Hepatocellular tumorlike lesions
Miscellaneous tumorlike lesions
Focal nodular hyperplasia
Mesenchymal hamartoma
Nodular regenerative hyperplasia
Inflammatory pseudotumor
Partial nodular transformation
Inflammatory myofibroblastic tumor
Precancerous lesions
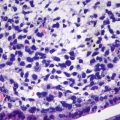
Pseudolymphoma
Compensatory hyperplasia
Pseudolipoma
Focal fatty change
Solitary necrotic nodules
Accessory lobe
Peliosis hepatis
Bile duct tumorlike lesions
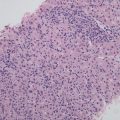
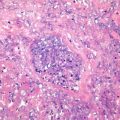
Sarcoidosis
Biliary hamartoma
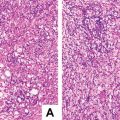
Nodular extramedullary hematopoiesis
Simple hepatic cysts
Cystic echinococcosis
Polycystic liver diseases
Liver abscess
Caroli disease
Malacoplakia
Congenital choledochal cyst
Ectopic tissues
Congenital hepatic fibrosis
Larva migrans
Ciliated hepatic foregut cyst
Hepatic infarction
Epidermoid cyst
Endometrial cyst
Peribiliary cysts
Cyst of the accessory liver
Alimentary duplication cyst
Biloma
Mesothelial cyst
Table 3.2
Histological types of benign tumors of hepatic and intrahepatic bile ducts
Hepatocellular tumors | Neurological and endocrinic tumors |
Hepatocellular adenoma | Neurilemmoma |
Hepatic adenomatosis | Neurofibroma |
Bile duct tumors | Plexiform neurofibroma |
Bile duct adenoma | Neurofibromatosis |
Biliary cystadenoma | Paraganglioma |
Intraductal papillary neoplasms of the bile ducts | Adrenal rest tumor |
Biliary adenofibroma | Pancreatic rest tumor |
Vascular and lymphatic tumors | Gastrinoma |
Cavernous hemangioma | Vasoactive intestinal peptide tumor |
Hemangioblastoma | Somatostatinoma |
Infantile hemangioendothelioma | Miscellaneous benign tumors |
Lymphangioma | Teratoma |
Lymphangiomatosis | Mesothelioma |
Muscular, fibrous, and adipose tumors | Myxoma |
Leiomyoma | Chondroma |
Solitary fibrous tumor | Langerhans cell histiocytosis |
Angioleiomyolipoma | Spongiotic pericytoma |
Lipoma | |
Myelolipoma |
Table 3.3
Histological types of malignant of hepatic and intrahepatic bile ducts
Hepatocellular tumors | Neurological and endocrinic tumors |
Hepatocellular carcinoma | Neuroendocrine neoplasms |
Fibrolamellar hepatocellular carcinoma | Malignant peripheral nerve sheath tumor |
Combined hepatocellular-cholangiocarcinoma | Miscellaneous malignant tumors |
Dual-phenotype hepatocellular carcinoma | Carcinosarcoma |
Hepatoblastoma | Yolk sac tumor |
Bile duct tumors | Chorioepithelioma |
Intrahepatic cholangiocarcinoma | Malignant teratoma |
Bile duct cystadenocarcinoma | Malignant rhabdoid tumor |
Mucin-producing intrahepatic cholangiocarcinoma | Gastrointestinal stromal tumors |
Special types of intrahepatic cholangiocarcinoma | Malignant melanoma |
Vascular and lymphatic tumors | Malignant mesothelioma |
Angiosarcoma | Synovial sarcoma |
Malignant hemangiopericytoma | Osteoclast-like giant cell tumors |
Epithelioid haemangioendothelioma | Desmoplastic small round cell tumor |
Kaposi sarcoma | Histocytic sarcoma |
Lymphoma | |
Follicular dendritic cell tumor | |
Extramedullary plasmacytoma | |
Muscular, fibrous, and adipose tumors | |
Leiomyosarcoma | |
Rhabdomyosarcoma | |
Fibrosarcoma | |
Liposarcoma | |
Malignant fibrous histiocytoma | |
Undifferentiated(embryonal) sarcoma | |
Myofibroblastic sarcoma | |
Osteosarcoma | |
Chondrosarcoma |
Under the leadership of Academician Meng-Chao Wu, we have made great progresses in the exploration of pathological diagnosis and molecular pathology of hepatobiliary tumors, resulting in the development from pathological group in the lab of hepatobiliary surgery to the Department of Pathology in a Grade A Tertiary Specialized Hospital of hepatobiliary surgery. The number of cases diagnosed in our Department of Pathology per year has gradually risen from less than one hundred, to several thousand, and to approximate ten thousand. Up to now, our Department has successfully applied and finished ten projects supported by the National Natural Science Foundation of China and several projects supported by the Army and Shanghai Municipal Foundations, including the training plan for 100 outstanding cross-century academic leaders of Shanghai health system and the fund for military outstanding young- and middle-aged experts of medical and health. We achieved the “Silver Star in Science and Technology” from PLA General Logistics Department, National Science and Technology Progress Award (third class), Medical Science and Technology Progress Award of PLA (second class, twice), Medical Achieve Awards of PLA (first class), Chinese Medical Science and Technology Awards (second class), Shanghai Science and Technology Awards (first class) and Shanghai Medical Science and Technology Awards (first class), and so forth. And we are also honored to have become one of the principal members of the Innovative Research Team Integrating Clinical and Basic Research of Liver Cancers of The Second Military Medical University, the National Science and Technology Progress Award of China in 2012, which was led by Academician Meng-Chao Wu and Academician Hong-Yang Wang in EHBH.
3.2 British Hepatopathologist Professor Anthony PP
Professor Anthony worked in the Department of Pathology of Royal Devon and Exeter Hospital, University of Exeter, and he took part in constructing WHO Histological Classification of Hepatic and Intrahepatic Bile Duct Tumors in 2002. Professor Anthony firstly suggested the concept of liver cell dysplasia (LCD) in 1973 [19] and defined it as the result of chronic integration of HBV in hepatic cells which is a premalignant lesion, and the patients with liver cirrhosis complicated by LCD are at significantly higher risks to develop HCC and should be followed up with serum AFP testing. The above important concepts are still very classic even today and remain to be the research focus. At the beginning of our research in pathology of hepatic carcinoma, we were faced with the question of how to observe and understand LCD; related articles written by Professor Anthony became our key reference and guidance, based on which we reported the findings that DNA ploidy and nuclear atypia index in LCD were between normal and hepatic cells and HCC cells in 1988 [20, 21], demonstrating abnormal proliferating cell populations at different stages of premalignant progression, consistent with the basic features of premalignant lesions. Later, we reported in situ hybridization and immunohistochemistry of HBV, AFP mRNA and P21, DNA content and nuclear atypia via image dissector in premalignant condition of liver cancer in the first National Youth Academic Conference held by Chinese Pathological Society, Chinese Medical Association in Xiamen City in November, 1991, and won the Outstanding Research Paper Awards. Thereafter, we kept on conducting the research in genomic instability and proteomic screening of diagnostic markers related to premalignant lesions, such as dysplastic nodules [22] and hepatocellular adenoma [23].
When we were planning to compile Surgical Diagnostic Pathology of Hepatobiliary Tumors, I wrote to Professor Anthony to consult him about premalignant lesions of liver cancers and invited him to participate in writing the book on December 2, 2001. Though he wrote back to say that he was not able to write related articles because he had already retired despite his identity as an emeritus professor and honorary advisor in pathology on December 19 of the same year, he showed great encouragement and provided a list of reference books to us. He believed the book would be very outstanding in the field due to its wide-range coverage and adequate pathological materials with proper utilization. Much to my surprise, he mentioned that he had paid an academic visit in Shanghai in 1983 when I just graduated and started to work in the SMMU, and I felt very pity that I hadn’t attend his lecture.
3.3 American Hepatopathologist Professor Anthony J. Demetris
Professor Demetris is the Director of the Division of Liver Transplantation Pathology of the University of Pittsburgh Medical Center (UPMC), Pennsylvania, USA, and the Director of Liver Steering Committee of International Banff Working Group on organ transplantation pathology. Professor Demetris took the lead in developing the well-adopted International Criteria for liver transplantation pathology including acute rejection activity index (RAI) [24], and he received the honorable title of Starzl Professor of Transplant Pathology, belonging to the working group led by Professor Thomas E. Starzl who successfully performed the world’s first liver transplantation. The first liver transplantation in our hospital was performed by Academician Meng-Chao Wu working group in 1978, and we reported the first pathological diagnosis of liver biopsy in 3 patients with posttransplantation complications in the Conference of diagnostic pathology of PLA in 1996. With more experience accumulated in liver transplantation pathodiagnosis, we realized much difference of theory and practice between liver transplantation pathodiagnosis and general surgical pathodiagnosis, and it was difficult for us to ensure the accuracy of each pathodiagnosis via liver biopsy due to the inadequate knowledge and training of liver transplantation pathodiagnosis. Hence, as a visiting scholar, I went to the Division of Liver Transplantation Pathology of Starzl Transplantation Institute in UPMC in 1999, which is one of the largest centers of organ transplantation in America. Pathodiagnosis of organ transplantations, mainly including the liver, kidney, heart, lung, small intestine, etc., was performed, and abundant data on transplantation pathology could be obtained in UPMC. Thanks to Professor Demetris’s meticulous and thoughtful arrangement for my study there, I learned a lot from Professor Demetris and other pathological experts, receiving much advice and guidance in transplantation pathology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree