breast cancer mortality risk of 5.4 % (from 60.1 to 54.7 %). Additionally, there was a 4.4 % absolute overall survival benefit at 15 years (from 59.8 to 64.2 %) which indicates that despite the technical limitations of the radiation treatment techniques at the time (and the associated cardiac and lung toxicity), postmastectomy radiotherapy for patients with lymph-node-positive disease provided a significant survival benefit. While the 2005 publication of the EBCTCG meta-analysis suggested a local control benefit for women with node-negative disease, subsequent updated analyses have not demonstrated a clear improvement of any end point, including local control, for women with node-negative breast cancer treated with mastectomy on these trials if restricted to the subgroup of patients who had complete axillary dissection [3, 13] .
These studies have established postmastectomy radiation as the standard of care for patients with invasive breast cancer and at least four positive lymph nodes. Given advances in systemic therapy and low rates of locoregional recurrence even without radiotherapy in selected patients in retrospective modern series, the role of postmastectomy radiation for patients with 1–3 positive lymph nodes is more controversial [20–22]. These studies also suggested that with more modern radiation techniques, postmastectomy radiotherapy can improve locoregional control without any adverse impact on survival. These findings led to increased interest in identifying additional patients, including those with node-negative invasive disease or DCIS, who may also benefit from postmastectomy radiation therapy under certain circumstances .
Patients with Node-Negative Invasive Cancer at Risk for Locoregional Recurrence
In addition to the postmastectomy patients with lymph-node-positive disease who clearly benefit from radiation in the adjuvant setting, there remain additional groups of women with invasive disease in whom postmastectomy radiation may be considered. The strongest evidence supporting the use of postmastectomy radiotherapy in node-negative invasive cancer patients has come from the Danish trials, which included patients with T3 and T4 node-negative disease. In those patients, locoregional recurrence was reduced from 17 to 3 % in premenopausal women and from 23 to 6 % in postmenopausal women [22]. Additionally, there was a survival advantage (from 70 to 82 %) in the premenopausal women [22] with the addition of postmastectomy radiation in node-negative invasive breast cancer with large primary tumors. However, this impact was not observed in the Oxford EBCTCG meta-analysis of the impact of postmastectomy radiotherapy in node-negative patients who received mastectomy and axillary dissection [13]. Moreover, retrospective analyses of patients with T3N0 disease have suggested that the risk of locoregional recurrence may be relatively low, and additional selection criteria may be necessary in order to identify a population of node-negative patients who really do have sufficient risk of locoregional recurrence to merit postmastectomy radiotherapy [23, 24].
Several retrospective studies have sought to further explore locoregional recurrence risks in patients with node-negative disease who undergo mastectomy. Such studies have identified possible additional risk factors for locoregional recurrence in lymph-node-negative patients who underwent mastectomy that may have implications in the setting of DCIS. These include young patient age, large tumor size, high nuclear grade, triple negative subtype, and close or positive surgical margins [25–28]. Of greatest relevance when considering patients with DCIS may be those studies which identified close or positive surgical margins as a possible indication for postmastectomy radiotherapy in node-negative invasive cancer [23].
Surgical margins in particular have received much recent attention. Initial indications regarding the effect of margin status on postmastectomy recurrence in women with invasive breast cancer comes from data from British Columbia. In this study, there was a higher likelihood of recurrence in early-stage patients treated with mastectomy with positive surgical margins that was age dependent (all recurrences were in women less than 50 years old) [25]. Additional data from investigators at Harvard suggested that close margins, T2 or larger tumors, premenopausal status, and lymphovascular invasion (LVI) put patients at higher risk for locoregional recurrences, and these patients may benefit from postmastectomy radiation [28]. These older studies, however, included patients treated before the advent of more sophisticated approaches to systemic therapy that may themselves reduce locoregional recurrence risk. In a more recent series from Boston, risks in invasive cancer patients with positive margins were higher than in those with close or negative margins, but considerably lower than in older studies; locoregional recurrence rates at 5 years increased from 1.9 % for women with negative margins to 6 % in women with margin-positive disease [29]. Women with close margins (< 2 mm) had a 1.5 % risk of locoregional recurrence at 5 years [29].
Rates of Local Recurrence After Mastectomy for DCIS
There exist no prospectively designed, randomized controlled studies evaluating postmastectomy radiation in women with DCIS . Thus, decisions in this setting must rely upon the much weaker rationale afforded by extrapolation from other sources of evidence. First, as discussed in detail elsewhere in this book, there is robust evidence from randomized trials that radiation therapy can reduce the risk of local recurrence of DCIS after breast-conserving surgery (with a relative risk reduction of approximately 50 %), without any observed impact on survival . Because the relative risk reductions afforded by radiotherapy after breast-conserving surgery and after mastectomy are similar for patients with invasive disease, one might extrapolate to infer that radiotherapy roughly halves the risk of local recurrence in DCIS patients regardless of surgery type. Some patients with DCIS, albeit few, do recur locally after mastectomy. If we could identify a subgroup of patients at sufficiently high risk of such recurrence, it might be reasonable to consider postmastectomy radiotherapy in that group .
Retrospective, single institutional studies provide some insight into the types of patients and disease characteristics associated with higher rates of local recurrence among patients with DCIS treated with mastectomy. One of the earliest of these studies evaluated women treated with mastectomy for DCIS between 1994 and 2002 [30]. In this series of patients from the Southern California Permanente group, a total of 574 women were identified as having undergone mastectomy for pure DCIS. Of these women, a total of 84 patients (18 %) were identified as having resections with close (< 10 mm) or positive margins after mastectomy, with 80 of the 84 women having not received postmastectomy radiation. This 80-patient cohort was then further analyzed to evaluate the risk and patterns of recurrence as well as the impact of local therapy on survival. Of the 80 samples, 47 (59%) had high-grade DCIS, 45/80 (56 %) samples had evidence of comedonecrosis, and 30/80 (38 %) samples had multifocal disease. The median follow-up time of patients in the study was 61 months and the majority (51/80) of patients were younger than 60 years of age. The overall rate of local recurrence in these patients was 7.5 %, with a 16 % (5/31) local recurrence rate in those patients whose resection margins were ≤ 2 mm. In the 49 patients with a margin > 2 mm, the recurrence rate was only 2 % (1/49). The majority of patients (5/6) with local recurrence had high-grade disease and/or comedonecrosis. The authors concluded that patients with surgical margins ≤ 2 mm have a greater-than-expected risk of local recurrence, and that this, coupled with other unfavorable features (like high-grade disease, comedonecrosis, or young age), may be indications for postmastectomy radiation [30] .
A subsequent study published a few years later from investigators at the University of California San Francisco identified 155 patients with pure DCIS who were surgically managed with mastectomy [31]. Of those 155 patients, 55 were found to have close surgical margins (< 5 mm) and 4 patients had truly positive surgical margins. With a median follow-up of 8 years, only one local recurrence (2 %) was noted in these 59 patients and it occurred in a patient with < 5 mm close margins and grade 3 disease after skin-sparing mastectomy. Contrary to the conclusions drawn by the Southern California Permanente group, these authors concluded that the risk of a chest wall recurrence was low enough not to warrant postmastectomy radiation therapy. Given the very few patients with margin-positive disease, they could not make any recommendations for patients in this population [31] .
A more recent series from a group at Harvard evaluated 142 consecutive patients who underwent mastectomy without adjuvant radiation for pure DCIS between 1998 and 2005. Of these 142 patients, 23 patients (16 %) had close margins (≤ 2 mm) and 21 patients (15 %) had frankly positive margins [32]. With a median follow-up time of 7.6 years (range 0.6–13.0 years), there were only two (1.2 %) chest wall recurrences. The rate of recurrence for patients with close margins was 4.3 % (1/23 patients), 4.8 % (1/21) in patients with positive margins, and 0 % (0/98) in patients with negative surgical margins. Like previous investigators, the authors concluded that mastectomy for pure DCIS results in a very low rate of local recurrences and that even in the setting of close or positive margins, postmastectomy radiation is not warranted [32] .
Additional data evaluating the rates of local recurrence after mastectomy for patients with DCIS come from investigators at Beth Israel Medical Center in New York [33]. In this retrospective study of a prospective database from 1997–2007, 207 patients with DCIS who underwent mastectomy were identified. With a median follow-up of 55 months (< 5 years), the 10-year relapse-free survival rate was 97 %. The majority of the patients were more than 45 years old with a mixture of ethnic backgrounds and an equal distribution of grade II and III disease. Final margins were negative in 88.6 % of patients but were close (< 1 mm) in 9 % and positive in 2.4 %. In this cohort, there were only two recurrences in the 207 patients (0.9 %) and they were both in patients with < 1 mm final surgical margins. Given the extremely low rate of local recurrence, there was a statistical inability to identify factors associated with local recurrence, though it is interesting that both recurrences were in patients with close, yet not positive, margins. The authors conclude that the use of postmastectomy radiation is unnecessary for patients with DCIS treated with mastectomy as the rates of local recurrence are diminishingly small .
Finally, investigators in British Columbia examined a large, population-based cohort of women to determine the risk factors associated with local recurrence after mastectomy [34]. They identified 637 patients with pure DCIS treated with mastectomy between 1990 and 1999 and with a median follow-up time of 12.0 years, the 10-year local recurrence rate was 1 % with breast-cancer-specific survival of 98.0 %. The majority of the patients in this cohort had high-grade disease (grade III, 42.5 %) with 87.1 % of patients having negative margins, 4.9 % with positive margins, and 5.5 % with close (< 2 mm) margins. In this population-based cohort they identified 12 local recurrences in the chest wall, with 11/12 recurrences being invasive disease, not DCIS. All 12 patients were successfully salvaged after recurrence, and the only factor found to be associated with increased rates of local recurrence was very young age (< 40 years, LRR 7.5 % vs. 1.5 %, P = 0.003). As with the previous groups, the authors conclude that mastectomy provides excellent locoregional control for DCIS and that the routine use of postmastectomy radiation therapy, even in young patients (< 40 years old), is not justified [34] .
Some have questioned whether the technique and degree of mastectomy influences the rate of local recurrence. In a series evaluating the rate of local recurrence after skin-sparing mastectomy, 223 patients were identified as having received skin-sparing mastectomy with immediate reconstruction without adjuvant radiation for pure DCIS [35]. With a mean follow-up of 6.9 years (range 0.4–10.3 years), the total recurrence rate was 5.1 % (11 patients) with local recurrences comprising the majority of the recurrences (3.3 % with 7/223 patients developing local-only recurrence). The authors did find that the rate of local recurrence was 10.5 % (2/19) in patients with close surgical margins of ≤ 1 mm. Age, size > 4 cm, tumor necrosis, and type of biopsy were not significantly associated with risk of local recurrence, but high tumor grade was significantly associated with likelihood of recurrence (p = 0.02). These authors concluded that in patients with close surgical margins after skin-sparing mastectomy, re-excision or adjuvant radiation should be performed .
Thus, the literature to assess the risk of local recurrence in DCIS after mastectomy is relatively limited, with authors from different institutions documenting differences in experience and drawing conflicting conclusions. Differences in individual surgeons’ approaches may be particularly important in this setting but are highly difficult to evaluate .
Challenges of Assessing Margin Status
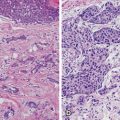
Given that much of the previously mentioned data consider the possible role of surgical margin status as a risk factor for local recurrence of DCIS after mastectomy, it is important to reflect on the additional challenges that arise with regard to the accuracy and reproducibility of margin assessment. Recent consensus guidelines published by the joint Society of Surgical Oncology-American Society for Radiation Oncology consensus panel have nicely summarized the challenges associated with accurately defining margin status [36]. While the consensus guidelines deal with appropriate margins governing the need for re-excision for invasive breast cancer, the challenges regarding margin assessment apply equally to patients with DCIS. One such challenge involves the processing of specimens after resection. Upon removal of the breast tissue, there is flattening of the specimen either from extrinsic compression of the sample or because of a lack of support from the surrounding tissue ex vivo. This leads to artificial narrowing of the margin and may falsely categorize as specimen having close or positive margins [37]. Further confounding of margin status occurs as superficially applied ink (either during surgery or during postsurgical sample pathologic processing) penetrates deeper into tissue, again artificially narrowing the margin. Methods of margin assessment may itself influence the rates of margin positivity, as data suggest that shaved margin assessment results in the categorization of many positive margins that would have been called negative by the inking method, thus leading to increased rates of re-excision and mastectomy [38]. Furthermore, margin status assessment is by necessity a highly selective process as true cell-by-cell assessment of the margin is impractical. Thus, random sampling of margin status is routinely performed but often only examines a tiny fraction of the total margin and thus may miss areas of close or positive margins [39]. Finally, margin status assessment is performed on fixed, inked, sectioned samples in two dimensions and clearly is unable to appreciate three-dimensional architecture. Thus, margin status on any given slide in two dimensions may not accurately reflect true margin status in three-dimensional space a few millimeters superficial or deep to the sectioned tissue. It is therefore important to consider these inherent limitations when examining the data regarding margin status postmastectomy for women with DCIS.
Outcomes After Radiation for DCIS Postmastectomy
As mentioned previously, there are no prospective, randomized data assessing the efficacy of postmastectomy radiation in women with DCIS . The limited data that do exist suggest that postmastectomy radiation is effective in controlling local disease with exceptionally low rates of local recurrence after postmastectomy radiation, even in women with positive surgical margins. The largest published series comes from investigators at the University of Pennsylvania who tracked the outcomes of 287 women treated with postmastectomy radiation between 1978 and 1992 [40]. Of these 287 women, 1 % (three patients) had DCIS and underwent mastectomy because of diffuse microcalcifications on screening mammography. All three women subsequently received postmastectomy radiation because of positive surgical margins after mastectomy. All patients were clinically node negative, and one of the women did undergo axillary lymph node dissection with 0 out of 10 lymph nodes positive. All women received between 42.75 and 50 Gy in 1.8–2.25 Gy daily fractions delivered to the chest wall (one with 1-cm bolus applied every other day) utilizing tangential fields without regional nodal irradiation. None of the patients received adjuvant endocrine or systemic chemotherapy . With a median follow-up time of 7.4 years (7.1–19.4 years), all patients were alive and disease-free with no evidence of local or distant recurrence. There were no contralateral breast events and the authors reported no significant long-term side effects. However, given the small numbers of patients with DCIS included, it is difficult to draw conclusions from these findings .
Treatment Indications/Current Consensus
Given the limited data regarding the role of postmastectomy radiation for DCIS, treatment guidelines have been developed based on institutional experience and have been borrowed from experience and principles gleaned from trials in the invasive cancer space. Indeed, data from multiple randomized trials involving thousands of patients are unequivocal in demonstrating that adjuvant radiation significantly decreases the rates of local recurrence after lumpectomy or mastectomy for invasive breast cancer and also significantly decreases local recurrence after lumpectomy for DCIS. More limited data also demonstrate excellent local control rates when adjuvant radiation is utilized in the postmastectomy setting, even for women with positive margins. The important unanswered question, however, is whether patients with close or positive surgical margins after mastectomy for DCIS are at sufficiently high risk to justify the use of the adjuvant postmastectomy radiation. As noted above, different retrospective series have generated widely varying estimates of risk in patients with DCIS who have close or positive margins after mastectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree