Abstract
This chapter discusses the incidence, classification, genetics, epidemiology, pathology, clinical features, diagnosis, staging, treatment, and posttreatment management of retinoblastoma.
Keywords
retinoblastoma, RBI gene, genetic counseling, chemotherapy, plaque radiotherapy, intra-arterial chemotherapy, intravitreal chemotherapy
Retinoblastoma (RB) is a malignant tumor of the embryonic retina. It affects young children, usually under the age of 5 years. Tumors may be unilateral or bilateral, unifocal or multifocal. There are hereditary and nonhereditary forms of the disease and the disease can be sporadic or familial. Intraocular growth occurs first, prior to invasion of structures within the globe or spread to metastatic sites. In developed nations, presentation with metastatic disease is unusual. However, metastatic disease is not uncommon in developing countries, where it is a significant cause of morbidity and mortality. RB is the paradigm for a genetically inherited cancer and provides the basis for Knudson’s two-hit hypothesis of carcinogenesis.
Incidence
- 1.
RB is the most common intraocular malignancy of childhood, occurring at a rate of approximately 1 in 20,000 live births.
- 2.
The annual incidence is 11 per million under 5 years of age.
- 3.
Approximately 200–300 new cases of RB occur each year in the United States.
- 4.
RB accounts for 11% of cancers developing in the first year of life, but for only 3% of all cancers diagnosed in children younger than 15 years of age.
- 5.
The median age at diagnosis is 2 years.
- 6.
Approximately 40% of cases are hereditary. The majority of these patients present with bilateral disease with an average of three tumors per eye and present in the first year of life. Of these, only 15% have an established family history of RB.
- 7.
The remaining 60% of cases are nonhereditary, most often presenting with unilateral and unifocal disease in the second and third years of life.
Classification
Laterality
Unilateral Tumors
Patients can have one or more tumors in one eye. Median age of presentation is 23 months, with few presenting under a year of age. Tumor development within the affected eye can be synchronous or metachronous. For those with unifocal unilateral disease, it is likely that these patients have the nonhereditary form of the disease. Patients with multifocal unilateral disease or those that present at a younger age are more likely to have the hereditary form of the disease.
Bilateral Tumors
Patients have one or more tumors in both eyes. Tumor development can be synchronous or metachronous. It is presumed that these patients have the hereditary form of the disease, even in the absence of a positive family history. These patients almost always present prior to age 2 years and most present in the first year of life. The severity of tumors may be variable in the two eyes, and this becomes important in weighing up potential treatment options.
Focality
If a single tumor focus exists, these tumors are more likely to be nonhereditary. In contrast, multiple tumor foci can be noted in one or both eyes. These patients are more likely to harbor a germline mutation in the RB1 gene.
Genetics
The Two-Hit Hypothesis
Knudson’s two-hit hypothesis proposes that as few as two stochastic events are required for tumor initiation. The first can be either germline or somatic and the second occurs somatically in the individual retinoblast cells.
The RB1 Gene
RB occurs as a result of mutations of the RB1 gene located on chromosome 13q14. This was the first tumor suppressor gene cloned. It spans 183 kilobases of genomic DNA, consisting of 27 exons, and coding for a 110-kd protein p110, with 928 amino acids. Regulation of transcription, and thus, cell proliferation are linked to the phosphorylation of the RB protein. Involved in this process are E2F1, a transcription factor that regulates the cell cycle during G1, histone deacetylase 1, and downstream cell cycle-specific kinases. Loss of function is the initiating event for RB. Mutations may be germline or somatic and there are a broad array of types and locations of mutations, ranging from single base changes to large deletions. No hot spots of common mutation have been identified.
Hereditary RB
A “two-hit” model has been proposed to explain the different clinical features of hereditary and nonhereditary cases of RB. These patients inherit a germline mutation in the RB1 gene that is present in every cell of the body. Eighty-five percent of these are new spontaneous mutations (sporadic), while the remaining 15% have a positive family history (familial). For the sporadic cases, the paternal allele is affected in approximately 94% of cases. Postconception, a second somatic mutation occurs in the remaining RB1 gene in one or more retinoblasts and tumor results. These cases are at risk of multifocal and bilateral tumors.
Nonhereditary RB
These patients inherit two normal copies of the RB1 gene. Postconception two somatic mutations occur, one in each copy of the RB1 gene in a retinoblast and tumor results. These cases are usually unifocal or unilateral tumors.
Genetic Counseling
The RB1 gene is inherited in an autosomal dominant fashion. Penetrance is high, at approximately 95%. Genetic counseling should be an integral part of the therapy for a patient with RB, whether unilateral or bilateral. Genetic counseling, however, is not always straightforward. A significant proportion (10–18%) of children with RB have somatic genetic mosaicism, making the genetic story more complex and contributing to the difficulty of genetic counseling.
Testing, including sequencing, duplication and deletion testing, MYCN copy number and promoter methylation analysis, is done on the tumor and then compared to somatic tissue (usually blood). If the globe is salvaged, then testing proceeds with a blood sample alone. Of note, in situations where the tumor is not available a negative peripheral blood test does not conclusively rule out that the patient has heritable RB, although it makes it significantly less likely. Environmental exposures associated with development of RB have been inconsistent in epidemiologic studies.
Prenatal Diagnosis and Further Genetic Counseling
With sequencing of the RB1 gene available, prenatal diagnosis can be undertaken, particularly if there is a family history and the mutation has been identified. However, a negative result cannot categorically rule out disease, as 100% of mutations are not picked up by current screening methods. The positive predictive value of screening, however, is rapidly improving.
13q Deletion Syndrome
This syndrome is associated with an increased risk of RB as 13q14 is the genomic location of the RB gene. Physical findings include microcephaly, a high forehead, short nose, hypertelorism, and micrognathia.
There are reports which correlate the size of the deletion with the degree of the attendant developmental delay, although this correlation can be inexact. Patients identified with this syndrome in the neonatal period should be sent to an oncologic ophthalmologist for serial ocular screenings.
Risk for Second Malignant Neoplasms
- 1.
As the RB1 gene is a tumor suppressor gene, individuals with heritable RB are at elevated risk for the development of second and subsequent malignancies.
- 2.
The most common second malignancies reported have been osteosarcoma, followed by soft tissue sarcomas and melanoma. Leukemia, lymphoma, and breast cancer are also reported in excess of that expected.
- 3.
The risk is highest for those children with the heritable form of the disease who are treated with full-dose, external beam radiotherapy delivered without use of conformal fields under the age of 12 months.
- 4.
The 40-year risk is approximately 35% for those treated with radiotherapy and 10% for those treated without radiotherapy.
- 5.
The risk for those patients with unilateral disease is approximately 5%, likely representative of the small fraction of genetic cases with only a single eye affected.
- 6.
For those who survive an second malignant neoplasm (SMN), the risk of developing yet another primary malignancy is about 2% per year.
- 7.
Approximately 60% of SMNs occur within the radiotherapy field, with the remainder occurring outside the field.
- 8.
Patients with RB should be counseled carefully regarding their increased risk of SMN and should be followed by routine clinical evaluation. Any signs or symptoms potentially referable to a SMN should be promptly evaluated. It is important to counsel against smoke exposure and in the proper use of sunscreen.
Pathology
Retinoblastoma
The tumor is composed mainly of undifferentiated anaplastic cells that arise from the nuclear layers of the retina. Histology shows similarity to other embryonal tumors of childhood, such as neuroblastoma and medulloblastoma, including features such as aggregation around blood vessels, necrosis, calcification, and Flexner–Wintersteiner rosettes. RBs are characterized by marked cell proliferation as evidenced by high mitosis counts. Tumors can undergo spontaneous regression.
Retinocytoma
This is a variant of RB referred to as either retinoma or retinocytoma. These tumors are composed of benign-appearing cells with a high degree of photoreceptor differentiation. Eyes with such tumors have normal vision. The main issue is that these tumors do not regress in the same way as RB, when treated with chemotherapy or local ophthalmic therapy. Thus, differentiating these benign variants from the malignant form of the tumor is essential, so unnecessary treatment is not employed.
Clinical Features
Presenting Signs and Symptoms
- 1.
Leukocoria.
- 2.
Strabismus.
- 3.
Decreased visual acuity.
- 4.
Inflammatory changes.
- 5.
Hyphema.
- 6.
Vitreous hemorrhage, resulting in a black pupil.
Differential Diagnosis
Pseudoretinoblastoma
The diagnosis of RB is made visually. There are multiple conditions that can mimic RB and in a review of almost 3000 patients referred to a major center with the diagnosis of RB, 22% had a simulating lesion referred to as pseudo RB. In children under the age of 2 years, these most commonly included persistent fetal vasculature (also termed persistent hyperplastic primary vitreous), Coats disease, and vitreous hemorrhage. Older children may have toxocariasis or familial exudative vitreoretinopathy.
Patterns of Spread
Intraocular
- 1.
With endophytic growth, there is a white hazy mass.
- 2.
With exophytic growth, there is retinal detachment.
- 3.
Most tumors have combined growth.
- 4.
Retinal cells frequently break off from the main mass and seed the vitreous, or new locations on the retina.
- 5.
Glaucoma may result from occlusion of the trabecular network or from iris neovascularization.
Extraocular
- 1.
RB spreads first to soft tissues surrounding the eye or invades the optic nerve. From there it can spread directly along the axons to the brain, or may cross into the subarachnoid space and spread via the cerebrospinal fluid to the brain.
- 2.
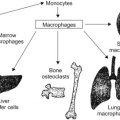
Hematogenous spread leads to metastatic disease, most commonly to brain, lungs, bone marrow, or bone.
- 3.
RB can spread lymphatically to the preauricular and submandibular nodes.
In patients with the genetic form of RB, central nervous system (CNS) disease is less likely the result of metastatic or regional spread than pineoblastoma, which is also termed trilateral RB.
Trilateral RB
Trilateral RB is a syndrome that occurs in children under the age of 5 years. It consists usually of bilateral hereditary RB associated with an intracranial neuroblastic tumor of the pineal gland, and occurs in less than 10% of children with familial, multifocal, or bilateral RB. With the onset of systemic neoadjuvant chemotherapy, the incidence of this syndrome is decreasing.
Diagnostic Procedures
Screening
All children should have screening performed as part of well-child check-ups, primarily by eliciting red reflexes in the eye. However, most cases of RB are diagnosed after a parent or other relative notices an abnormality of the eye and this prompts further evaluation.
Siblings of children with RB should be screened by ophthalmology at regular intervals at least through age 2 to 3 years unless their genetic testing has revealed they do not carry the RB1 gene mutation.
Diagnosis of Intraocular RB
Diagnosis is made by ophthalmologists, retinal specialists, or ocular oncologists using a combination of an ophthalmologic examination generally performed under sedation or anesthesia, together with retinal camera (RetCam) imaging, ultrasound, computed tomography, or magnetic resonance imaging (MRI). Calcification of the lesion(s) may be seen. Due to concern about rupturing the tumor and causing both intraocular and extraocular spread, surgical biopsies are not performed for confirmation.
Defining Extent of Disease
The ophthalmologic examination will determine the extent of intraocular tumor and presence or absence of orbital extension. It is crucial that intraocular examination with a binocular indirect ophthalmoscope be performed on both eyes with the pupils maximally dilated. The ophthalmologist should make diagrams of the retina to show the number, size, and location of all tumors. These diagrams are now being supplemented by the use of RetCam images, which are helpful in determining not only the extent of disease, but response to treatment. When the binocular indirect ophthalmoscope is used, the location of the tumor(s) should be related to specific landmarks such as the optic nerve head, fovea, and ora serrata. Size of the lesion is estimated by comparison with the optic nerve head diameter.
Extraocular Extent of the Disease
All children with RB should be referred to a pediatric oncologist for evaluation of extraocular disease.
Table 28.1 summarizes the investigations to be performed for diagnosis of RB.